Medication Switch Calculator
How It Works
This tool helps you compare two medication options based on your personal priorities. Enter the absolute risk numbers and set your preferences to see which option fits you best.
Current Medication
New Medication Option
Your Priorities
Rate what matters most to you (1-10 scale)
Your Decision Result
How This Works
We compared both medications using your priorities. Your choices matter most.
Why This Matters
Personalized decisions reduce regret and increase confidence in your choice.
Your Priority Weight
Health Risk: | Side Effects: | Convenience:
Comparison Metrics
Risk Reduction: | Weight Gain:
What to Discuss With Your Doctor
- Ask: What is the absolute risk reduction for me personally?
- Ask: How does this choice affect my specific health conditions?
- Ask: What side effects should I monitor for?
What Happens When You Switch Medications?
Switching medications isn’t just swapping one pill for another. It’s a decision that can change how you feel every day - for better or worse. Maybe your current drug isn’t working well enough. Maybe the side effects are too much. Or maybe your doctor thinks there’s a safer or cheaper option. But here’s the thing: without clear, personalized information, most people feel overwhelmed. And that’s where decision aids come in.
These aren’t just brochures or websites with generic advice. Decision aids are tools built to help you and your doctor make a choice together - based on what matters most to you. They lay out the real numbers: how likely are you to have a heart attack if you stay on this drug? What’s the chance you’ll gain weight or feel dizzy on the new one? And most importantly - which side effects are you willing to live with?
How Decision Aids Work (And Why They’re Different)
Traditional advice might say: “This new medication is better.” But better for whom? Decision aids cut through the noise. They show you the facts in plain terms - not percentages that sound impressive, but real-world examples.
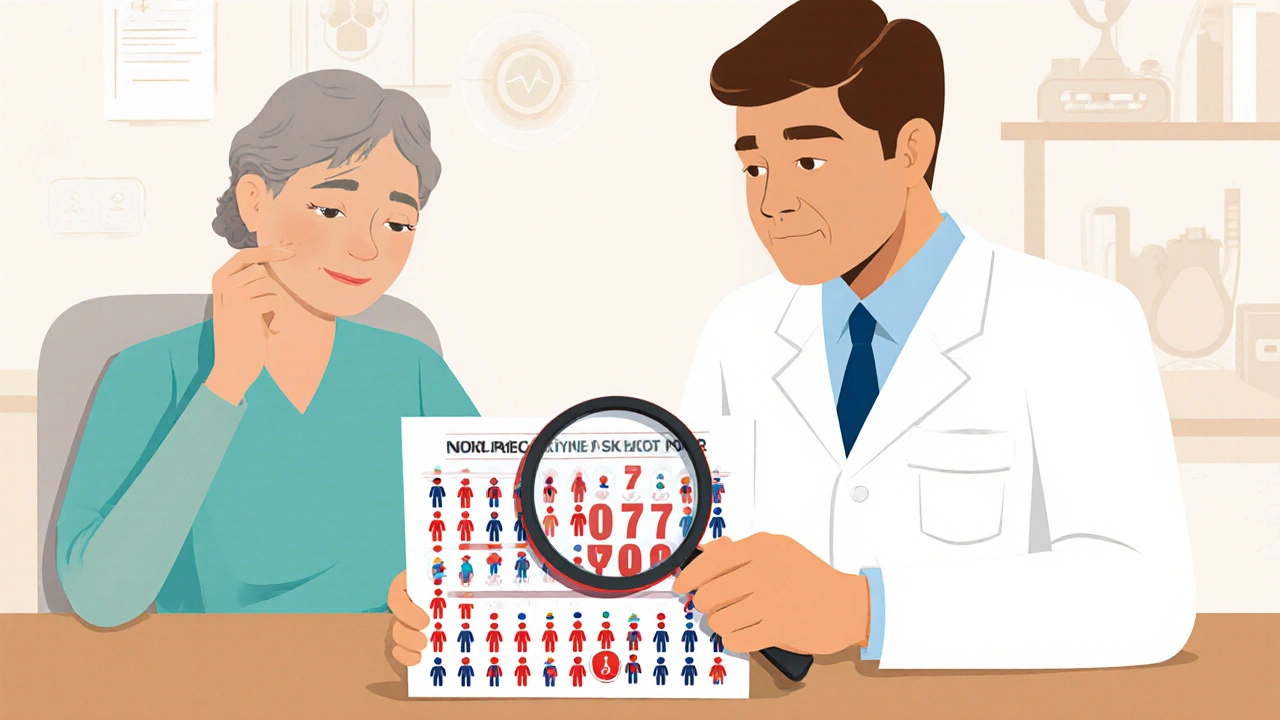
For example, instead of saying “this drug reduces stroke risk by 30%,” a good decision aid will say: “Out of 100 people like you, 10 will have a stroke in five years on your current medicine. On the new one, that number drops to 7. So 3 people out of 100 will avoid a stroke.” Then it shows icons - little pictures of people - so you can see it visually. One group of 100 with 10 red dots (stroke risk). Another with 7. Suddenly, it’s not abstract. It’s human.
These tools also ask you what you care about. Do you hate taking pills twice a day? Are you terrified of bleeding? Worried about cost? You rank these things. The aid then shows you which options match your priorities. One medication might have a lower risk of weight gain but needs three doses a day. Another might be cheaper but has a 1 in 5 chance of nausea. You don’t just get options - you get clarity.
The Real Benefits: Less Regret, More Control
Studies show people who use decision aids feel more confident. In one large review of over 100 trials, patients who used these tools scored 15-25% higher on tests about their medications. They understood the risks better. They knew what to watch for. And they were less likely to regret their choice later.
That matters because nearly half of all patients stop their meds within the first year - not because they’re noncompliant, but because they didn’t fully understand the trade-offs. One man switched from warfarin to a newer blood thinner after using a VA decision aid. He’d been scared of bleeding. The tool showed him: out of 100 people, 8 on warfarin had a major bleed in a year. On the new drug, it was 3. He chose the switch. Another woman, after seeing the numbers, decided to stay on her old antidepressant - even though it wasn’t perfect - because the alternative had a 1 in 4 chance of causing tremors, and she was a musician. She didn’t want to risk her hands shaking during performances.
Decision aids don’t tell you what to do. They help you know why you’re doing it.
The Risks: Too Much Info, Too Little Time
But it’s not perfect.
Some people feel bombarded. One study found 31% of users said there were “too many numbers.” If you’re not used to thinking in probabilities, seeing charts and icons can feel confusing, not helpful. A few patients even misunderstood the data - thinking a 20% risk reduction meant they were now safe, not that the risk went from 10% to 8%.
And then there’s the time issue. Doctors are busy. A good decision aid session adds 7 to 12 minutes to a visit. Many clinicians say they don’t have it. In a survey of 1,200 doctors, 68% said workflow disruption was a major barrier. If the tool isn’t built into the electronic health record, or if the patient doesn’t get it ahead of time, it’s easy to skip.
Also, these tools aren’t meant for emergencies. If you’re having a heart attack or a severe allergic reaction, you don’t need a decision aid - you need action. They’re for planned changes, when there’s time to think.

Who Benefits Most?
Decision aids shine in situations where there’s no single “right” answer. For example:
- Switching from one diabetes drug to another - metformin to an SGLT2 inhibitor or GLP-1 agonist
- Choosing between different blood thinners - warfarin vs. DOACs
- Changing antidepressants when the first one didn’t work well
In each case, multiple options exist. All are supported by evidence. But the side effect profiles differ. The cost varies. The dosing schedule changes. What’s best for one person might be terrible for another.
That’s why experts like the National Academy of Medicine say these decisions are “preference-sensitive.” They’re not just clinical - they’re personal. And that’s exactly where decision aids help the most.
What You’ll Find in a Good Decision Aid
Not all tools are created equal. A strong one includes:
- Clear clinical question: “Should I switch from Drug A to Drug B?”
- Real numbers: Absolute risks, not just relative ones. “Your chance of bleeding goes from 8% to 4%.”
- Visuals: Icon arrays, bar charts, color-coded risk levels.
- Side-by-side comparison: Table showing each option’s side effects, cost, dosing, and monitoring needs.
- Value clarification: “How important is avoiding weight gain vs. avoiding daily injections?” You rank them.
- Next steps: What to ask your doctor. What to watch for after switching.
Tools from the VA, Mayo Clinic, and the Ottawa Hospital Research Institute are among the most trusted. Many are free and available online. Some even work in 12 languages and meet accessibility standards for people with vision or mobility challenges.
How to Use One - Step by Step
- Ask your doctor: “Is there a decision aid for this switch?” Don’t wait for them to offer it. Many still don’t know about them.
- Get it early: Request it 24-72 hours before your appointment. Read it alone first. Write down questions.
- Bring your priorities: What side effects scare you? What’s your budget? Do you hate pills? Be honest.
- Use it in the room: Don’t just hand it to your doctor. Say, “I read this. Here’s what stood out to me.”
- Ask for a copy: Save it. You’ll need it later when you’re adjusting or checking in.
Some clinics now send these tools through patient portals. Others email them. If yours doesn’t, ask if they can print one. Paper works too.
What to Watch Out For
Not every tool is trustworthy. Some are made by drug companies and downplay risks. Look for these signs of credibility:
- Developed by a university, hospital, or government agency (like the VA or NIH)
- Lists sources - studies, guidelines, FDA labels
- Shows both benefits and harms equally
- Doesn’t push one option
- Updated within the last 2 years
Watch out for phrases like “most effective” or “newest breakthrough.” Real decision aids avoid hype. They say: “Here’s what we know. Here’s what we don’t.”
What If You Don’t Use One?
You can still make a good decision without a tool. But you’re more likely to rely on your doctor’s quick recommendation - or on internet rumors. One woman switched to a new statin because her friend said it “didn’t cause muscle pain.” She ended up with severe cramps and had to stop. She didn’t know her own risk was 1 in 20 - and her friend’s was 1 in 100.
Without a structured way to weigh trade-offs, you might choose based on fear, cost, or convenience - not what’s truly best for your body and life.
Final Thought: This Is Your Body, Not a Checklist
Medication changes aren’t about picking the “best” drug. They’re about finding the right fit for you. Your job isn’t to be a passive patient. It’s to be a partner. Decision aids give you the tools to do that - without jargon, without pressure, without guesswork.
Next time your doctor suggests a switch, ask: “Is there a decision aid for this?” It might be the most important question you ever ask.
Are decision aids only for serious conditions like heart disease or diabetes?
No. Decision aids are useful for any medication switch where there’s more than one valid option and side effects matter. That includes antidepressants, blood pressure drugs, pain relievers, and even supplements. If your doctor says, “We could try X or Y,” and you’re unsure which is better for you, a decision aid can help.
Can I use a decision aid on my own, or do I need my doctor?
You can read one on your own - and you should. But the real power comes when you bring it to your doctor. These tools are designed for shared decision-making. Your doctor can explain what the numbers mean for your specific health, answer questions you didn’t think to ask, and help you adjust the options based on your full medical history.
What if I don’t understand the statistics?
That’s normal. Most people aren’t trained to interpret risk numbers. Good decision aids use visuals - like icons showing 100 people - to make it easier. If something’s confusing, say so. Ask your doctor to explain it again. You can even ask for a simpler version. There’s no shame in needing it broken down.
Do insurance companies or pharmacies provide these tools?
Some do - especially larger health plans or Medicare Advantage plans, which are now required to support shared decision-making. But the most reliable ones come from independent medical institutions like the VA, Mayo Clinic, or the Ottawa Hospital. Don’t trust tools made by drug companies unless they’re clearly labeled as independent and unbiased.
What if my doctor says I don’t need a decision aid?
You still have the right to ask for one. Say: “I’ve read that these tools help patients make choices that fit their values. Could we use one for this switch?” If your doctor refuses, ask why. If it’s because they don’t know how to use it, offer to find one together. If they say it’s not needed, ask what evidence supports their recommendation - and whether it’s based on your priorities, not just clinical guidelines.
Are these tools available in my language?
Many are. The Ottawa Hospital’s collection supports 12 languages, including Spanish, Mandarin, Arabic, and Tagalog. The VA’s tools are available in English and Spanish. Check the website of the organization offering the aid - they usually list language options. If you can’t find one in your language, ask your clinic if they can provide translation support during your visit.
How do I know if a decision aid is up to date?
Look for a publication or update date on the tool. Reputable ones are reviewed every 18-24 months, especially when new drug labels come out. If the tool doesn’t show a date, or if it hasn’t been updated in over two years, it may be outdated. Ask your doctor if the information matches current guidelines - and check the source. Government or academic sites are more likely to be current than commercial ones.
Next Steps: What to Do Right Now
If you’re thinking about switching a medication - or your doctor has mentioned it - here’s what to do:
- Write down the name of your current drug and the one being suggested.
- Search for “decision aid” + [drug name] + “switch.” Try adding “VA,” “Mayo Clinic,” or “Ottawa Hospital.”
- Read one before your appointment. Highlight what confuses you.
- Ask your doctor: “Can we go over this together?”
- After your visit, keep a copy. Use it to track side effects or changes in how you feel.
Switching meds is a big step. You don’t have to make it alone. With the right tool, you can turn fear into clarity - and confusion into control.











8 Comments
I used one of these when switching my blood pressure med. The icon thing with the 100 people? Made it click. I stayed on my old one because I hate pills twice a day and the new one needed three. No regrets.
Also, my doc had never heard of it. I had to print it myself.
I find it utterly astonishing that anyone would require a visual aid to comprehend basic risk statistics. In my day, we were taught probability in primary school. Now we need animated icons to understand that 8% is greater than 4%. This is not progress. This is infantilisation.
Furthermore, the notion that a patient’s ‘priorities’ should override clinical evidence is a dangerous drift toward emotional governance of medicine. I am appalled.
LMAO so now we need a whole PowerPoint presentation just to switch from lisinopril to amlodipine? My grandma took 3 different blood pressure pills in the 70s and never once opened a PDF. She just took ‘em and didn’t complain. Guess she was too busy being a human, not a data point.
Also, why does every ‘decision aid’ have those stupid little people icons? Are we 5? 😒
I used one for my antidepressant switch. It showed me the tremor risk was 25%. I’m a pianist. I stayed on the old one. Best decision I ever made. No emojis needed.
This is exactly the kind of thing we need in healthcare. Too many people are scared to ask questions because they feel dumb. These tools give them the language to speak up. I work in a clinic and I’ve seen patients cry because they finally understood what was happening to them. It’s not about dumbing down - it’s about lifting people up.
Also, if your doc says you don’t need it, ask them why they’re so scared of you being informed. That’s not medicine - that’s control.
I get why people hate these things. I used to be one of them. Thought they were fluff. Then I had to choose between two diabetes meds. One had a 1 in 5 chance of nausea. The other had a 1 in 10 chance of kidney issues. I didn’t even know those were options. I thought the doc just picked one. Turns out, I had a say. And I didn’t know what I cared about until I saw the choices side by side.
Yeah, it takes time. Yeah, the icons look like clip art. But if you’re going to be on this stuff for life, shouldn’t you know what you’re signing up for? I didn’t want to be the guy who just followed orders and then ended up in the ER because he didn’t realize ‘mild dizziness’ meant ‘I can’t stand up without throwing up.’
Also, if your doc doesn’t have one, ask for the Ottawa one. It’s free. Google it. Don’t wait for them to be perfect. Be the person who pushes for clarity.
I read this whole thing. Honestly? It’s good. But here’s the thing nobody says: most people don’t read this stuff. They scroll past it. They’re tired. They’re anxious. They just want the doc to tell them what to do. And honestly? Sometimes the doc’s right.
But then again, sometimes the doc’s just rushing. And sometimes the patient’s got a 30-year history of migraines and the doc doesn’t even ask. So maybe the tool helps. But it’s not magic. It’s just another layer. And if the system’s already broken, adding a PDF isn’t fixing it. It’s just putting a Band-Aid on a hemorrhage.
As someone who has studied health communication across 12 countries, I find this approach profoundly aligned with the principles of patient autonomy and cognitive accessibility. The use of icon arrays to represent absolute risk is not merely pedagogical-it is ethically necessary in contexts where numeracy disparities are systemic. The VA’s implementation, particularly in multilingual formats, demonstrates a commitment to equity that transcends mere clinical efficacy.
However, I must note that cultural attitudes toward authority in healthcare vary significantly. In some societies, questioning a physician’s recommendation is perceived as disrespectful. Thus, while the tool is excellent, its efficacy is contingent upon sociocultural readiness. This is not a technical problem-it is a cultural one.