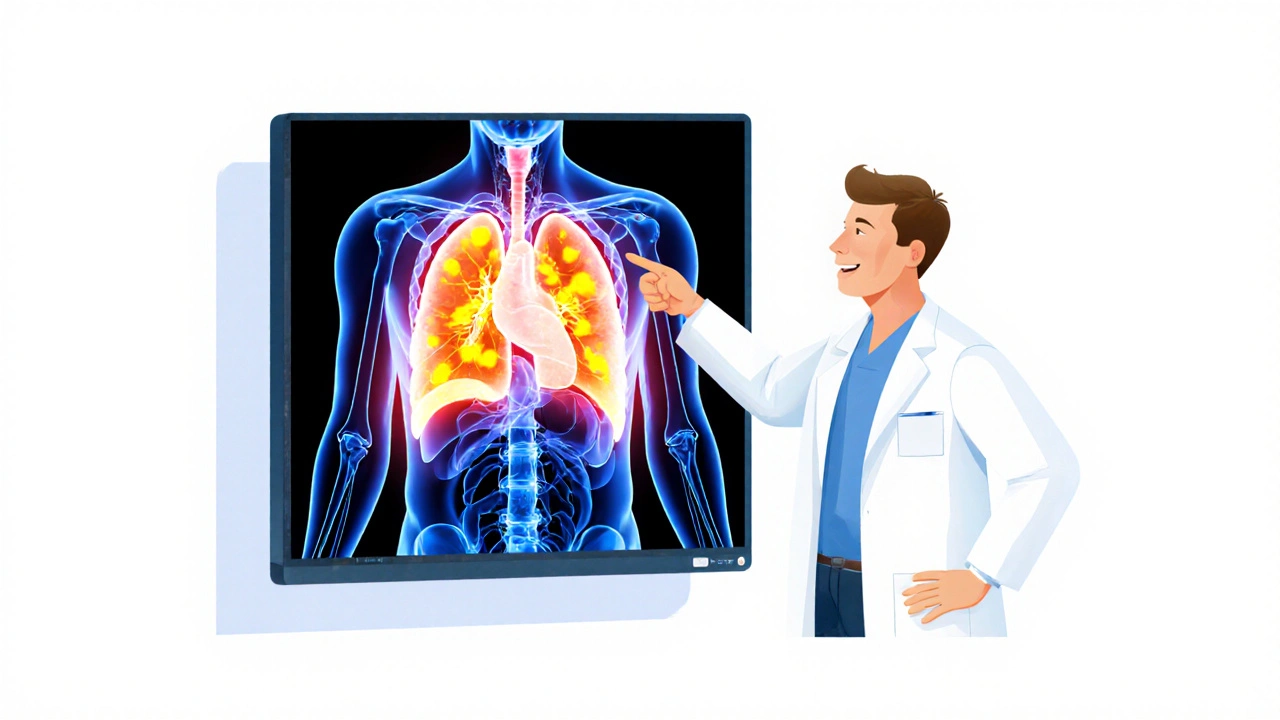
When a doctor suspects cancer, the first real question isn’t just whether it’s there-it’s how far it’s spread. That’s where imaging becomes life-changing. PET-CT, MRI, and PET-MRI aren’t just fancy machines; they’re the tools that tell oncologists if a tumor is still local, if it’s reached the lymph nodes, or if it’s jumped to the liver or bones. The difference between accurate staging and a misread scan can mean the difference between a cure and a last-resort treatment plan.
Why Staging Accuracy Matters More Than You Think
Cancer staging isn’t a label-it’s a roadmap. Stage I means early, localized, often curable. Stage IV means widespread, usually requiring systemic therapy. Get it wrong, and you might skip surgery that could’ve cured someone, or push a patient into aggressive chemo they don’t need. That’s why imaging accuracy isn’t just technical-it’s ethical. The old way relied on CT scans alone. They showed size and shape, but not whether a lymph node was truly cancerous or just swollen from infection. PET-CT changed that by showing metabolism. Cancer cells burn sugar like crazy, so when you inject a radioactive glucose tracer (18F-FDG), they light up on the scan. Combine that with the detailed anatomy from CT, and you get a picture of both structure and activity. That’s why, since 2001, PET-CT became the default for lung, colorectal, and lymphoma staging.PET-CT: The Workhorse of Oncology Imaging
Most hospitals still rely on PET-CT because it’s fast, widely available, and proven. A typical scan takes 15 to 20 minutes. Patients get a small dose of 18F-FDG-about 370 MBq-and wait an hour for it to circulate. Then they’re scanned from head to toe. The radiation dose? Around 10 to 25 mSv, depending on the protocol. That’s equivalent to 3 to 8 years of natural background radiation, but the benefit usually outweighs the risk. For non-small cell lung cancer, PET-CT correctly identifies spread to lymph nodes in 84% of cases. In melanoma, it finds hidden metastases in 30% of patients who looked clear on CT alone. It’s also the go-to for checking if treatment is working. If a tumor’s metabolic activity drops after chemo, that’s a good sign-even if it hasn’t shrunk yet. But PET-CT has limits. It’s bad at spotting small tumors in organs with high background uptake, like the liver or brain. It also can’t tell the difference between scar tissue and active cancer after radiation. And it uses ionizing radiation-something you don’t want to repeat often, especially in younger patients.MRI: The Soft-Tissue Champion
MRI doesn’t use radiation. Instead, it uses powerful magnets and radio waves to map water molecules in tissues. That makes it unbeatable for seeing soft tissue detail-brain tumors, prostate cancer, liver lesions, and pelvic cancers. A 3T MRI machine can resolve structures as small as 0.5 mm. That’s why it’s the gold standard for prostate cancer staging: it shows if the tumor has broken through the prostate capsule or invaded nearby nerves. In breast cancer, MRI detects additional tumors in 15-20% of patients who seemed to have a single lesion on mammogram or ultrasound. For rectal cancer, it tells surgeons exactly how deep the tumor has grown into the wall and whether nearby lymph nodes are involved-critical for deciding if you need chemo before surgery. But MRI doesn’t show metabolism. A swollen lymph node could be cancer… or infection. A dark spot in the liver could be tumor… or a benign cyst. That’s where MRI alone can mislead. That’s why, for many cancers, it’s paired with PET.
PET-MRI: The Hybrid Advantage
PET-MRI came onto the scene in 2011, combining the metabolic power of PET with the soft-tissue clarity of MRI in a single scan. No more two separate appointments. No more misalignment between scans taken days apart. The result? Better accuracy where it matters most. In brain tumors, PET-MRI can distinguish between radiation necrosis and tumor recurrence with 85-90% accuracy-something MRI alone struggles with at 70-80%. In prostate cancer, when you combine PSMA-targeted PET with multiparametric MRI, you catch more aggressive tumors than either modality alone. A 2023 study found that PET-MRI changed treatment plans for nearly half of pancreatic cancer patients because it revealed hidden spread that PET-CT missed. It’s also the best choice for pediatric patients and young adults. Since it cuts radiation exposure by about 50% compared to PET-CT, it reduces long-term cancer risk from repeated scans. For someone with Lynch syndrome or BRCA mutations who needs yearly monitoring, that matters. But PET-MRI isn’t perfect. It’s slower-45 to 60 minutes per scan. Motion from breathing or bowel movement can blur the image. It’s also more expensive: $2,500 to $3,500 per scan versus $1,600 to $2,300 for PET-CT. And not every hospital has it. Only 22% of U.S. cancer centers have PET-MRI, mostly in academic hospitals with research programs.Which Scan for Which Cancer?
There’s no one-size-fits-all. Here’s how experts choose:- Lung cancer: PET-CT is standard for initial staging. MRI is added only if brain metastasis is suspected.
- Prostate cancer: Multiparametric MRI is first-line. PSMA PET-MRI is used for high-risk cases or when PSA rises after treatment.
- Breast cancer: MRI for high-risk screening and pre-op planning. PET-CT for advanced disease. PET-MRI shows promise in evaluating response to neoadjuvant chemo.
- Pancreatic cancer: PET-MRI is gaining ground because it finds small liver lesions and assesses vascular involvement better than PET-CT.
- Lymphoma: PET-CT remains king for staging and response assessment. PET-MRI is being studied for cases where bone marrow involvement is unclear.
- Brain tumors: PET-MRI is the clear winner. It shows tumor boundaries, metabolic activity, and differentiates recurrence from treatment effects.
- Pediatric cancers: PET-MRI is preferred whenever possible to avoid unnecessary radiation.

What’s Holding PET-MRI Back?
The technology is better-but adoption is slow. Why? First, cost. A PET-MRI machine runs $3 to $4.2 million. A PET-CT? $1.8 to $2.5 million. Add in the shielded room, maintenance, and specialized staff, and the ROI takes years. Second, workflow. Scans take longer. Radiologists need extra training to interpret both PET and MRI data together. A 2022 survey found 63% of sites struggled with PET-MRI’s attenuation correction artifacts-errors in how the scanner measures tissue density that can distort the PET image. Third, reimbursement. Insurance companies often don’t cover PET-MRI unless PET-CT was inconclusive. Many centers only use it for research or complex cases. But things are shifting. Siemens launched a new BioMatrix 600 system in early 2024 with a 6-minute whole-body scan time-cutting scan duration nearly in half. AI tools are now helping automate tumor detection and quantification. The NCI’s PREDICT trial is testing whether AI can predict treatment response from PET-MRI data before the patient even finishes chemo.The Future Is Personalized
The next big leap isn’t just better machines-it’s smarter decisions. The 2024 ASCO guidelines now recommend imaging choices based on tumor biology. For example, triple-negative breast cancer responds better to PET-CT early in treatment, while hormone-receptor-positive tumors show more value with MRI for monitoring. New radiotracers are coming too. PSMA for prostate cancer, DOTATATE for neuroendocrine tumors, and even tracers targeting specific mutations are being tested. These will let us see not just where the cancer is, but what kind it is. The goal isn’t to replace PET-CT. It’s to use the right tool for the right patient. For most, PET-CT is still the best first step. For complex cases, children, or when you need to know if a liver spot is cancer or scar tissue-PET-MRI is becoming indispensable.What Patients Should Know
If you’re facing cancer imaging, ask:- What’s the goal of this scan-finding cancer, checking spread, or seeing if treatment worked?
- Is there a reason to choose MRI or PET-MRI over PET-CT in my case?
- Will this scan expose me to radiation? How many times will I need it?
- Will the results change my treatment plan?
Which imaging test is most accurate for cancer staging?
There’s no single answer-it depends on the cancer type. PET-CT is the most widely used and accurate for lung, colorectal, and lymphoma staging. MRI is superior for prostate, breast, and brain cancers due to its soft-tissue detail. PET-MRI offers the highest accuracy in complex cases, like distinguishing tumor recurrence from scar tissue in the brain or detecting small liver metastases, but it’s not always necessary or available.
Is PET-MRI better than PET-CT for all cancers?
No. PET-MRI is better for specific cancers like brain tumors, prostate cancer, and pediatric cancers, where soft-tissue contrast and reduced radiation matter most. For most lung or lymphoma cases, PET-CT remains the standard because it’s faster, cheaper, and just as accurate. PET-MRI doesn’t replace PET-CT-it complements it in select situations.
Does MRI detect cancer better than CT?
MRI detects cancer better than CT in soft tissues-like the brain, prostate, liver, and pelvic organs-because it shows differences in tissue water content and structure. CT is better for bones, lungs, and quick scans. But neither shows metabolic activity. That’s why PET is often added: to see if a suspicious area is actually cancerous based on how much sugar it’s consuming.
How much radiation do these scans expose me to?
A standard PET-CT scan delivers 10 to 25 mSv of radiation-similar to 3 to 8 years of natural background exposure. MRI uses no ionizing radiation at all. PET-MRI reduces radiation by about half compared to PET-CT because it replaces the CT component with MRI. For patients needing multiple scans over time, especially children and young adults, this reduction matters.
Why isn’t PET-MRI used everywhere if it’s more accurate?
Cost and access. PET-MRI machines cost over $3 million, require special shielding, and take longer to scan. Fewer than a quarter of U.S. cancer centers have them. Insurance often won’t pay unless PET-CT was inconclusive. Plus, interpreting PET-MRI requires specialized training. So while it’s superior in key cases, it’s not practical for routine use.
Can AI improve cancer staging with these scans?
Yes. AI is already being used to detect tumors faster, measure changes in tumor size and metabolism more precisely, and predict how a tumor will respond to treatment based on imaging patterns. The NCI’s PREDICT trial is testing whether AI can use PET-MRI data to predict treatment success before the patient even finishes chemo. This could one day make staging not just accurate-but predictive.


12 Comments
Okay, but let’s be real-PET-CT is the OG of cancer staging, and nobody’s gonna replace it with a $4M MRI hybrid that takes an hour and makes your butt numb. I’ve seen scans where the tech had to reposition the patient three times because they sneezed. Meanwhile, PET-CT? Boom, done, next.
Also, the radiation? Yeah, it’s a lot-but so is dying from stage IV you didn’t know about. We’re not talking about a weekend MRI for a sprained ankle here. This is life-or-death math.
PSMA-PET-MRI for prostate: 92% sensitivity. PET-CT: 78%. But access? 0.2% in Global South. This is precision medicine for the 1%.
AI-driven quantification? Nice. But who labels the data? Western radiologists. Bias embedded. You’re not fixing disparity-you’re automating it.
Y’all need to stop treating imaging like a menu at Applebee’s. ‘I’ll have the PET-CT with extra radiation and a side of CT contrast.’ No. This isn’t about what’s cheaper or faster-it’s about what saves the person in front of you.
I had a cousin with recurrent glioblastoma. PET-CT said ‘stable.’ PET-MRI showed active tumor growth in the frontal lobe-hidden under scar tissue. Surgeon changed the plan. She’s alive three years later. That’s not data. That’s a miracle wrapped in magnets and isotopes.
And yes, the cost is insane. But if we’re spending $100k on a chemo regimen that fails because we missed a 3mm lesion-then we’re just wasting money on ignorance.
Stop thinking about budgets. Start thinking about lives. The tech isn’t the problem. Our priorities are.
Let’s not pretend this isn’t a luxury product masquerading as medical advancement. The U.S. spends 18% of GDP on healthcare and still can’t get basic CT scanners to rural clinics. Now we’re funding $4M PET-MRI machines in Manhattan while Nigeria waits for its first MRI in 15 years?
This isn’t innovation-it’s performative medicine. The real breakthrough would be getting basic diagnostics to 8 billion people. Not giving Silicon Valley billionaires another shiny toy.
ok so like… PET-MRI is the new iphone 16 pro ultra max but like… why do i need it if my doc just wants to know if the cancer spread??
also who even has time to sit for 60 mins?? my dog gets more anxious than i do during a car ride lol
and the cost?? my insurance denied it bc ‘not medically necessary’… so now i’m paying $2k out of pocket for a scan that might change nothing??
also why do all the studies come from ‘academic centers’?? like… are we just pretending this tech exists in the real world??
also who wrote this?? it reads like a pharma ad with footnotes.
I get it-tech is cool. But I’ve seen families torn apart because they had to choose between paying for a PET-MRI or keeping the lights on. No one talks about that part.
Maybe the real question isn’t which scan is better-but how do we make the good ones available to everyone, not just those with good insurance or living near a university hospital?
Also, thank you for writing this. It’s rare to see something so detailed that doesn’t make me feel dumb for not knowing all this.
It is imperative to underscore that the integration of metabolic and anatomical modalities represents a paradigm shift in oncologic diagnostics. The convergence of positron emission tomography with magnetic resonance imaging facilitates a synergistic elucidation of tumor biology and microenvironmental dynamics, thereby enhancing diagnostic precision beyond the limitations of either modality in isolation.
Furthermore, the attenuation correction challenges inherent in PET-MRI systems necessitate rigorous calibration protocols to mitigate quantitative inaccuracies in standardized uptake value measurements, which may compromise therapeutic decision-making if unaddressed.
It is therefore incumbent upon healthcare institutions to invest in multidisciplinary training programs to ensure radiologists are proficient in dual-modality interpretation, thereby maximizing clinical utility while minimizing diagnostic ambiguity.
One cannot help but observe the alarming disparity between the rate of technological advancement in oncologic imaging and the stagnation of reimbursement policy. The Centers for Medicare & Medicaid Services continue to classify PET-MRI as investigational for the majority of indications, despite robust peer-reviewed evidence demonstrating improved diagnostic accuracy and downstream cost savings through avoided unnecessary interventions.
Moreover, the assertion that PET-MRI is ‘not always necessary’ is a dangerous oversimplification. In cases of biochemical recurrence following prostatectomy, where PSA levels are rising but conventional imaging is negative, PET-MRI with PSMA tracer is not merely ‘better’-it is the only modality capable of identifying oligometastatic disease amenable to curative-intent therapy.
The failure to adopt evidence-based imaging protocols is not a logistical issue-it is a systemic failure of medical ethics.
I just want to say thank you to whoever wrote this. I’m a nurse and I’ve seen too many patients scared because they don’t understand what scan they’re getting or why. This breaks it down so clearly.
Also, to the person who said PET-MRI is just for rich people? I’ve had patients who drove 3 hours to get one because their oncologist said it was their best shot. They didn’t have money-but they had hope. And that matters.
What if the real question isn’t ‘which scan is most accurate’-but ‘who gets to decide what accuracy means?’
Is accuracy just about detecting more tumors? Or is it about avoiding harm-over-treating, over-radiating, over-analyzing?
Maybe the most ethical scan is the one that doesn’t get ordered at all-if the risk outweighs the benefit.
We’ve turned cancer into a puzzle to solve with machines. But sometimes, the most human thing we can do is sit with uncertainty-and choose compassion over clarity.
AI will fix everything. Just wait.
Given the high specificity of PSMA-PET-MRI in prostate cancer, one must consider whether the incremental diagnostic yield justifies the increased resource utilization, particularly in resource-constrained settings. The cost-benefit analysis must be contextualized within regional epidemiological and economic parameters. Furthermore, the generalizability of Western-centric clinical trials to low-income populations remains unvalidated. A global health equity framework is urgently required to prevent technological stratification in oncologic care.