Abrasion Healing Timeline Calculator
Track the healing process of your abrasion with this timeline tool. Enter the date you got the injury to see what to expect and what signs to watch for.
Healing Progress Timeline
Scraping your knee on a playground or getting a kitchen burn can feel dramatic, but most of the time the body knows exactly how to fix it. Understanding the abrasion healing journey helps you stay calm, avoid common mistakes, and spot trouble early.
What is an abrasion?
When you scrape a surface, the injury you’re dealing with is an Abrasion is a superficial wound that removes the outermost skin layer, usually caused by friction, a fall, or a sharp edge. Unlike deeper cuts, abrasions rarely hurt nerves or blood vessels, but they do expose the skin’s protective barrier, making infection a real concern.
How does the body heal an abrasion?
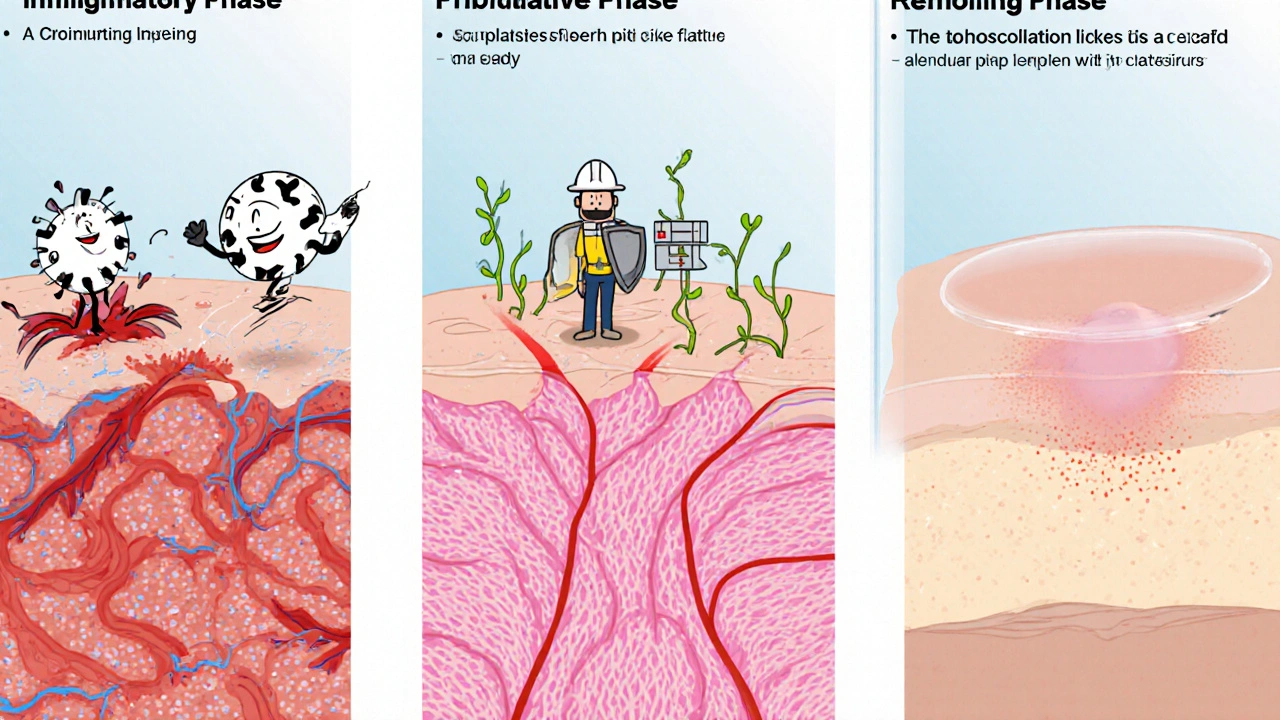
The process belongs to the broader phenomenon of Wound Healing is a coordinated sequence of cellular events that restores tissue integrity after injury. The body runs through three overlapping phases:
- Inflammatory Phase (0‑2 days) - Blood vessels constrict, then widen to let white blood cells rush in. These cells clean out debris and bacteria.
- Proliferative Phase (2‑7 days) - New tissue forms. Fibroblasts lay down Collagen is a protein that provides structural support for new tissue, and new blood vessels sprout to deliver nutrients.
- Remodeling Phase (7‑21 days and beyond) - Collagen fibers realign, the wound contracts, and the scar (if any) matures. Color and texture gradually blend with surrounding skin.
Each phase relies on healthy Skin is a the body’s largest organ that protects against external threats and regulates temperature. The outer Epidermis is a thin, protective layer that constantly regenerates and the underlying Dermis is a second layer rich in collagen, blood vessels, and nerves. When either layer is disrupted, the healing cascade kicks in.
Typical timeline: What to expect day by day
- Day 0‑1: The wound looks raw, may bleed slightly, and feels sore. A reddened halo signals the inflammatory response.
- Day 2‑3: Crusting (scab) forms as blood clot solidifies. The area might itch as new cells migrate underneath.
- Day 4‑7: New pink tissue (granulation) appears under the scab. The scab may loosen and fall off on its own.
- Day 8‑14: Most of the visible crust disappears. The wound looks pink and slightly raised - normal for the proliferative phase.
- Day 15‑21+: The scar (if any) fades, becoming flatter and lighter. Full strength returns slowly over weeks to months.
These ranges are averages; age, nutrition, and existing health conditions shift them. Younger, healthy skin typically heals faster.
Best practices for caring for an abrasion
Proper care accelerates healing and reduces infection risk. Follow these steps:
- Clean gently - Rinse the area with lukewarm water. Avoid harsh soaps; a mild, fragrance‑free cleanser works.
- Disinfect - Apply an Antiseptic is a substance that kills or inhibits microorganisms on the skin like povidone‑iodine or chlorhexidine. Let it dry before covering.
- Cover if needed - Use a non‑stick sterile dressing (e.g., a hydrocolloid pad) to protect the wound from friction. Change the dressing daily or whenever it becomes wet.
- Moisture balance - A thin layer of antibiotic ointment (e.g., bacitracin) can keep the wound moist, which speeds re‑epithelialization.
- Pain relief - Over‑the‑counter acetaminophen or ibuprofen eases discomfort and reduces inflammation.
- Nutrition - Protein, vitamin C, and zinc support collagen synthesis. A balanced diet with lean meat, citrus fruits, and nuts helps.
Hands off the scab unless it’s stuck. Popping it can reopen the wound and invite infection.
Signs of infection - when to act fast
Most abrasions heal without drama, but watch for red flags:
- Increasing redness that spreads beyond the wound margin.
- Swelling, warmth, or throbbing pain that intensifies after the first 48 hours.
- Yellowish pus or foul odor.
- Fever above 38°C (100.4°F) or chills.
- Red streaks radiating from the abrasion toward the heart.
Any of these symptoms merit a prompt medical visit. Early antibiotics can prevent deeper tissue involvement.

Special considerations
Not every abrasion follows the average script. Keep these groups in mind:
- Children - Kids often scratch or pick at scabs. Using a breathable, flexible dressing can reduce temptation.
- People with diabetes - High blood sugar impairs circulation and immune response. Monitor wounds closely, keep them clean, and seek professional care sooner.
- Tetanus risk - If the abrasion was caused by a dirty object and the person’s tetanus booster is older than 10 years, an immunization update is advisable.
- Large or deep abrasions - When more than 5 cm² or involving joints, a healthcare provider may need to debride (remove) dead tissue and apply advanced dressings.
Frequently Asked Questions
How long does an abrasion usually take to heal?
Most minor abrasions close within 7‑10 days, with visible scabbing disappearing by day 14. Full strength can take several weeks.
Can I use honey on an abrasion?
Medical‑grade honey has antibacterial properties and can be a safe dressing for small wounds, but commercial honey may contain spores. Use only sterile, medical‑grade honey if you choose this route.
Is it okay to wash an abrasion with alcohol?
Alcohol is too harsh; it damages new cells and delays healing. Stick to water, mild soap, and a gentle antiseptic.
When should I see a doctor for an abrasion?
Seek care if the wound is larger than a postage stamp, if you notice any infection signs, if you have diabetes or a weakened immune system, or if a tetanus shot is overdue.
Can I apply a bandage over a scab?
Yes, a breathable, non‑stick bandage protects the scab from friction while still allowing airflow. Change it daily.
Understanding each step of the abrasion healing journey empowers you to act confidently, keep infections at bay, and get back to your normal routine faster.








9 Comments
When you first notice a scrape, the most important step is to stop the bleeding gently; applying gentle pressure with a clean cloth does the trick. After the bleeding subsides, rinse the area with lukewarm water-avoid hot water because it can damage the fragile new tissue. A mild, fragrance‑free cleanser helps remove debris without stripping natural oils; many people overlook this and use harsh soaps, which can delay healing. Pat the skin dry with a clean gauze pad; rubbing can reopen micro‑tears. Apply a thin layer of antibiotic ointment-bacitracin or mupirocin are common choices-then cover with a non‑stick sterile dressing; this creates a moist environment that encourages re‑epithelialization. Change the dressing at least once daily, or sooner if it becomes wet or soiled; keeping the wound moist but not soggy is a delicate balance. Remember that the inflammatory phase typically lasts the first 48 hours, so some redness and swelling are normal, but any rapid expansion of redness warrants closer inspection. Nutrition plays a surprisingly pivotal role: protein supplies the building blocks for collagen, vitamin C acts as a co‑factor in collagen synthesis, and zinc contributes to cellular proliferation. Hydration also matters; well‑hydrated skin is more pliable and better able to repair itself. If you have diabetes, monitor blood glucose closely, because hyperglycemia impairs leukocyte function and delays collagen deposition. For children who tend to pick at scabs, a breathable, flexible bandage can reduce the temptation to disturb the wound. In the proliferative phase (days 2‑7), you may notice a pink granulation tissue forming beneath the scab-this is a sign of healthy tissue growth. Avoid the urge to “pop” the scab; it acts as a natural barrier against pathogens. By days 8‑14, the scab usually sloughs off on its own, revealing a pink but slightly raised wound; this is still part of normal remodeling. Full strength may take weeks to months, depending on age, health status, and wound size. Finally, keep an eye out for infection signs-spreading redness, increasing pain, pus, or fever above 38 °C-and seek medical care promptly if they appear. Following these steps consistently maximizes healing speed while minimizing complications.
Cleaning the abrasion with lukewarm water and a mild soap removes surface contaminants without irritating the newly forming tissue. Applying a sterile, non‑adhesive dressing protects the wound from friction while allowing airflow, which is essential for optimal healing. Monitoring for signs of infection-especially increased redness, swelling, or discharge-ensures timely medical intervention if needed.
Yo, just slap on some honey if u want 😉
While your advice is adequate, neglecting the importance of proper moisture balance can actually prolong the healing process; applying a thin layer of antibiotic ointment is not optional, it is essential, and failing to do so is irresponsible.
From a pathophysiological perspective, the cascade of cytokine-mediated cellular recruitment delineates the transition from the hemostatic to the proliferative phase, wherein fibroblasts synthesize extracellular matrix components such as type III collagen. The subsequent remodeling phase is characterized by matrix metalloproteinase activity, facilitating the conversion of collagen fibers into a more tensile type I configuration. Adequate nitrogenous substrate availability, primarily via dietary protein, underpins fibroblast proliferation, whereas micronutrients like ascorbic acid serve as essential cofactors for proline hydroxylation. Disruption of any of these biochemical pathways-whether by systemic disease states or inadequate nutritional intake-can manifest clinically as delayed epithelialization or hypertrophic scarring. Consequently, clinicians should adopt a multimodal therapeutic algorithm that integrates wound hygiene, optimal occlusive dressings, and targeted nutritional supplementation to expedite convalescence.
That’s a solid breakdown; in practice, though, a simple reminder to keep the wound clean and switch dressings daily often does the trick for most patients.
It is utterly galling how cavalier some people remain when discussing something as fundamental as skin integrity; an abrasion is not a trivial blemish but a breach of the body’s primary defense system. Ignoring proper after‑care is tantamount to inviting infection, a betrayal of one’s own health. One must champion meticulous hygiene, superior dressings, and vigilant monitoring with unwavering conviction. Anything less is an affront to basic medical prudence.
Absolutely, the stakes are high, and a proactive approach-cleaning, moist environment, and regular checks-can make all the difference 😊.
Great overview! Remember to stay hydrated and eat plenty of fruit for vitamin C – it really helps the skin heal faster 🍊.