Meningitis isn’t just a headache with a fever. It’s an inflammation of the protective layers around your brain and spinal cord-and it can kill within hours if ignored. Every year, about 1.2 million people worldwide get bacterial meningitis. Of those, nearly 135,000 die. But here’s the good news: most cases are preventable. Vaccines have cut cases of some types by 99%. The problem? Many people don’t know the signs until it’s too late.
What Exactly Is Meningitis?
Meningitis happens when the meninges-the thin membranes wrapping your brain and spinal cord-get inflamed. It’s not one disease. It’s a reaction to something else: bacteria, viruses, fungi, parasites, or even certain drugs and autoimmune conditions. The type determines how fast it hits, how bad it gets, and how you treat it.The Five Main Types of Meningitis
- Bacterial meningitis is the most dangerous. Caused by germs like Neisseria meningitidis (meningococcus), Streptococcus pneumoniae (pneumococcus), and Haemophilus influenzae type b (Hib), it can turn deadly in under 24 hours. Even with treatment, 5-30% of patients die. Survivors often face hearing loss, seizures, or brain damage.
- Viral meningitis is far more common-making up about 85% of all cases. Most are caused by enteroviruses, the same bugs behind stomach bugs and colds. It’s unpleasant: fever, headache, fatigue. But most people recover fully in 7-10 days without special treatment.
- Fungal meningitis is rare and mostly affects people with weakened immune systems-like those with HIV, cancer, or on long-term steroids. The main culprit is Cryptococcus neoformans. It’s slow-growing but deadly if missed. Around 223,000 cases happen yearly, with 181,000 deaths globally.
- Parasitic meningitis is extremely rare. The most common cause is Angiostrongylus cantonensis, a rat lungworm. People get it from eating raw or undercooked snails, slugs, or contaminated produce. It’s mostly seen in Southeast Asia and the Pacific Islands.
- Non-infectious meningitis isn’t caused by germs at all. It can come from lupus, certain cancer treatments, or reactions to medications like NSAIDs or antibiotics. It makes up 5-10% of cases.
What Are the Real Symptoms?
You’ve probably heard the classic trio: fever, stiff neck, headache. But here’s the truth-only 41% of people with bacterial meningitis have all three. In fact, 30% of immunocompromised patients show almost no symptoms at all.- High fever (above 101.3°F or 38.5°C) hits 86% of cases.
- Severe headache is reported by 87% of patients.
- Neck stiffness (nuchal rigidity) occurs in 70%.
- Light sensitivity (photophobia) affects 65%.
- Vomiting happens in over half.
- A rash that doesn’t fade when you press a glass against it-this is a sign of meningococcal sepsis. It starts as tiny red or purple spots and turns into large bruises.
- Confusion, drowsiness, or trouble waking up.
- Seizures.
- Extreme sensitivity to light or noise.
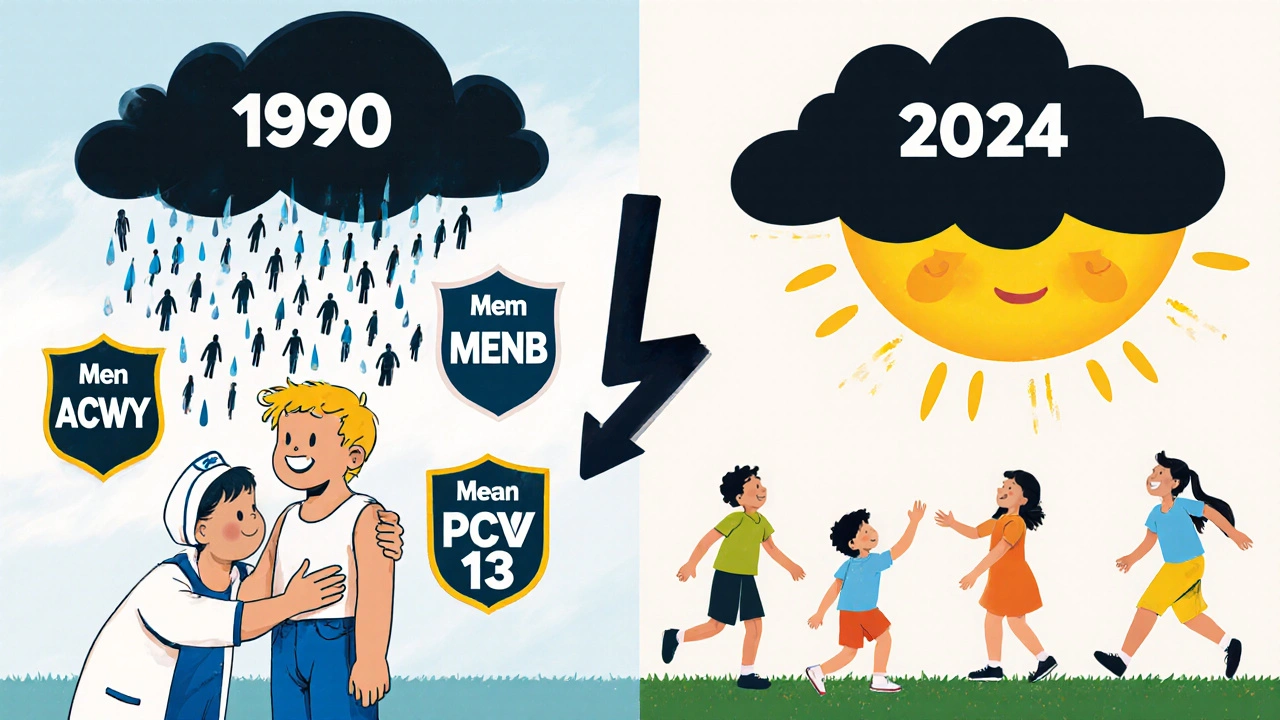
How Vaccines Stopped the Worst Cases
Vaccines are the biggest reason meningitis deaths are falling. Before vaccines, Hib alone caused 20,000 cases a year in the U.S. Now? Fewer than 50. That’s a 99% drop.- MenACWY (Menveo, MenQuadfi): Protects against four deadly strains (A, C, W, Y). Recommended for all kids at age 11-12, with a booster at 16. It’s 80-85% effective. In places where it’s required for college dorms, outbreaks have dropped by 75%.
- MenB (Bexsero, Trumenba): Targets serogroup B, which causes nearly half of teen and young adult cases. Previously only for high-risk groups, the CDC now recommends it for all adolescents starting in 2024. It’s 60-70% effective. College students living in dorms are 3-5 times more likely to get it.
- PCV13 (pneumococcal vaccine): Protects kids under 5 from pneumococcal meningitis. Reduces cases by 80% in vaccinated children.
- Hib vaccine: So effective that Hib meningitis is now rare in countries with routine immunization.
What If You’ve Been Exposed?
If someone in your house, dorm, or classroom gets bacterial meningitis, you’re at risk. But you don’t have to wait for symptoms. Close contacts (like roommates, kissing partners, or people sharing utensils) are given antibiotics like ciprofloxacin or rifampin within 24 hours. This drops the chance of getting sick from 1-5% to under 0.1%. Delay beyond 24 hours? Effectiveness plummets. The problem? Most people don’t know they were exposed until hours later. That’s why awareness matters. If someone you know is diagnosed, ask your doctor: “Should I get prophylaxis?”
Non-Vaccine Prevention
Vaccines are your best shield-but they’re not the only tool.- Wash your hands often. Hand hygiene cuts transmission risk by 30-50%.
- Don’t share drinks, utensils, toothbrushes, or lip balm. These are common ways bacteria spread.
- Pregnant women should avoid unpasteurized dairy and undercooked meats to prevent listeria meningitis.
- Travelers to the African meningitis belt should get MenACWY vaccine before departure.
Why People Delay-And Why That’s Deadly
A 2023 survey by the National Meningitis Association found that 68% of survivors waited over 38 hours before seeking care. Many thought it was just the flu. Others didn’t have a rash-and assumed they were fine. But here’s the hard truth: the rash doesn’t always come. In fact, half the time, it doesn’t show up at all. Waiting for it means waiting too long. A 2022 study in JAMA Internal Medicine showed that when ER doctors used standardized screening tools, diagnostic delays dropped from 8.2 hours to 3.7 hours-and deaths fell from 18% to 9%. If you’re feeling off, and it’s getting worse fast-especially with fever, headache, and neck pain-go to the ER. Don’t wait. Don’t text your doctor. Don’t “see how it is tomorrow.”What’s Next?
New vaccines are coming. A universal meningococcal vaccine targeting multiple strains is showing 92% effectiveness in early trials. A low-cost MenACWY vaccine priced at just $0.50 per dose is now being rolled out in Africa. But challenges remain. Antibiotic resistance in pneumococcus is rising-now 32% of strains in the U.S. resist penicillin. Vaccine costs are still high in poor countries. And serogroup replacement is real: as we block one strain, others can fill the gap. Still, the progress is undeniable. Meningitis used to be a death sentence. Now, it’s largely preventable. The tools exist. The science is clear. What’s missing is awareness.Can you get meningitis more than once?
Yes, but it’s rare. Different types of meningitis are caused by different germs. Getting bacterial meningitis from one strain doesn’t protect you from another. For example, surviving meningococcal disease doesn’t shield you from pneumococcal meningitis. Vaccines are the only reliable way to prevent multiple types.
Are meningitis vaccines safe?
Yes. Over 3.5 million pediatric records show 97% parental satisfaction with meningitis vaccines. Side effects are mild: sore arm, low-grade fever, or fatigue lasting less than 48 hours. Serious reactions are extremely rare-far less risky than the disease itself.
Do I need a meningitis vaccine if I’m over 20?
It depends. If you’re a college student living in a dorm, have a weakened immune system, travel to high-risk areas, or work in a lab with meningitis-causing bacteria, yes. For healthy adults over 20 who aren’t in these groups, routine vaccination isn’t currently recommended-but talk to your doctor if you’re unsure. The MenB vaccine is now advised for all teens, and some adults may benefit.
Can meningitis be cured?
Bacterial meningitis can be treated with antibiotics-but only if caught early. Delayed treatment increases death risk from 5% to over 20%. Viral meningitis usually clears on its own. Fungal and parasitic types need specific antifungal or antiparasitic drugs. Non-infectious cases are treated by stopping the trigger (like a drug) or managing the underlying condition.
What’s the difference between meningitis and encephalitis?
Meningitis affects the membranes around the brain and spinal cord. Encephalitis is inflammation of the brain tissue itself. They can happen together (meningoencephalitis). Symptoms overlap, but encephalitis often causes more confusion, seizures, or personality changes. Both are medical emergencies.










9 Comments
Bro, I got the MenB shot last year and my arm was sore for a day. Worth it. No way I'm letting some bacteria turn me into a statistic. 😎
Let me break this down for you slow folks. The CDC’s own data shows 85% of meningitis cases are viral and non-lethal. But you wanna panic about the 15%? That’s fearmongering. We’ve got better things to spend money on than vaccinating every teen. Plus, natural immunity > lab-made crap. 🤷♂️
ok but like… why do we even need 3 diff vaccines for meningitis? its just a head cold with extra steps right? i got the shot in 2018 and still got the flu last winter so… 🤔
My cousin had bacterial meningitis in college. She was fine one day, in the hospital the next. Lost hearing in one ear. She’s 28 now and still deals with it. Vaccines aren’t perfect but they’re the best shot we’ve got. Just get the damn shot. 🙏
Frankly, the entire public health narrative around meningitis is a textbook case of over-medicalization. You’ve got the CDC pushing vaccines like they’re candy, while ignoring the fact that most cases are self-limiting. And let’s not pretend the pharmaceutical industry isn’t cashing in-MenB vaccines cost $130 per dose. That’s not prevention, that’s profit-driven panic. 🤑
It’s fascinating how we treat meningitis like a monster when it’s really just biology doing its thing. The real tragedy isn’t the disease-it’s the lack of systemic awareness. Why do we wait for a rash to appear before acting? Why do we trust symptoms over science? We’ve got the tools. We just need the collective will to use them. No heroics needed. Just consistency.
Let’s get real: if you’re living in a dorm, partying, sharing drinks, and skipping vaccines, you’re playing Russian roulette with your neurology. The MenACWY + MenB combo isn’t optional-it’s a biological firewall. And yes, I said firewall. You’re not too cool for immunity. Get it. Now. 💪
I never thought much about this until my nephew got sick. Now I make sure everyone in my family is up to date. It’s not about fear. It’s about peace of mind. Simple as that.
Big shoutout to the docs and researchers who made this possible. Seriously. Vaccines saved my sister’s life. I know it’s easy to get cynical, but this is one of those rare wins where science actually worked. Don’t let noise drown out the facts. Get vaccinated. Protect your people. ❤️