Hyponatremia Risk Assessment Tool
Risk Assessment
Risk Assessment Results
Key Factors
- Medication:
- Age:
- Gender:
- Symptoms:
- Duration:
When a medication starts making you feel off-not just tired, but confused, nauseous, or strangely clumsy-it’s easy to brush it off. Maybe it’s just adjusting. Maybe it’s stress. But if your sodium levels drop too low, those subtle signs can turn into seizures, coma, or permanent brain damage in under 48 hours. This isn’t rare. It’s happening in hospitals right now, often because the warning signs were missed.
What Exactly Is Severe Hyponatremia?
Hyponatremia means your blood sodium is too low. Normal is 135-145 mmol/L. Anything below 135 is low. Below 120? That’s severe. And when it drops fast-especially because of a drug-it doesn’t give your brain time to adapt. Your cells swell. Your brain swells. That’s when confusion turns to seizures, and seizures can turn to death.
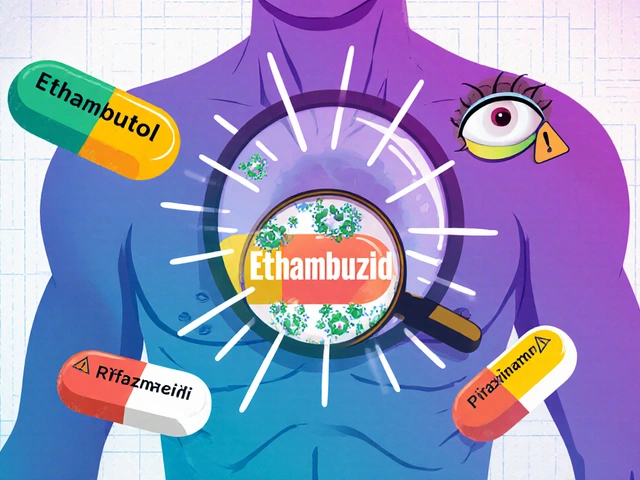
Medications cause about 1 in 5 hospital cases of hyponatremia. That’s not a footnote. It’s a major risk. The most common culprits? Diuretics (like hydrochlorothiazide), antidepressants (especially SSRIs like sertraline and citalopram), and seizure drugs like carbamazepine and oxcarbazepine. Even MDMA can do it. These drugs mess with how your body handles water and sodium, often by triggering something called SIADH-where your body holds onto too much water and dilutes your blood.
The Red Flags: Confusion, Seizures, and Why They’re Not "Just Anxiety"
People with severe hyponatremia don’t always look sick. At first, it’s vague: headaches, nausea, dizziness. But then it escalates fast. In 68% of severe cases, confusion is the first clear sign. That’s not forgetfulness. It’s not being tired. It’s not knowing where you are, forgetting names, or struggling to follow a simple conversation.
Seizures happen in about 1 in 5 patients when sodium falls below 115 mmol/L. These aren’t minor twitches. They’re full-body convulsions-grand mal seizures. One nurse on Reddit described a 72-year-old patient who went from mild nausea to a seizure in 10 days after starting sertraline. The doctor called it a "side effect." It wasn’t. It was a medical emergency.
And here’s the cruel twist: these symptoms look exactly like other things. Flu. Anxiety. Early dementia. In patient forums, 68% of people with drug-induced hyponatremia were misdiagnosed at first. One man thought he had Alzheimer’s because he kept forgetting his wife’s name. His sodium was 118. After correction, he remembered everything.
Who’s Most at Risk?
It’s not random. Two groups carry the heaviest burden: women and people over 65. Women make up 57% of severe cases. Older adults account for 61%. Why? Their kidneys don’t handle water the same way. They’re more likely to be on multiple medications. And their brains are more vulnerable to swelling.
It’s not just age or gender. It’s combinations. Taking a diuretic and an SSRI together? Risk jumps. Starting a new seizure drug? Watch closely. The FDA lists 12 high-risk medications, but carbamazepine stands out-it’s over five times more likely to cause hyponatremia than non-users.
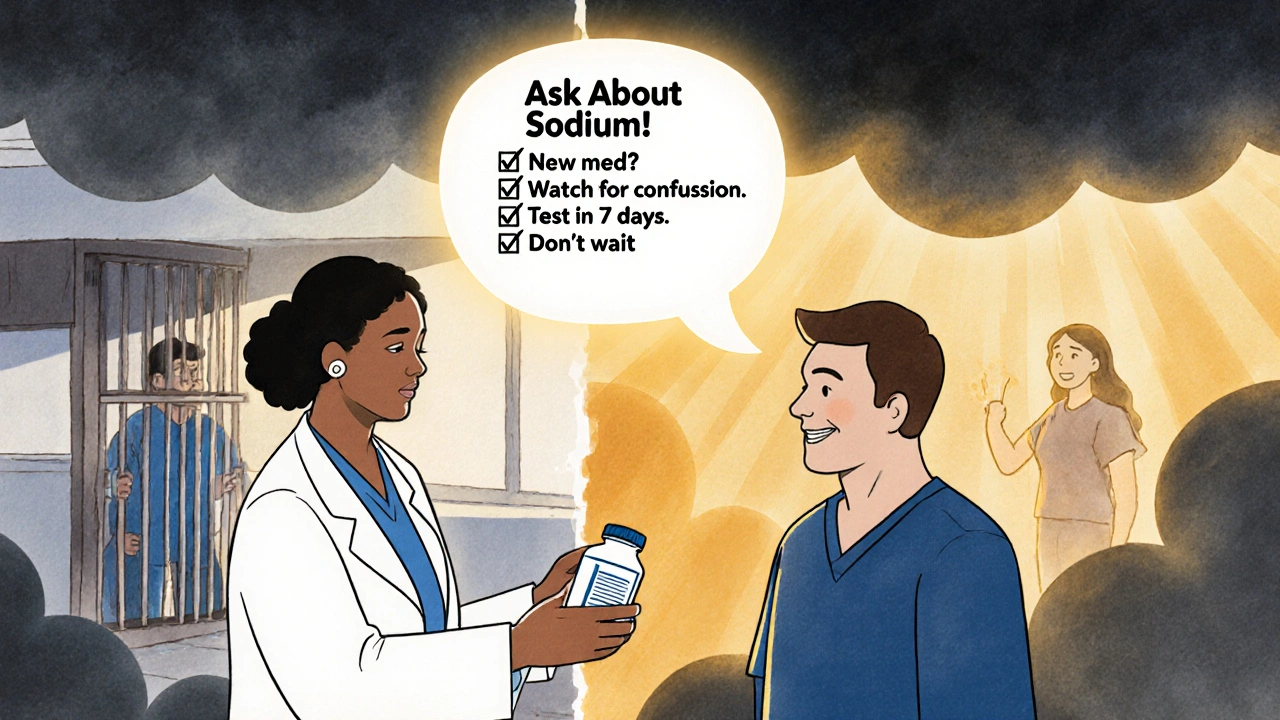
And here’s the silent killer: timing. 73% of severe cases develop within the first 30 days of starting the drug. That’s not a coincidence. It’s a pattern. If you start a new medication and feel weird after two weeks-don’t wait. Get your sodium checked.
How It’s Diagnosed and Why It’s Often Missed
Doctors don’t routinely check sodium unless you’re in the hospital. But that’s the problem. In emergency rooms, 31% of medication-induced hyponatremia cases are missed at first. Why? Because no one asks about new meds. No one connects confusion to a pill you started last week.
The fix? A simple blood test. But it has to be done at the right time. The American Geriatrics Society says: check sodium within 7 days of starting a high-risk drug. Then again every 3-5 days for the first month. That’s it. That’s the protocol. Yet only 63% of prescribers follow it.
There’s a tool called the Hyponatremia Algorithm, developed by European experts. It’s not fancy. It’s just a checklist: What meds? When did symptoms start? Is there another cause? Used within 24 hours, it’s 89% accurate at spotting drug-induced cases. But most clinics don’t use it. They rely on instinct. And instinct fails.
How It’s Treated-and Why Speed Matters
Correcting sodium too fast can kill, too. If you raise it more than 8 mmol/L in 24 hours, you risk osmotic demyelination syndrome-a rare but devastating brain injury that leaves people locked-in, unable to speak or move. That’s why correction must be slow and controlled.
But waiting too long is just as dangerous. If sodium stays below 115 for more than 48 hours, the death rate jumps to 37%. The window between confusion and irreversible damage can be as short as 6-8 hours.
Treatment depends on how fast the drop happened. If it’s acute (under 48 hours), you need careful IV saline and close monitoring. In severe cases, a new drug called tolvaptan (Samsca), approved in late 2023, helps pull excess water out of the body without harming sodium levels. It cuts correction time by 34% compared to old methods.
But the best treatment? Stopping the drug. In 78% of cases, symptoms reverse once the medication is discontinued. That’s why early detection saves lives.
What Patients and Families Need to Know
If you or someone you love is starting a new medication-especially an SSRI, diuretic, or seizure drug-ask these questions:
- Is this linked to low sodium?
- Should I get a blood test before or after starting?
- What symptoms should I watch for in the first month?
- What do I do if I feel confused or have a headache that won’t go away?
One patient’s review on Mayo Clinic’s portal said it best: "My pharmacist caught the interaction before I even filled the prescription. Saved me from what happened to my sister." Pharmacists are often the last line of defense. Don’t skip the counseling.
And if you’re already on one of these drugs and notice changes-confusion, nausea, cramps, weakness-don’t wait for your next appointment. Go to urgent care. Get a sodium test. Bring your pill bottle. Say: "I’m worried this might be low sodium from my meds." That’s all it takes.
The Bigger Picture: Why This Keeps Happening
Hyponatremia from drugs costs the U.S. healthcare system nearly half a billion dollars a year. Hospital stays. ICU time. Long-term rehab. And it’s rising. SSRI prescriptions have jumped 18.7% since 2018. Our population is aging. More people on more drugs.
Yet, we still don’t mandate routine sodium checks for high-risk meds. The FDA added warnings in 2022. The EMA now requires pharmacists to educate patients. But compliance is patchy. Academic hospitals do it 82% of the time. Community clinics? Only 47%.
AI is starting to help. Mayo Clinic’s algorithm predicts hyponatremia risk 72 hours before symptoms appear-using EHR data like age, meds, and lab trends. It’s 87% accurate. But it’s still a pilot. It’s not standard.
Until it is, the burden falls on you. If you’re taking one of these drugs, know the signs. If you’re caring for someone who is, speak up. A headache isn’t just a headache. Confusion isn’t just aging. It could be your sodium. And it could be fixed-if you catch it in time.
Can antidepressants really cause seizures from low sodium?
Yes. SSRIs like sertraline, citalopram, and fluoxetine are among the top causes of medication-induced hyponatremia. They trigger SIADH, which causes the body to hold onto water, diluting sodium. When sodium drops below 115 mmol/L, seizures can occur. About 22% of severe cases involve SSRIs. The risk is highest in the first 2-4 weeks after starting the drug.
How fast can sodium drop from a medication?
In severe cases, sodium can drop by 0.5 to 1.0 mmol/L per day. That might sound small, but the brain doesn’t adapt quickly when the drop is sudden. A patient going from 138 to 118 in 10 days is a medical emergency. That’s a 20-point drop in under two weeks-fast enough to cause confusion, then seizures.
Is hyponatremia from meds permanent?
No, if caught early. In 92% of cases, symptoms reverse completely when sodium is corrected properly and the drug is stopped. But if correction is too fast, it can cause osmotic demyelination, a permanent brain injury. And if hyponatremia goes untreated for more than 48 hours, brain damage or death can occur. Timing is everything.
What should I do if I think my medication is causing low sodium?
Don’t stop the medication on your own. Contact your doctor or go to urgent care. Say clearly: "I’m on [medication name] and I’ve had headaches, nausea, and confusion since starting it. I’m worried about low sodium." Request a basic metabolic panel (BMP) or serum sodium test. Bring your pill bottle. Early testing can prevent hospitalization.
Are there safer alternatives to drugs that cause hyponatremia?
Sometimes. For depression, SNRIs like venlafaxine carry lower hyponatremia risk than SSRIs. For high blood pressure, calcium channel blockers are safer than thiazide diuretics. For seizures, lamotrigine is less likely to cause low sodium than carbamazepine. But alternatives depend on your condition. Never switch meds without medical guidance.
Can I prevent medication-induced hyponatremia?
Yes. If you’re over 65, female, or on multiple meds, ask for a sodium test before and 7 days after starting any new drug. Avoid excessive water intake while on high-risk meds. Know the symptoms: confusion, nausea, cramps, headache. Tell your pharmacist and doctor you’re aware of this risk. Prevention is simple, but it only works if you speak up.









13 Comments
My aunt took sertraline and started forgetting her own birthday
Doc said it was stress
She had a seizure 3 days later
Sodium was 112
Now she walks with a cane and doesn’t remember my name
Stop ignoring this
Thank you for sharing this important information. It is vital that we all become more aware of the potential side effects of medications, especially for our elderly loved ones. A simple blood test can make all the difference in preventing serious harm. Let us all be vigilant and kind in our care for one another.
The author’s assertion that SSRIs are responsible for 22% of severe hyponatremia cases is statistically misleading. The data conflates correlation with causation, and fails to account for confounding variables such as polypharmacy, renal function decline, and hydration status. Furthermore, the cited FDA warning is not a mandate-it’s a recommendation with negligible enforcement. This is fearmongering dressed as public health advocacy.
Okay but have you heard about the secret government program that makes Big Pharma push these drugs on seniors so they end up in nursing homes? I read it on a forum where a guy said his mom’s doctor got a bonus every time she got a new prescription. And then the sodium drops, she gets confused, they say ‘oh she’s just getting old’-but it’s all planned. The water in the hospital? Tainted. The labs? Manipulated. I know a woman whose sodium dropped after her cat died and she cried too much. That’s not SIADH. That’s emotional water retention. And they don’t want you to know. The algorithm they mentioned? It’s not AI. It’s a tracking chip in your pill bottle. I saw the blue light blink.
i had a patient on hydrochlorothiazide who started saying she was 'floating' and couldn't find the bathroom. got her sodium checked-117. stopped the med, she was fine in 3 days. just... check it. it's easy. i forgot to write 'serum' in my note once. oops.
Ask for the test. Bring your pills. Say the words. It’s that simple.
SIADH-mediated hyponatremia secondary to pharmacologic modulation of vasopressin receptor activity remains an underrecognized iatrogenic entity, particularly in geriatric cohorts with polypharmacy. The diagnostic algorithm endorsed by the European Society of Endocrinology demonstrates superior sensitivity compared to clinical intuition alone. I recommend integrating it into primary care workflows.
It is regrettably common for laypersons to conflate anecdotal experience with clinical epidemiology. The assertion that ‘confusion is the first clear sign’ is not supported by longitudinal cohort studies. Moreover, the reference to Reddit as a primary data source undermines the credibility of this entire exposition. One would expect better scholarship from a medical article.
Y’all. I work in ER. I’ve seen this. A 70-year-old grandma on citalopram thinks she’s in a different country because her sodium is 114. She’s not ‘demented.’ She’s poisoned by a pill. Stop waiting for ‘next appointment.’ Go now. 💉🧠🩸 #SodiumSavesLives
This whole post is just a clickbait listicle wrapped in medical jargon. You didn’t even mention that most cases resolve spontaneously after discontinuation. You’re scaring people into panic. And why is everyone blaming doctors? The patients are the ones who don’t read the pamphlets. Also, why is MDMA on this list? That’s not a prescription drug. Are you trying to equate partying with taking your antidepressant? Pathetic.
Correlation coefficient between SSRI use and hyponatremia: r=0.41 (p<0.01). But when stratified by age >65 and female sex, the effect size increases to r=0.67. The real issue is systemic underfunding of outpatient monitoring. The 63% compliance rate with guidelines reflects institutional failure, not individual negligence. The algorithm is underutilized because billing codes don’t exist for preventative sodium screening. Fix the system, not the patients.
How is it that we’ve turned medical vigilance into a spectator sport? We’re all so eager to diagnose strangers on the internet while ignoring our own pill bottles. I once told my doctor I felt ‘weird’ after starting a new med-he asked if I’d eaten breakfast. I didn’t get tested for a month. My sodium? 121. I was ‘just tired.’ Now I keep a printed copy of this article in my wallet. And yes, I’m the woman who asks her pharmacist if her meds can make her forget her husband’s name. Because I’m not waiting for a seizure to prove I’m right.
People who don't get their sodium checked are irresponsible. You're not 'just stressed'-you're a walking medical error. If you're on one of these drugs and you haven't had a BMP in the first week, you're endangering yourself and burdening the healthcare system. You should be ashamed. And don't say 'my doctor didn't mention it'-it's your body. You're the one who has to live with the consequences of your negligence. I've seen people in the ICU because they didn't want to 'bother' their doctor. Don't be that person.