Colitis vs IBS Symptom Checker
Analysis Results
Important Note: This tool provides educational insights only. For accurate diagnosis and treatment, consult a healthcare professional.
Key Takeaways
- Colitis is an inflammatory condition of the colon; IBS is a functional disorder without visible inflammation.
- Both can produce similar abdominal pain, bloating, and irregular bowel movements, which often leads to confusion.
- Overlap occurs because chronic inflammation can alter gut motility and microbiome, mimicking IBS patterns.
- Accurate diagnosis relies on a combination of history, lab tests, and imaging - not just symptom checklists.
- Treatment plans may address both conditions simultaneously, focusing on diet, stress management, and targeted medication.
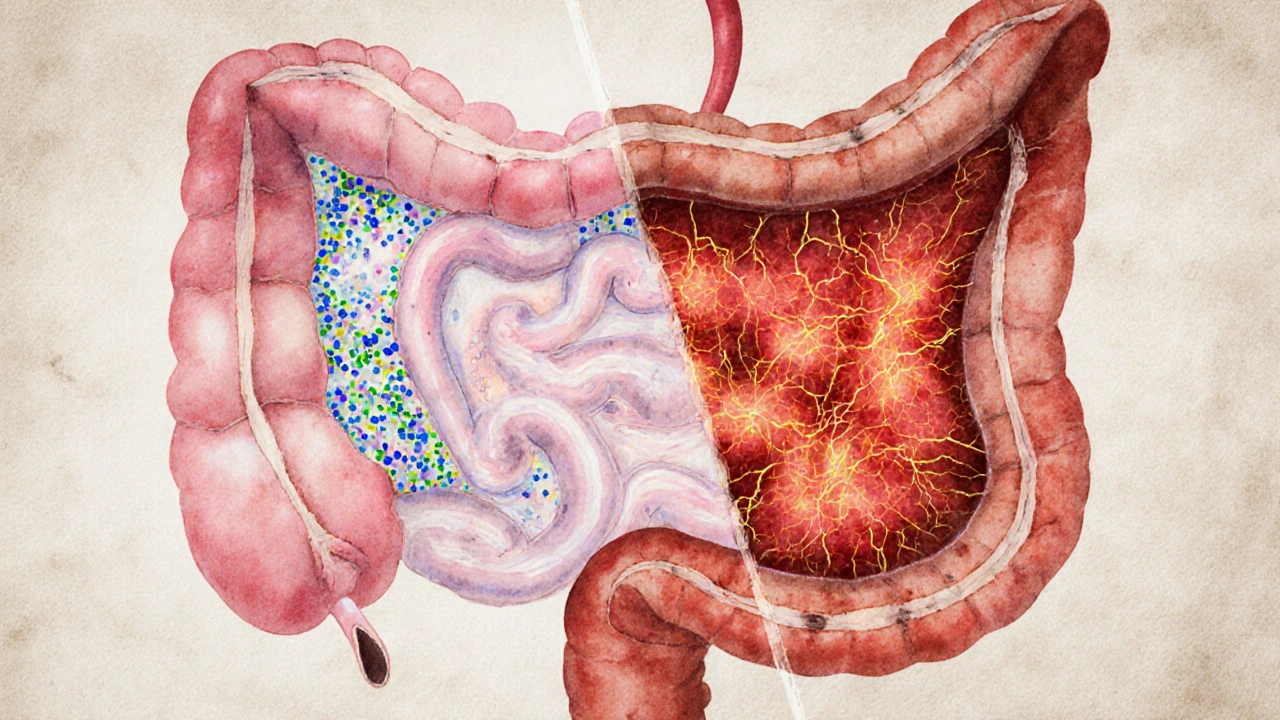
What Is Colitis?
When people hear “colitis,” they often picture severe inflammation of the colon. Colitis is a term that describes inflammation of the large intestine, which can be caused by infections, autoimmune reactions, or chronic conditions like ulcerative colitis. The inflamed lining becomes swollen, may bleed, and can develop ulcers. Common triggers include bacterial infections (e.g., Clostridioides difficile), medication side‑effects, and long‑standing immune disorders.
Because the colon is the final stop for water absorption, any irritation can quickly translate into diarrhea, urgency, or even constipation when the muscle layer spasms. In severe cases, blood in the stool and fever signal that the body is fighting a real infection or autoimmune attack.
What Is Irritable Bowel Syndrome (IBS)?
Irritable Bowel Syndrome is a functional gastrointestinal disorder marked by recurrent abdominal pain, bloating, and altered bowel habits without any detectable structural damage. Think of IBS as a miscommunication between the brain and the gut, often sparked by stress, diet, or a sensitive microbiome. Unlike colitis, there’s no visible inflammation on endoscopy, and lab work typically comes back normal.
IBS is classified into three sub‑types based on stool pattern: IBS‑D (diarrhea‑predominant), IBS‑C (constipation‑predominant), and IBS‑M (mixed). Each subtype may require slightly different lifestyle tweaks, but the core issue remains abnormal gut motility and heightened pain perception.
Why Do the Two Conditions Feel So Similar?
The gut is a tightly knit ecosystem. When the colon inflames, it releases cytokines and other signaling molecules that can sensitize the nerves lining the intestine. This heightened sensitivity can persist even after the inflammation eases, creating a lingering IBS‑like picture.
Conversely, chronic IBS symptoms can strain the gut lining, making it more vulnerable to infections that trigger an acute bout of colitis. In both directions, the colitis and IBS connection hinges on three physiological bridges:
- Gut microbiome disruption: Antibiotics used for colitis can wipe out beneficial bacteria, allowing gas‑producing species to flourish-classic IBS triggers.
- Visceral hypersensitivity: Inflammation heightens nerve signaling, so even minor distension feels painful.
- Motility changes: Inflammatory lesions may scar the muscle layers, causing erratic contractions that mimic IBS patterns.
How Doctors Distinguish Between Colitis and IBS
Because the symptoms overlap, clinicians follow a step‑by‑step algorithm to rule out one before confirming the other.
- Medical history: Sudden onset of bloody diarrhea or fever points toward colitis; gradual, lifelong pain with symptom relief after defecation leans toward IBS.
- Physical exam: Tenderness in the lower left quadrant, especially with guarding, suggests inflammation.
- Laboratory tests: Elevated C‑reactive protein (CRP) or fecal calprotectin are strong markers of colitis; normal values favor IBS.
- Endoscopic evaluation: Colonoscopy visualizes the mucosa; ulcerations confirm colitis, while a normal‑looking colon supports IBS.
- Stool studies: Pathogen panels detect infection‑related colitis; negative results push the diagnosis toward IBS.
In practice, many patients receive a provisional IBS diagnosis, only to have it revised when lab results reveal hidden inflammation.
Comparing Colitis and IBS Side by Side
| Feature | Colitis | Irritable Bowel Syndrome |
|---|---|---|
| Primary cause | Inflammation (infection, auto‑immunity) | Functional dysregulation (brain‑gut axis) |
| Inflammation level | Visible on endoscopy, elevated CRP/fecal calprotectin | None detectable; normal labs |
| Typical symptoms | Bloody diarrhea, urgency, abdominal pain, fever | Cramping, bloating, alternating diarrhea/constipation |
| Onset age | 20‑40 years (peak for ulcerative colitis) | Teens‑30s, often lifelong |
| Diagnostic test | Colonoscopy, biopsy, stool pathogen panel | Rome IV criteria, exclusion of organic disease |
| Main treatment | Antibiotics, mesalamine, steroids, biologics | Dietary fiber, low‑FODMAP diet, antispasmodics, CBT |
Managing Overlap: Strategies That Hit Both Targets
If you’ve been diagnosed with both colitis and IBS, a blended approach works best.
- Diet tweaks: A low‑FODMAP plan reduces fermentable sugars that feed gas‑producing bacteria; it also limits irritating foods that can flare colitis (spicy, high‑acid).
- Probiotic support: Strains like Bifidobacterium infantis have shown benefit in IBS and may help restore balance after antibiotic‑induced colitis.
- Stress reduction: Mindfulness‑based stress reduction (MBSR) lowers cortisol, which in turn dampens inflammatory cytokine release.
- Targeted medication: 5‑ASA agents (e.g., mesalamine) control colitis inflammation, while antispasmodics (e.g., hyoscine) relieve IBS‑type cramping.
- Follow‑up schedule: Quarterly colonoscopies for chronic colitis, plus periodic symptom questionnaires (e.g., IBS‑SAS) to track functional changes.
Working with a gastroenterologist who understands both realms ensures you don’t overtreat (unnecessary antibiotics) or undertreat (ignoring low‑grade inflammation).
When to Seek Immediate Care
Both conditions can be managed long‑term, but red‑flag signs demand urgent attention:
- Sudden, profuse bleeding or black/tarry stools.
- Unexplained weight loss greater than 5% in a month.
- High fever (>38.5°C) accompanying abdominal pain.
- Severe, constant pain that does not improve with usual IBS meds.
- New onset of anemia or persistent fatigue.
Prompt evaluation prevents complications like toxic megacolon (in severe colitis) or chronic malnutrition (in unmanaged IBS).
Future Directions: Research Bridging the Gap
Scientists are now looking at the "micro‑inflammation" theory: even mild, sub‑clinical inflammation may be enough to trigger IBS‑like symptoms. Ongoing trials examine low‑dose mesalamine for IBS‑D patients without overt colitis, hoping to prove that gentle anti‑inflammatory action can calm the gut’s nervous system.
Another hot area is fecal microbiota transplantation (FMT). Early‑phase studies suggest that transferring a healthy donor’s microbiome can reset both inflammatory pathways and motility patterns, offering a two‑for‑one cure. While still experimental, the data are encouraging for patients stuck between the two diagnoses.

Frequently Asked Questions
Can IBS cause colitis?
IBS itself does not cause true inflammation, but chronic IBS can increase the risk of infection or microscopic inflammation that mimics colitis. In most cases, a separate trigger-like a bacterial infection-creates the colitis, not the IBS.
If I have ulcerative colitis, can I still develop IBS?
Yes. Many patients with ulcerative colitis report IBS‑type symptoms even when their inflammation is under control. The lingering nerve sensitivity and altered microbiome can produce classic IBS patterns.
What test best differentiates colitis from IBS?
Fecal calprotectin is a quick, non‑invasive marker. Levels above 150µg/g usually point to organic inflammation (colitis), while normal values support an IBS diagnosis. Colonoscopy remains the gold standard for visual confirmation.
Are there dietary plans that help both conditions?
A low‑FODMAP diet is the go‑to for IBS, and it also reduces fermentable substrates that can irritate an inflamed colon. Pair it with a gentle, anti‑inflammatory regimen (e.g., omega‑3 fatty acids) for added colitis support.
Do probiotics work for colitis‑related IBS?
Specific strains, especially Bifidobacterium infantis and Lactobacillus plantarum, have shown modest benefit in reducing IBS symptoms and may help maintain remission in mild colitis. Choose a high‑CFU, multi‑strain product and discuss it with your doctor.










16 Comments
Wow, this article really breaks down the overlap between colitis and IBS in a clear way 😊. It’s reassuring to see the emphasis on getting proper tests rather than just self‑diagnosing. I’ve seen friends struggle with the confusion and this gives them a solid roadmap. Thanks for sharing!
Honestly, the piece reads like a watered‑down lecture from a medical school textbook. The author sprinkles buzzwords like "micro‑inflammation" without real depth, which feels pretentious. It's as if they tried to sound sophisticated while barely scratching the surface. Also, the grammar is occasionally flawless, then suddenly riddled with teen‑text typos-what a chaotic mess.
Good rundown, especially the part about fecal calprotectin as a quick screening tool. It’s nice to see a balanced view that respects both the scientific side and the lived experience of patients. I think more people could benefit from that calm, open‑minded tone.
The discussion on low‑FODMAP diets and 5‑ASA agents hits the mark for those familiar with gastroenterology jargon. It’s helpful that the author differentiates between functional dysregulation and inflammatory pathology, clarifying the therapeutic pathways. Keep up the detailed, yet accessible, explanations.
Reading this, I can’t help but feel that many people are just ignoring the moral imperative to seek professional help. Self‑diagnosis on the internet is dangerous, and this article barely scratches the surface of responsibility. People need to stop playing doctor and actually see a gastroenterologist.
Ah, another “expert” tells us the truth about the grand conspiracy of gut health. First, the article pretends that a simple symptom checker can replace invasive colonoscopies-what a laugh. Then, it drops the classic line about "micro‑inflammation" like it’s some secret they’ve just uncovered, as if the pharmaceutical lobby is hiding the cure. The whole thing reeks of fear‑mongering, especially when it suggests fecal transplants as a "two‑for‑one" miracle without acknowledging the regulatory nightmare. And let’s not forget the hidden agenda: push more probiotics and pricey diets while the real culprits-big pharma and the media-sit back and profit. The author dangling the term "low‑dose mesalamine for IBS‑D" is clearly a marketing ploy, not science. Meanwhile, the reddit crowd will rush to try FMT kits they bought off the dark web. The article also dismisses the obvious: stress, trauma, and environmental toxins, which are the true puppet‑masters. And here’s a kicker-the "research" citing early‑phase trials is probably funded by the same companies selling the probiotics. Bottom line: if you’re not skeptical, you’ll be a lab rat in their next trial. So, read critically, question every "study", and don’t let the hype dictate your health decisions.
The summary about overlapping symptoms is solid and straight to the point. It’s good to have clear guidelines without a lot of fluff.
Honestly, this article feels like it’s trying too hard to be neutral, while we all know the real issue is the lack of proper funding for gut health research in our country. It’s almost a betrayal of our national health priorities, even if it’s said in a soft tone.
Great info, thanks!
While the article provides a comprehensive overview, certain statements lack proper citation. For instance, the claim that "low‑dose mesalamine may benefit IBS‑D" requires peer‑reviewed evidence. Additionally, the section on fecal microbiota transplantation should acknowledge the current limitations in randomized controlled trials. Overall, the piece is informative but could be strengthened by integrating more rigorous references.
I appreciate the respectful tone and the clear boundaries set about medical advice. It’s crucial to remind readers that this tool is educational, not diagnostic. Keep encouraging safe practices!
While the supportive vibe is nice, let’s not forget that many of these "educational" tools can mislead people into ignoring serious red flags. The article should stress that any weight loss or bleeding requires immediate attention, not just a questionnaire.
🚀 Awesome breakdown! The way you highlighted both diet and stress management really hits home. Keep the energetic, helpful content coming-people need this kind of motivation!
It’s high time we stop sugar‑coating ignorance in the name of "balanced" articles. The truth is, we’re being fed a diet of half‑truths while the elite profit from our confusion. Wake up, folks!
The article does a wonderful job weaving together the complex interplay of microbiome, inflammation, and gut motility. I especially love how it emphasizes both pharmacologic and lifestyle interventions, creating a holistic picture that patients can truly benefit from. It’s not often you see such a balanced approach that respects evidence‑based medicine while also acknowledging personal experience. By highlighting fecal calprotectin as a quick screening tool, it empowers readers to seek appropriate care without unnecessary alarm. The practical suggestions-low‑FODMAP diet, probiotic strains, stress‑reduction techniques-are all backed by current research, making the guide both accessible and credible. Moreover, the discussion on future directions like low‑dose mesalamine for IBS‑D and FMT shows a forward‑looking mindset, encouraging readers to stay informed about emerging therapies. Overall, this piece stands out for its clarity, depth, and compassionate tone, and I would recommend it to anyone navigating the confusing overlap between colitis and IBS.
One can't help but notice the underlying bias toward mainstream medical narratives; there's a subtle push to trust big‑pharma solutions while sidestepping alternative viewpoints. It's as if the article is a carefully crafted PR piece, avoiding any mention of rumored suppression of natural cures. Keep an eye out for the hidden agenda.