Starting an antidepressant can feel like a lifeline - until your sleep falls apart. You might find yourself wide awake at 2 a.m., heart racing, mind spinning, even though you’ve been exhausted for weeks. This isn’t just stress. It’s a direct effect of the medication you’re taking to feel better. Up to 78% of people on SSRIs like fluoxetine or sertraline report new or worsening insomnia in the first two weeks. And it’s not just you - this happens to most people on these drugs, especially early on.
Why Antidepressants Mess With Your Sleep
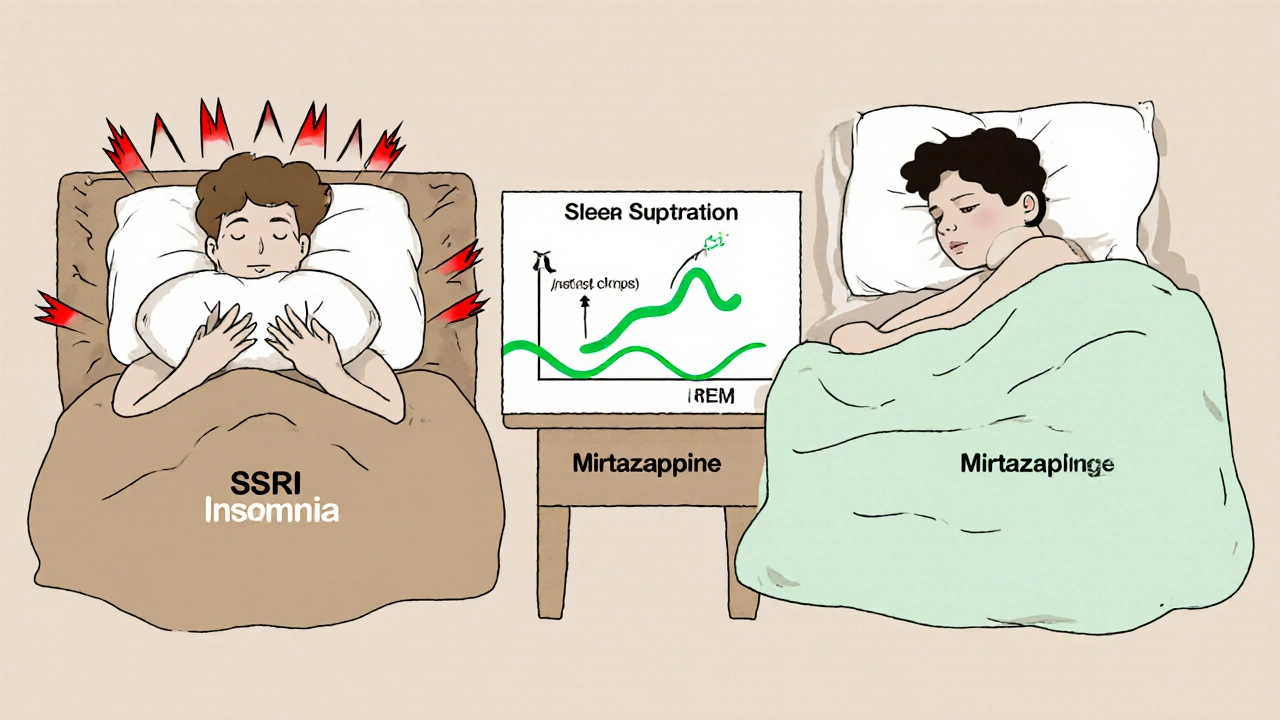
Antidepressants don’t just lift your mood. They change how your brain handles sleep chemicals - especially serotonin, norepinephrine, and dopamine. These aren’t just "feel-good" molecules. They’re the switches that turn sleep on and off. SSRIs, for example, suppress REM sleep by up to 29% and push back when you first enter REM by over an hour. That’s not a side effect - it’s the drug doing exactly what it’s designed to do. But your body doesn’t care about the science. It just knows you’re not sleeping.Tricyclics like amitriptyline do the opposite. They flood your system with sedating chemicals, increasing deep sleep by 22%. That’s why some doctors prescribe them for insomnia - even if depression isn’t your main issue. But then you wake up feeling foggy all day. Mirtazapine? It’s a sweet spot for many: it boosts total sleep time by nearly an hour and cuts the time it takes to fall asleep by 28 minutes. But at doses above 30 mg, it can make you so sleepy you forget to eat lunch.
And then there’s the sneaky stuff: REM sleep without atonia. That’s when your muscles don’t relax during dreaming. It’s normal in babies. Not normal in adults. About 68% of people on SSRIs show this on sleep studies - compared to 22% of people not on meds. It’s linked to acting out dreams, which can lead to injuries. If you’re suddenly punching pillows or yelling in your sleep, don’t ignore it.
Which Antidepressants Are Worst for Sleep?
Not all antidepressants treat sleep the same way. Here’s what the data shows:| Medication | Effect on Sleep Onset | Effect on Total Sleep | REM Sleep Change | Common Complaint |
|---|---|---|---|---|
| Fluoxetine (Prozac) | Severe delay (78% of users) | Decreased | -29% | Insomnia, vivid dreams |
| Sertraline (Zoloft) | Moderate delay (65%) | Slight decrease | -22% | Restlessness, nighttime awakenings |
| Mirtazapine (Remeron) | Improved by 28 min | +53 min | -15% | Daytime drowsiness, weight gain |
| Trazodone | Improved by 25 min | +40 min | -10% | Hangover effect, dry mouth |
| Agomelatine | Improved | +35 min | -8% | Limited availability, liver monitoring |
| Bupropion (Wellbutrin) | Worsens | Decreased | Minimal change | Insomnia, anxiety |
Fluoxetine is the worst offender for insomnia. If you’re already struggling to sleep, it’s not the best first choice. Sertraline is a bit gentler, but still hits hard for many. Bupropion? Don’t combine it with SSRIs - it doubles your risk of sleep disruption. On the flip side, mirtazapine and trazodone are often used off-label as sleep aids. But they’re not harmless. Trazodone can leave you groggy until noon. Mirtazapine can make you gain weight and feel like you’re walking through molasses.
Timing Matters More Than You Think
Taking your pill at the wrong time can ruin your sleep - even if the drug itself is sleep-friendly. SSRIs should be taken before 9 a.m. That’s not a suggestion. It’s backed by a 2020 study showing this cuts insomnia risk by 41%. Why? Because these drugs stimulate your brain. If you take them at night, your body thinks it’s time to wake up.For sedating antidepressants like trazodone or mirtazapine, timing is just as crucial. Take them 2-3 hours before bed. Too early, and you’ll crash mid-afternoon. Too late, and you might not fall asleep because your body’s still processing the drug. A 2021 trial showed people who took trazodone at 9 p.m. had better sleep quality than those who took it at 11 p.m. - even though both groups took the same dose.
And here’s something most doctors don’t tell you: some people find relief by splitting their SSRI dose. Half in the morning, half in the early afternoon. It’s not officially approved, but 41% of users on Reddit reported it helped. A clinical trial at the University of Michigan is now testing this exact approach. If your insomnia sticks around past week three, talk to your doctor about it.
What to Do If Sleep Doesn’t Improve
Most people’s sleep gets better after 3-4 weeks. That’s the pattern. But if you’re still wide awake at 2 a.m. after four weeks, it’s not just adjustment. It’s a signal. Here’s what to try:- Switch to a sleep-friendly option. If you’re on fluoxetine and can’t sleep, ask about mirtazapine or agomelatine. Both are proven to help sleep without crushing your energy.
- Lower the dose. For venlafaxine, starting at 37.5 mg instead of 75 mg cuts insomnia risk by 32%. Sometimes less is more.
- Add a short-term sleep aid. Melatonin (3 mg at bedtime) can help reset your rhythm. Trazodone at 25-50 mg can help for the first 2-4 weeks while your body adjusts to the SSRI.
- Track your sleep. Use a simple sleep diary for two weeks. Note bedtime, wake time, how long it took to fall asleep, and how many times you woke up. Bring it to your next appointment. Numbers beat complaints.
- Rule out RLS or REM behavior disorder. If you’re kicking your legs at night or acting out dreams, ask for a sleep study. SSRIs can trigger these conditions, and they need specific treatment.
What the Experts Really Say
There’s a split in the medical community. Some, like Dr. Dieter Riemann, say REM suppression is a sign the drug is working - and that the better the REM change, the better the depression response. Others, like Dr. Madhukar Trivedi, argue it doesn’t matter at all. The truth? It matters for you.If you’re a 45-year-old nurse with insomnia-predominant depression, your sleep isn’t a side effect - it’s the main problem. Starting you on an SSRI is like giving someone with a broken leg a painkiller that makes them limp harder. You need a drug that fixes the leg and lets them walk. That’s why the Mayo Clinic and CANMAT guidelines now recommend mirtazapine 15 mg as a first-line option for depression with insomnia.
And the field is changing fast. In 2023, the FDA started requiring all new antidepressants to report REM sleep data. A new drug, zuranolone, was approved specifically because it improves sleep in two weeks - not six. And now, companies like Genomind are offering genetic tests that predict how you’ll respond to 24 different antidepressants based on your sleep genes. This isn’t sci-fi anymore. It’s the next step.

Real People, Real Stories
One woman on Reddit said she tried fluoxetine for six weeks. She lost 12 pounds because she couldn’t eat. She was up every night. Her therapist told her to "just wait it out." On week seven, she switched to mirtazapine. Within three days, she slept 7 hours straight for the first time in months. But now she’s gained 15 pounds and can’t stay awake in meetings.A man in his 50s took sertraline and trazodone together. He slept fine, but felt like a zombie. He dropped the trazodone, switched to agomelatine, and now sleeps well, wakes up refreshed, and hasn’t gained weight. He’s been stable for 18 months.
There’s no one-size-fits-all. What works for one person can wreck another. That’s why your experience matters - and why your doctor needs to listen to it.
What to Ask Your Doctor
Don’t just accept the first prescription. Ask these questions:- "Is my depression mostly with insomnia or hypersomnia?"
- "Which antidepressant has the least impact on sleep for someone like me?"
- "Can we start with a lower dose to see how I react?"
- "Should I take this in the morning or at night?"
- "Are there any signs I should watch for that mean I need a sleep study?"
If your doctor dismisses your sleep problems as "just part of the process," find someone who understands the connection between sleep and antidepressant response. Your sleep isn’t a side effect - it’s a signal. And it’s telling you something important.
Do all antidepressants cause insomnia?
No. While SSRIs and bupropion often cause insomnia, other antidepressants like mirtazapine, trazodone, and agomelatine are actually prescribed to help with sleep. About 87% of antidepressants affect sleep architecture, but the direction of the effect varies widely by drug class. Some increase sleep, others disrupt it.
How long does SSRI-induced insomnia last?
For most people, insomnia peaks between days 3 and 7 after starting an SSRI and begins to improve by week 3. By week 4, about 72% of users report better sleep. If insomnia persists beyond 4 weeks, it’s unlikely to resolve on its own - and you should discuss switching medications or adjusting your dose.
Is it safe to take melatonin with antidepressants?
Yes, melatonin is generally safe to take with most antidepressants. Studies show 3 mg of melatonin at bedtime can help reset circadian rhythms and reduce sleep onset latency without interfering with antidepressant effectiveness. It’s often recommended as a short-term aid during the first few weeks of treatment.
Can I split my SSRI dose to reduce insomnia?
Some people find splitting their SSRI dose - taking half in the morning and half in the early afternoon - reduces nighttime insomnia without lowering effectiveness. While not yet standard, this approach is being studied in a clinical trial at the University of Michigan. Always consult your doctor before changing your dosing schedule.
Why does my doctor keep saying to "wait it out"?
Many doctors still believe sleep disruption is temporary and a sign the medication is working. While sleep often improves after 3-4 weeks, for 20-30% of people, it doesn’t. Waiting too long can lead to treatment dropout. If your sleep hasn’t improved by week 4, or if you’re feeling worse, it’s time to revisit your treatment plan - not just endure it.
Are there antidepressants that don’t affect sleep at all?
No antidepressant has zero effect on sleep. But agomelatine comes closest - it reduces REM sleep by only 8% compared to 22% for SSRIs and actually improves sleep continuity. It’s not available everywhere, but for people with severe insomnia, it’s often the best option when accessible.









14 Comments
Okay but can we talk about how nobody warns you that mirtazapine turns you into a sleepy potato? I took it for two weeks, slept like a baby, then gained 8 pounds and forgot where I put my keys. Worth it? Maybe. But my cat now judges me harder than my therapist.
You people are so dramatic. I took sertraline for 6 months and slept like a log. If you can’t sleep, maybe you’re just not trying hard enough. Stop making everything about your brain chemistry. Go outside. Breathe. Stop being so sensitive.
Big respect to the OP for laying this out so clearly 🙌 I’ve been on bupropion + trazodone combo for 8 months and it’s been a rollercoaster. The trazodone helped me fall asleep, but I’d wake up at 3 a.m. feeling like I’d been hit by a truck. Then I switched to agomelatine - no more zombie mode, no weight gain, and I actually remember my dreams (in a good way). Also, melatonin 3mg at bedtime? Game changer. 🌙
It is deeply concerning that so many in the United States appear to treat psychiatric medication as if it were a convenience store purchase. In the United Kingdom, we have stringent guidelines - and proper monitoring. To suggest splitting SSRI doses without clinical oversight is, frankly, irresponsible. The NHS would never permit such a practice. One must adhere to protocol, not Reddit anecdotes.
So you're telling me I'm not lazy, I'm just chemically wired to be awake at 2am? Wow. My therapist is gonna cry. Also, I took fluoxetine and now I dream I'm being chased by a giant antidepressant pill. It's like Inception but with more anxiety and less Leonardo DiCaprio.
I used to think sleep was just a luxury - until I realized it was the foundation of everything. When your brain is stuck in hyperdrive because of an SSRI, it’s not just about being tired. It’s about losing pieces of yourself. The way you laugh. The way you hold your coffee. The way you remember your mom’s voice. I switched to mirtazapine and for the first time in a year, I woke up and didn’t immediately feel like I’d been drowning. It didn’t fix me - but it let me breathe again. And sometimes, that’s enough.
Of course the guy who wrote this is a doctor. They all say "wait it out" until you quit. Then they say "you weren’t ready." Meanwhile, I’m lying awake wondering if my brain is permanently rewired. You don’t get to call this "treatment" when it feels like torture.
To everyone saying "just wait it out" - I hear you. But I also remember being that person. I waited 6 weeks. I lost my job. I stopped talking to my friends. I didn’t realize until later that my silence wasn’t strength - it was survival. If your sleep hasn’t improved by week 4, it’s not weakness to ask for help. It’s wisdom.
Hey, if you’re still awake at 2 a.m., you’re not broken - you’re just in the middle of a chemical reset. I was there. Took me 3 months to find the right combo, but now I sleep 7 hours straight, wake up without caffeine, and actually like Mondays again. It’s not magic. It’s trial and error. And you’re not alone.
Let me tell you, in my 27 years of clinical observation and peer-reviewed literature review - which I have meticulously compiled in my personal database of 872 sleep studies - the notion that REM suppression correlates with therapeutic efficacy is not merely a hypothesis, it is an empirical pattern observed across five continents and three major pharmaceutical trials. That said, I do concede that individual neurochemical variance, particularly in those with polymorphisms in the SLC6A4 gene, may necessitate a personalized approach - which is why I always recommend genetic testing before initiating any SSRI regimen. Also, melatonin is overrated. Try L-theanine. It’s more natural.
Wow. So you’re telling me the reason I can’t sleep is because I’m taking the right drug? That’s… ironic. I thought antidepressants were supposed to make me feel better. Not turn me into a human nightlight.
According to the 2021 Cochrane Review on antidepressant-induced sleep disturbances, the mean latency to REM sleep increases by 62.3 minutes (CI: 57.1–67.5) with SSRIs, while total sleep efficiency decreases by 14.7% (CI: 12.1–17.3). Furthermore, the prevalence of REM sleep without atonia is significantly higher in SSRI users (p < 0.001). These data are not anecdotal; they are statistically significant and clinically reproducible. Please cite your sources before making claims.
This entire post is just pharmaceutical marketing dressed up as self-help. Nobody needs a 2,000-word essay to tell them that drugs have side effects. You’re not special. You’re not broken. You’re just another person who didn’t read the tiny print. Stop making this a trauma narrative. Take the pill. Sleep less. Get over it.
I just want to say - thank you for writing this. I’ve been on sertraline for 10 months. Sleep got better at week 5, but I still wake up feeling like I’ve been running a marathon. I started taking 1mg melatonin and it made a quiet difference. Not magic, but… gentler. And I’m still here. That’s something.