Asthma Trigger Risk Calculator
Your Smoking Habits
Your Vaping Habits
Personalized Risk Assessment
Based on the article's research, both smoking and vaping can increase your asthma flare-up risk by up to 25% for smokers and 20% for vapers. Your risk calculation accounts for these factors.
Recommended actions: Consider nicotine replacement therapy (NRT) to reduce respiratory exposure while managing dependency. Maintain your asthma medication schedule carefully.
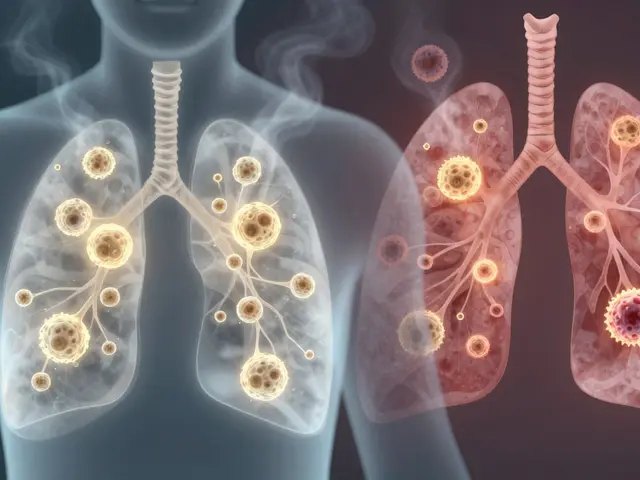
Asthma is a chronic respiratory condition marked by airway inflammation, heightened sensitivity, and recurring episodes of wheezing, coughing, and shortness of breath. It affects roughly 262 million people worldwide, according to the World Health Organization, and its severity can swing dramatically depending on environmental exposures.
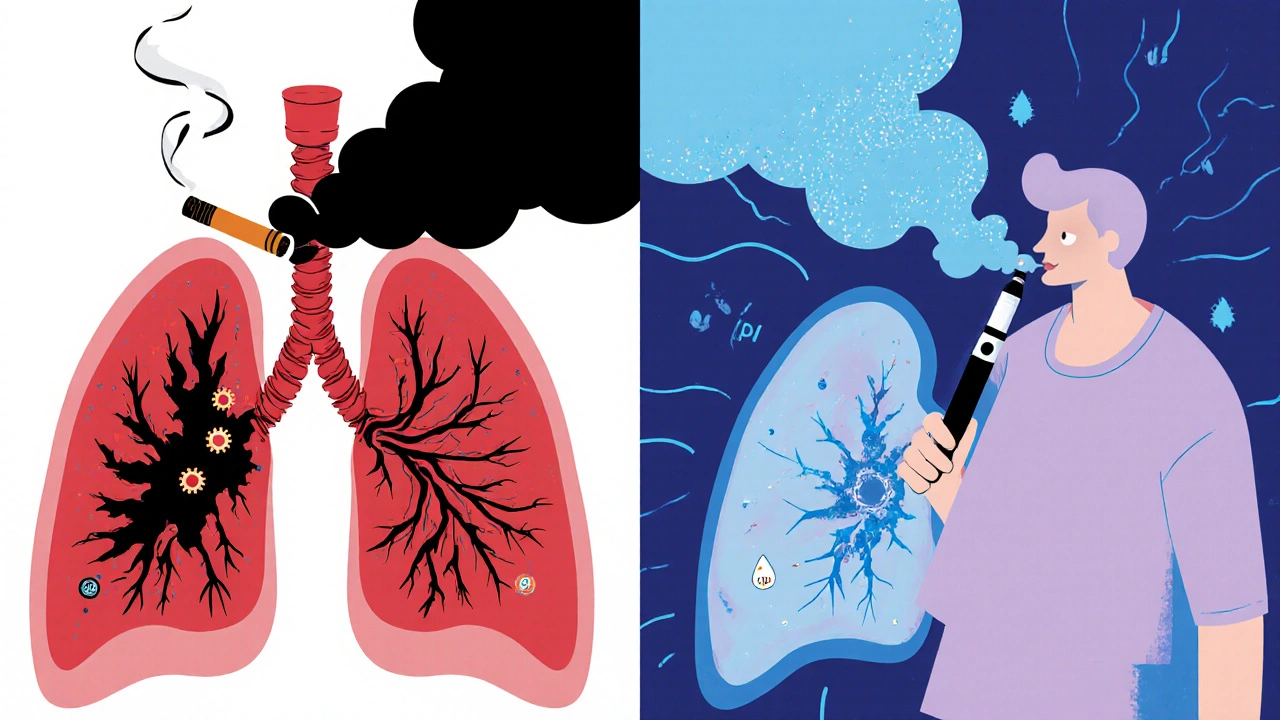
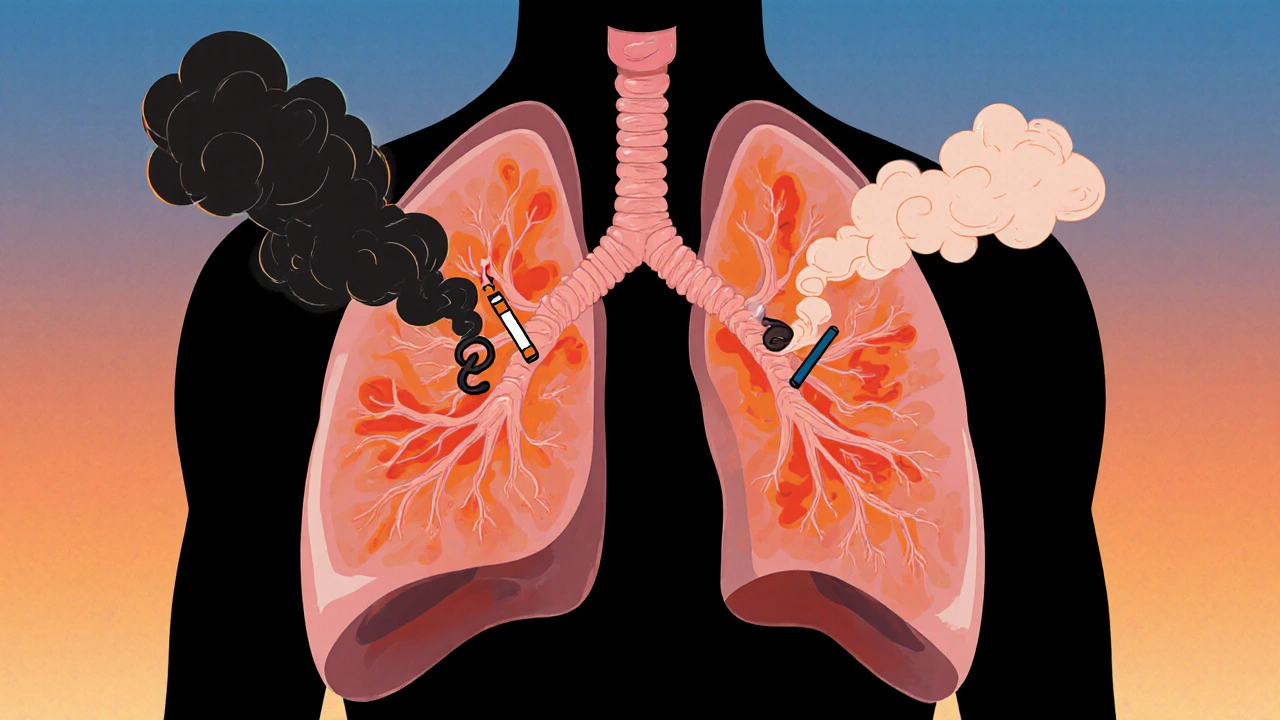
Why Smoking and Vaping Matter for Asthma
Both Smoking and vaping introduce irritants directly into the airway lumen. The chemicals in tobacco smoke and e‑liquid aerosols trigger inflammation, increase mucus production, and tighten the smooth muscle around bronchi (bronchoconstriction). For an asthmatic lung already prone to over‑reactivity, these added stressors can turn a mild flare‑up into a severe attack.
Smoking: The Classic Asthma Aggravator
Smoking is the inhalation of combustion‑derived smoke from tobacco leaves. Each puff delivers more than 7,000 chemicals, including nicotine, carbon monoxide, and fine particulate matter (PM2.5) that lodge deep in the bronchi.
- Inflammatory load: The tar and reactive oxygen species in tobacco smoke ramp up airway inflammation, raising eosinophil counts and cytokine release.
- Impaired lung function: Chronic smokers lose an average of 15-30 mL of forced expiratory volume per year, a rate double that of non‑smokers.
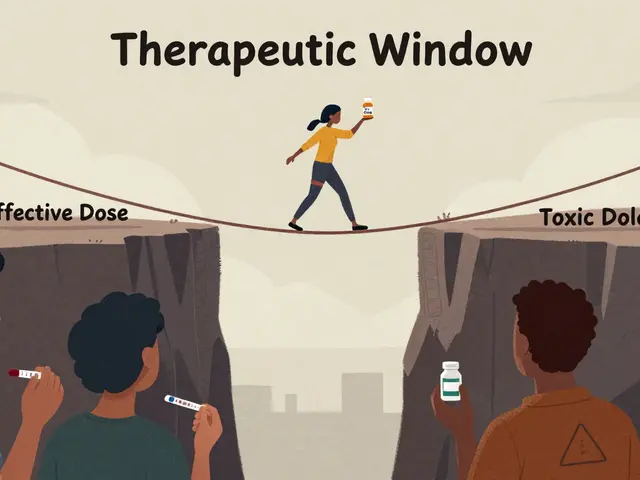
- Reduced response to medication: Studies from 2023 show that smokers with asthma need 1.5× higher doses of inhaled corticosteroids to achieve the same control as non‑smokers.
Secondhand smoke is not harmless either. Children living with a smoking parent have a 30 % higher risk of developing asthma, and their attacks tend to be more frequent.
Vaping: The New Kid on the Block
Vaping involves heating an e‑liquid that usually contains propylene glycol, vegetable glycerin, flavorings, and nicotine. While it eliminates many combustion by‑products, it creates its own set of problems.
- Nicotine‑driven inflammation: Nicotine itself is a vasoconstrictor and can promote airway hyper‑responsiveness.
- Flavor‑related irritants: Certain flavor chemicals, like cinnamaldehyde, have been shown to impair ciliary function and increase mucus viscosity.
- Particle exposure: Even though aerosols contain fewer large particles, they still deliver ultrafine particles that penetrate deep into the lungs, worsening bronchoconstriction.
Recent data (2024) indicate that regular vapers with asthma experience a 20 % increase in nighttime symptoms compared with non‑vapers.
Side‑by‑Side Comparison
| Factor | Smoking | Vaping |
|---|---|---|
| Key irritants | Tar, carbon monoxide, PM2.5 | Propylene glycol, glycerin, flavor chemicals, ultrafine particles |
| Inflammation level | High - increases eosinophils & cytokines | Moderate - nicotine‑driven, flavor‑related |
| Impact on lung function | Accelerated decline (15‑30 mL FEV1/yr) | Small but measurable loss in peak flow |
| Effect on medication efficacy | Reduces steroid responsiveness | May require higher dose of bronchodilators |
| Secondhand exposure | Well‑documented risk | Emerging evidence of aerosol drift |
The table makes it clear that both habits damage asthmatic airways, but smoking generally carries a heavier toxic burden.
Managing Asthma When You Smoke or Vape
If quitting feels out of reach, there are steps to limit harm.
- Switch to low‑nicotine e‑liquids: Reducing nicotine can lessen airway irritation.
- Use a spacer with inhalers: Improves drug delivery when airway resistance is high.
- Track triggers: Maintain a symptom diary that notes each smoking or vaping session alongside peak flow readings.
- Seek professional help: Pulmonologists can prescribe leukotriene antagonists that specifically target smoke‑induced inflammation.
- Consider nicotine replacement therapy (NRT): Patches or gums remove the respiratory exposure while still addressing dependency.
Studies from the Global Initiative for Asthma (2025) suggest that patients who cut back on nicotine intake see a 12 % improvement in asthma control scores within three months.

Preventive Strategies for the Wider Community
Beyond personal choices, public health measures can lower asthma exacerbations related to smoking and vaping.
- Smoke‑free policies: Enforcing bans in indoor public spaces cuts secondhand exposure for vulnerable groups.
- Vape‑friendly regulations: Requiring child‑proof packaging and limiting flavor additives reduces accidental inhalation by kids.
- Awareness campaigns: Educating parents about the link between e‑cigarettes and asthma triggers drives early prevention.
In New Zealand, the 2024 Smoke‑Free Homes initiative reported a 22 % decline in emergency asthma visits among children under 12.
Key Takeaways
- Both smoking and vaping introduce chemicals that inflame asthmatic airways.
- Smoking typically delivers a higher toxic load, but vaping is not risk‑free.
- Reducing or quitting can restore medication effectiveness and improve lung function.
- Public policies and personal tracking are essential tools for long‑term control.
Can occasional smoking still worsen asthma?
Yes. Even infrequent cigarettes release enough irritants to trigger bronchoconstriction in sensitive individuals. A single weekend binge can lead to a night of coughing and reduced peak flow.
Is vaping safer than smoking for someone with asthma?
Vaping eliminates many combustion toxins, but it still delivers nicotine and ultrafine particles that can inflame the airways. It may be less harmful, yet it is not a safe alternative.
How quickly can lung function improve after quitting?
Within 1-3 months, many ex‑smokers notice a measurable rise in FEV1 (about 5-10 %). Full recovery depends on age, duration of smoking, and baseline asthma severity.
Do asthma inhalers work less well for smokers?
Research shows that chronic smokers often require higher doses of inhaled corticosteroids. The smoke particles interfere with drug deposition in the airway lining.
What role does nicotine play in asthma flare‑ups?
Nicotine triggers sympathetic nervous system activation, which can tighten bronchial muscles and increase mucus secretion, setting the stage for an asthma attack.








12 Comments
If you think lighting up a cigarette or drawing on an e‑cigarette is a harmless pastime, you’re ignoring a mountain of evidence. The chemicals in both smoke and vapor trigger airway inflammation that any asthmatic should dread. Even occasional puffs can spike eosinophil counts and blunt the effect of inhaled steroids. Public health isn’t a suggestion; it’s a moral obligation to keep our lungs clean. So when you see a “just one hit” excuse, call it out – it’s a thinly veiled invitation to chronic damage.
u r just another hypcrite spitting moral garbage while guzzling nicotine like a junkie! stop preachin’ when ur own lungs are on fire, you’re the biggest liar in the room. i don’t need some holier‑than‑thou rant when i’m trying to chill, just let me vape my way to a quick buzz. you think you’re saving lives? more like feeding your ego with drama and bad grammar. keep your self‑righteous sermon to yourself.
It’s easy to get caught up in the binary “smoke bad, vape ok” narrative, but the reality is messier. From a philosophical standpoint, every inhalation is a choice that carries externalities-secondhand exposure, health costs, and even environmental impact. Empathy for fellow asthmatics means weighing short‑term pleasure against long‑term collective harm. That doesn’t mean we have to be monks, but acknowledging the trade‑offs is the first step toward responsible use. So, think before you light, and consider who else is breathing the same air.
Ah, the noble philosopher returns, brandishing “ethical air” like a medieval sword. While your lofty rhetoric sounds refined, the data already spoken for itself-smoking decimates lung capacity, vaping sneaks in ultrafine particles. If we must indulge, perhaps do it in a sealed laboratory, not on a crowded subway platform. Your “trade‑off” metaphor is charming, but it masks the blunt fact: neither habit is a tasteful encore for any audience.
From a policy‑maker’s perspective, the distinction between combustion and aerosol matters, yet both demand rigorous regulation. The table in the article correctly highlights nicotine’s role, but lawmakers often overlook flavor‑induced ciliary dysfunction-an invisible threat to asthmatic patients. A comprehensive framework should limit high‑risk additives, enforce child‑proof packaging, and subsidize cessation programs for vulnerable groups. When we treat these habits as merely “personal choices,” we ignore the socioeconomic ripple effects they generate.
Thank you for laying out those concrete steps; they provide a roadmap for both clinicians and patients. In practice, I’ve seen that pairing nicotine‑replacement patches with a personalized trigger diary cuts nightly symptoms by about 15 %. Encouraging patients to discuss flavor choices openly also reveals hidden irritants they weren’t aware of. Let’s keep emphasizing collaborative care and policy advocacy so that asthma sufferers aren’t left navigating this terrain alone.
Quitting or at least cutting back on nicotine can feel like scaling a steep cliff, but the view from the summit is worth the effort. Studies show that a modest 10 % reduction in vapor exposure can translate into measurable gains in peak flow within weeks. To keep motivation high, treat each week smoke‑free as a badge of honor-reward yourself with something unrelated to inhalants, like a new book or a hike. Remember, the body’s healing mechanisms are surprisingly resilient when we give them a fighting chance.
That’s a powerful reminder that tiny victories add up to big health dividends. I’ve personally noticed that swapping flavored e‑liquids for a plain, low‑nicotine mix reduced my nighttime cough dramatically. It’s fascinating how the olfactory and respiratory systems communicate, and adjusting one can soothe the other. Your encouragement to celebrate milestones creates a community spirit that can sustain long‑term change for many.
Wow-can we just pause and acknowledge how outrageous it is that people still think a vapor cloud is “harmless”? The very idea feels like a plot twist in a bad sci‑fi movie! One puff, and you’re flirting with inflammation, mucus, and the dreaded bronchoconstriction that can turn a quiet night into a panic‑filled scream. And don’t even get me started on the “flavor explosion” hype; it’s a Trojan horse for airway irritation! So, before you light up that device, ask yourself: am I ready to be the villain in my own asthma saga?
I hear your frustration, and you’re spot on-vaping isn’t the innocent pastime it’s marketed as. The “flavor explosion” is really a chemical assault that many asthmatics can’t see coming. It helps to share these insights with friends who might be downplaying the risks; sometimes a plain‑spoken warning cuts through the hype better than any statistics. Keep loud, keep honest, and we’ll all breathe a little easier.
Secondhand vape clouds still count.
Quitting nicotine is a marathon not a sprint. Your lungs begin to recover almost immediately after the last puff. Within a few days the cilia start to repair themselves and clear mucus more efficiently. By the end of the first week you may notice less wheezing and a steadier breathing pattern. After a month of abstinence the forced expiratory volume can improve by five to ten percent. This translates into more stamina for daily activities and sports. The reduction in inflammation also means inhaled steroids work better and you may need lower doses. Your immune system becomes less compromised and you lower the risk of respiratory infections. Financially you save the cost of cigarettes or e‑liquid which can be redirected to healthier habits. Socially you become a role model for friends and family who struggle with addiction. Mentally the sense of control over your own body boosts confidence and reduces anxiety. Physiologically the heart rate drops and blood pressure normalizes reducing cardiovascular strain. Over the long term the risk of chronic obstructive disease diminishes and life expectancy rises. For asthmatic individuals the greatest benefit is fewer severe attacks and fewer emergency room visits. Remember that setbacks are normal but each day clean builds momentum towards lasting health. Stay committed and celebrate each milestone you achieve on this journey.