When you pick up a prescription at your local pharmacy, you might not think twice if the pill looks different than last time. That’s generic substitution-a routine part of retail pharmacy. But if you’re in the hospital, and your IV antibiotic changes from one brand to another, that’s not just a swap. It’s a clinical decision, made by a team, documented in your chart, and tied to your treatment plan. The difference between how retail and hospital pharmacies handle medication substitution isn’t just about where you get your drugs-it’s about why and how those changes happen.
How Substitution Works in Retail Pharmacies
In retail pharmacies, substitution is mostly about cost. When a doctor writes a prescription for a brand-name drug like Lipitor, the pharmacist can legally swap it for a generic version-atorvastatin-unless the doctor checks "Do Not Substitute" or the patient says no. This isn’t optional; it’s built into state laws. All 50 states allow pharmacists to make this swap, and they do it 90.2% of the time when allowed by law and insurance rules.Why? Because insurance companies push for it. Most plans have formularies that require generics unless there’s a medical reason not to. Retail pharmacists spend a big chunk of their day navigating these rules-calling insurers for prior authorizations, explaining why a brand isn’t covered, or convincing a patient that the generic works just as well. In 2023, 92.4% of retail pharmacists said insurance requirements were the main driver behind substitution decisions.
Patients are supposed to be notified. In 32 states, pharmacists must tell you verbally. In 18, they need written consent for the first substitution. But in practice, many patients don’t remember the conversation. A 2023 Consumer Reports survey found that 14.3% of patients didn’t realize their medication had changed, leading to confusion about side effects or dosing.
Most retail substitutions are for oral pills-tablets and capsules. Only about 12.7% of specialty drugs (like injectables for autoimmune diseases) are even eligible for substitution, according to Express Scripts. That’s because these drugs are complex, often require special handling, and have limited generic alternatives.
How Substitution Works in Hospital Pharmacies
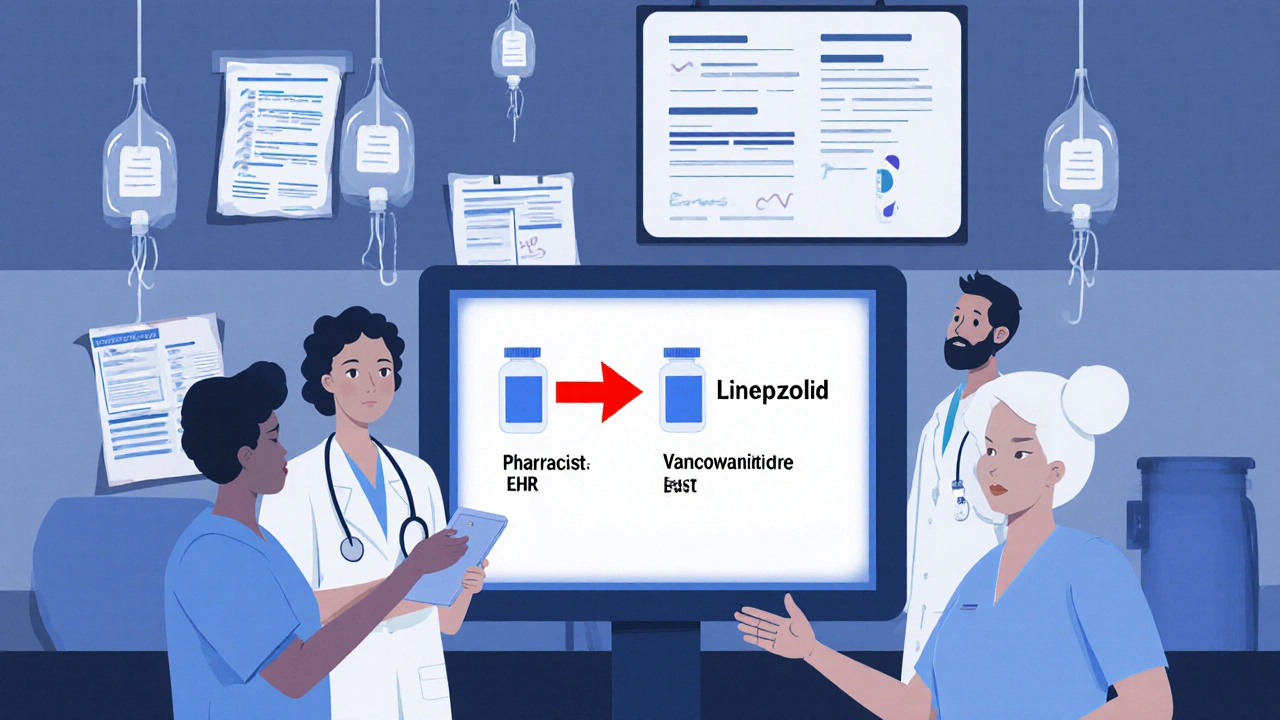
Hospitals don’t do substitution the same way. There’s no walk-up counter where a pharmacist hands you a different pill. Instead, changes happen behind the scenes, through a group called the Pharmacy and Therapeutics (P&T) committee. This team includes doctors, pharmacists, nurses, and sometimes administrators. They meet regularly to review which drugs should be on the hospital’s formulary-meaning which ones are approved for use.If a new, cheaper version of a drug proves just as safe and effective, the P&T committee might approve a therapeutic interchange. For example, switching from vancomycin to linezolid for MRSA infections. But this isn’t a pharmacist’s solo call. It’s a clinical decision backed by evidence, reviewed by multiple specialists, and documented in the electronic health record.
And it’s not just pills. In hospitals, substitutions often involve IV medications, biologics, and even compounded drugs. According to ASHP, 68.4% of hospital therapeutic interchanges involve IV drugs, compared to almost none in retail. Why? Because inpatient care is more complex. A patient on an IV antibiotic might need a switch due to kidney function, allergies, or resistance patterns-all things a pharmacist can’t assess alone.
When a substitution happens in the hospital, the prescriber must be notified within 24 hours. That’s a Joint Commission requirement. The change is logged in the EHR, and clinical decision support tools flag it so the care team knows what happened. No patient walks in asking for a different drug. The system changes the drug to fit the patient’s clinical needs.
Who Decides? Patient vs. Team
This is the biggest difference: who controls the decision.In retail, the patient has a voice. They can say no. They can ask for the brand. They can refuse the generic. The pharmacist’s role is to inform, respect their choice, and navigate insurance hurdles. It’s a transaction. One person, one decision.
In the hospital, it’s a team. The pharmacist doesn’t make the call alone. They recommend, but the doctor, nurse, and clinical team all weigh in. The patient’s preferences are considered, but they’re not the final say. The goal isn’t just cost-it’s safety, effectiveness, and alignment with clinical pathways.
Dr. Lucinda Maine of ASHP put it this way: “Hospital therapeutic interchange operates within a closed-loop system where substitutions are clinically vetted through P&T committees and integrated into care pathways, unlike retail substitution which often occurs as a transactional event driven by third-party payer requirements.”
That’s why hospital pharmacists need advanced clinical training. They’re not just dispensing-they’re managing drug therapy across complex conditions. Retail pharmacists need strong communication skills to explain substitutions to confused patients. Hospital pharmacists need deep knowledge of pharmacokinetics, antimicrobial stewardship, and drug interactions to make safe switches.
Cost Savings vs. Clinical Outcomes
Retail substitution saves money. A lot of it. In 2023, generic substitutions in community pharmacies saved $317 billion nationwide. That’s the main reason insurers push it. For a patient on a $300 brand-name drug, switching to a $10 generic is a huge win.Hospital substitution saves too-but differently. Vizient data shows hospital therapeutic interchange leads to an 18.7% average reduction in medication costs per acute care patient. But the bigger win is clinical. Hospitals use substitution to improve outcomes. For example, switching from broad-spectrum antibiotics to targeted ones reduces C. difficile infections. One hospital saw a 32% drop in C. difficile cases after implementing a beta-lactam substitution protocol.
That’s not just cost-it’s safety. And it’s why hospital pharmacists report higher satisfaction with substitution practices. In ASHP’s 2022 survey, 68.4% of hospital pharmacists said therapeutic interchange improved patient care. Only 52.7% of retail pharmacists felt the same, mostly because they’re stuck dealing with insurance delays and patient resistance.
Where Things Go Wrong
Both systems have risks.In retail, the biggest problem is communication. Patients don’t always understand why their medication changed. They might stop taking it because they think it’s “not the real thing.” Or they might not tell their new doctor about the switch, leading to dangerous interactions. Insurance prior authorizations can delay care-some pharmacists spend hours on the phone just to get a generic approved.
In hospitals, the risk is fragmentation. When a patient is discharged, their hospital medication list might not match what the retail pharmacy dispenses. A 2022 ISMP report found that 23.8% of medication errors during hospital-to-home transitions involved substitution mismatches. The hospital switched to a generic, but the retail pharmacy dispensed the brand because the discharge summary didn’t update properly.
That’s why new rules are coming. The 2023 CMS Interoperability Rule, effective July 2024, will require standardized electronic records of substitutions across settings. Epic and Cerner are already building tools to share substitution history between hospital and retail systems by 2025.

What Pharmacists Need to Know
If you’re new to pharmacy, the learning curves are very different.In retail, you’ll spend your first few months learning state laws, insurance formularies, and how to talk to patients. You’ll need to know when to say yes to a generic, when to push back, and how to handle angry customers who think generics are “inferior.” It’s about empathy, patience, and persistence.
In hospitals, you’ll spend your first six to twelve months learning how P&T committees work, how to interpret clinical guidelines, and how to use EHR decision support. You’ll need to know drug interactions inside out, understand antimicrobial resistance patterns, and be able to explain why a switch is safe to a skeptical doctor.
Both roles require deep knowledge-but applied in completely different ways.
The Future: Convergence, Not Conflict
The gap between retail and hospital substitution is slowly closing. More hospitals now have discharge programs that check a patient’s medication list before they leave. More retail chains are partnering with hospitals to follow up with patients after discharge.By 2028, Avalere Health predicts that 78% of healthcare systems will have integrated substitution protocols. That means when a patient is switched to a generic in the hospital, that change follows them home-automatically, accurately, and safely.
But retail substitution isn’t going away. It’s still the main engine of drug cost savings in the U.S. The Generic Pharmaceutical Association projects $1.7 trillion in savings from generics through 2028. That’s not just a number-it’s millions of people who can afford their meds because of it.
The real future isn’t about one system replacing the other. It’s about both working together. A pharmacist in a hospital makes a smart, clinical substitution. A pharmacist in a retail store ensures that substitution continues safely at home. That’s the goal: seamless, safe, and affordable care-no matter where the patient is.




9 Comments
Yeah right, like retail pharmacists are just money-grubbing clerks and hospital ones are some kind of medical wizards. I’ve seen hospital pharmacists refuse to switch a patient to a cheaper generic because ‘the committee hasn’t approved it yet’-while the patient’s on Medicaid and can’t afford the brand. The system’s broken, not the people.
Let’s be clear: the U.S. healthcare system is a corrupt, profit-driven nightmare. Insurance companies dictate drug choices in retail pharmacies-and hospitals? They’re just following the same script, masked in ‘clinical protocols.’ The real villain isn’t the pharmacist-it’s the FDA, the AMA, and Big Pharma’s lobbying arm. They’ve turned medicine into a commodity. And you wonder why people die from medication errors? It’s because we’ve outsourced care to accountants.
wait so u mean the gov is secretly using generic meds to track us?? like if u switch to atorvastatin they put a chip in it?? i heard this from a guy on youtube who works at cerner and he said the ehr logs everything even your sneezes lol
I get both sides. Retail pharmacists are under insane pressure from insurers and overworked patients. Hospital pharmacists are drowning in data and bureaucracy. The real issue isn’t who’s right-it’s that we don’t connect the two systems. A patient shouldn’t have to relearn their meds when they leave the hospital. Simple fix: shared digital records. Why isn’t that standard yet?
Let’s not pretend this is about patient care. It’s about power. The retail pharmacist, reduced to a glorified cashier, is forced to perform ideological obedience to corporate formularies. Meanwhile, the hospital pharmacist, cloaked in the sanctified robes of clinical authority, performs substitutions under the guise of ‘evidence-based practice’-but who decides what counts as evidence? The same pharmaceutical conglomerates that fund the studies, the same P&T committees that receive consulting fees, the same system that treats human beings as data points on a balance sheet. We have lost the soul of medicine. We have replaced compassion with compliance. And we call this progress?
The distinction between retail substitution and therapeutic interchange is methodologically valid, but the operational divergence reflects a broader fragmentation in pharmacoeconomic governance. Retail models are transactional, governed by payer-driven formulary constraints; hospital models are protocol-driven, embedded within clinical pathways. However, the lack of interoperability between EHR systems impedes continuity of care. The 2023 CMS Interoperability Rule is a necessary, albeit insufficient, step toward system harmonization.
Y’all act like hospital pharmacists are saints 🤡 They’re just doing the same thing but with a lab coat and a fancy title. And don’t get me started on these ‘P&T committees’-more like P&T cults where 7 doctors vote on which drug makes them look smart. Meanwhile, grandma in Ohio can’t afford her insulin because the ‘generic’ isn’t covered until Tuesday. Real talk: we need price caps, not more committees. 🤬💊
This was actually really helpful to read. I’m a new pharmacy tech and I’ve been confused about why hospital vs retail feels so different. Now it makes sense-retail is about access and affordability, hospital is about precision and safety. Both matter. We need both. And honestly? We need better communication between them. Maybe we can start by having discharge pharmacists call the retail pharmacy before the patient leaves? 🙌
It is imperative to note that the prevailing narrative regarding retail pharmacy substitution is fundamentally misinformed. The assertion that pharmacists merely act as agents of insurance companies is reductive and lacks empirical substantiation. In fact, pharmacists are statutorily mandated to ensure therapeutic equivalence and to counsel patients regarding potential bioequivalence variances. The 90.2% substitution rate is not indicative of coercion, but rather of regulatory compliance and cost-efficiency optimization. Furthermore, the notion that hospital pharmacists operate with superior clinical acumen is misleading; both domains require advanced pharmacotherapeutic knowledge, albeit applied in divergent contexts. The true deficiency lies not in the practitioners, but in the systemic fragmentation of pharmaceutical care delivery.