Transferring a prescription shouldn’t feel like playing Russian roulette with your health. One wrong digit on a label, one missed refill, one miscommunicated drug name-and you could be at risk of a dangerous overdose, missed treatment, or a hospital visit. In 2026, with electronic systems and updated federal rules, this doesn’t have to happen. But it still does-because too many people and pharmacies skip the basics.
Why Prescription Label Accuracy Matters More Than You Think
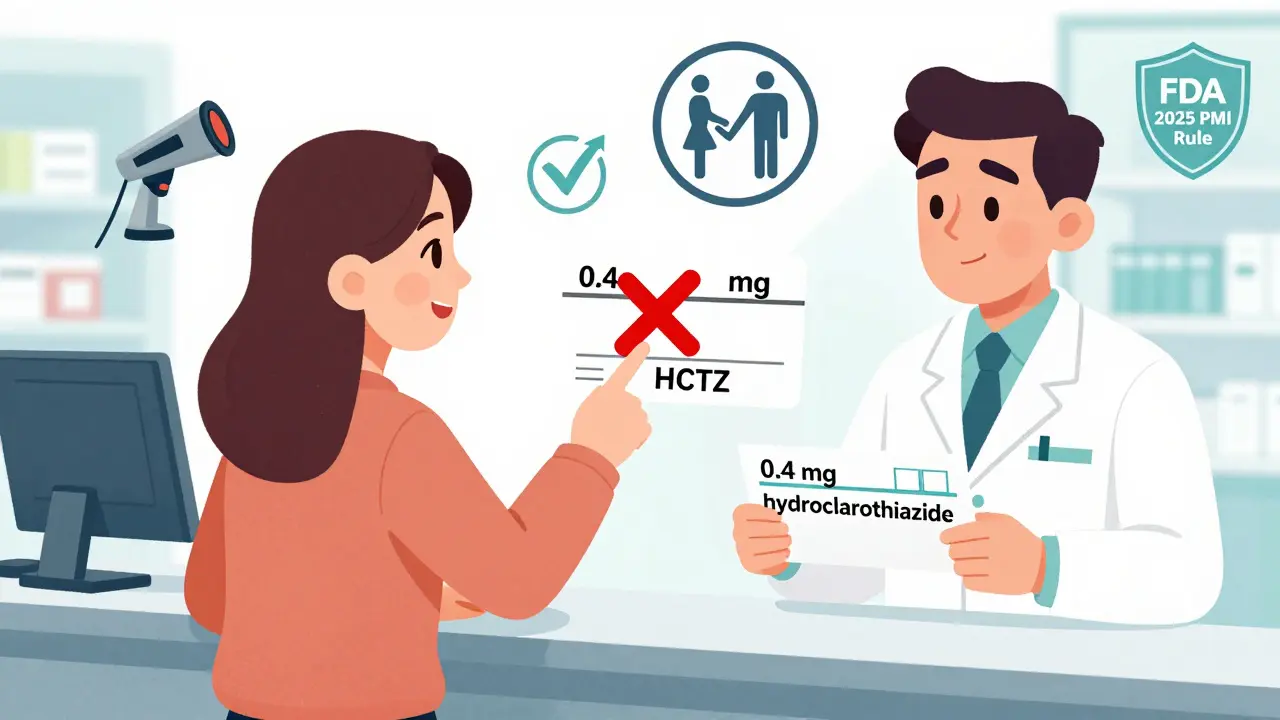
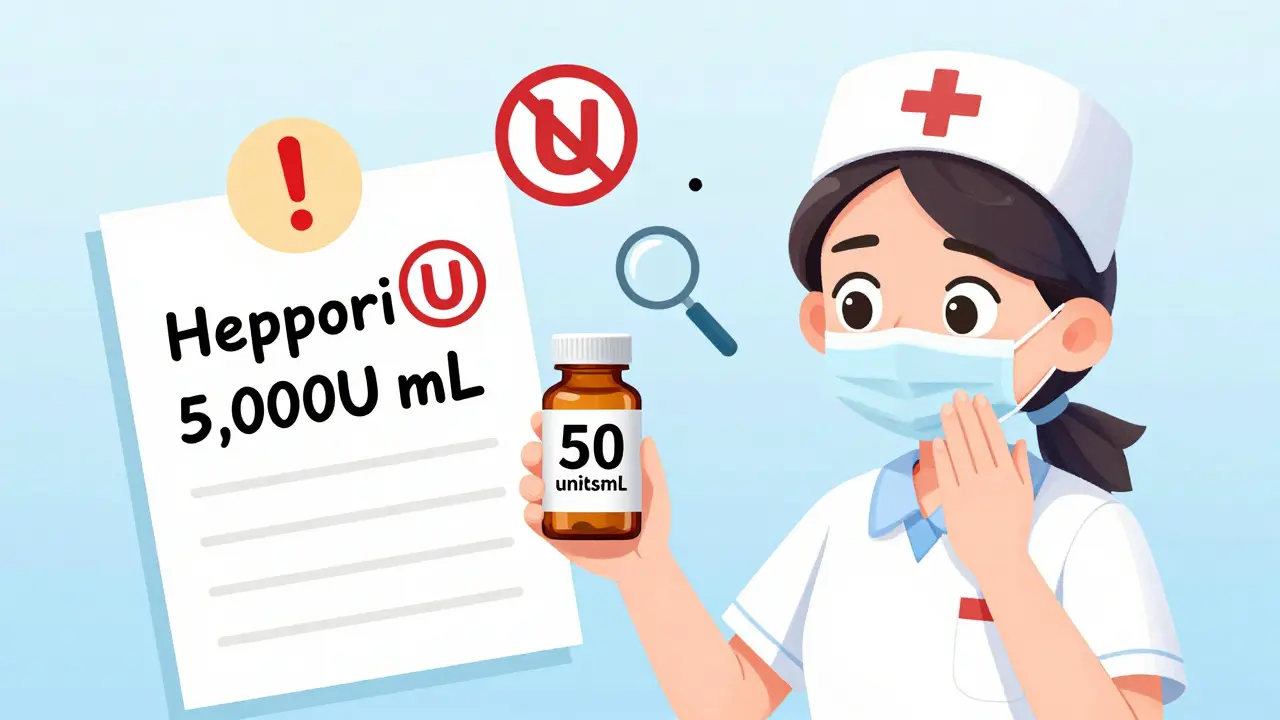
A tiny mistake on a prescription label can kill. The FDA estimates that 1.5 million adverse drug events happen every year in the U.S. because of unclear or incorrect labeling. That’s not a guess. That’s data from real hospital records, pharmacy audits, and patient reports. One of the most common-and deadly-errors? Trailing zeros. Writing "1.0 mg" instead of "1 mg" has led to over 327 documented cases of ten-fold overdoses between 2018 and 2022. Why? Because someone read "1.0" as "10". That’s not a typo. That’s a life-or-death misread. Same with leading zeros. Writing ".4 mg" instead of "0.4 mg" can make a pharmacist think you meant 4 mg. That’s ten times the dose. The National Coordinating Council for Medication Error Reporting and Prevention (NCCMERP) found this mistake in nearly 1 in 5 error reports they analyzed in 2022. And it’s not just about numbers. Abbreviations like "HCTZ" for hydrochlorothiazide or "MOM" for magnesium oxide mixture are banned in modern prescribing because they’re too easy to confuse. "MOM" could be mistaken for morphine. "HCTZ" might look like "HCT"-a different drug entirely. Your label must include:- Patient’s full name
- Drug name (no abbreviations)
- Strength in metric units (e.g., 5 mg, not 5.0 mg)
- Dosage form (tablet, capsule, liquid)
- Quantity dispensed
- Directions for use (e.g., "Take one tablet by mouth twice daily")
- Prescriber’s name and DEA number
- Prescription number
- Date issued
- Number of refills allowed
- Pharmacy name, address, and phone number
The DEA’s 2023 Rule: What Changed for Controlled Substances
Before August 2023, if you had a Schedule II prescription-like oxycodone, fentanyl, or Adderall-you couldn’t transfer it at all. Not even once. If you moved, changed pharmacies, or needed a refill at a different location, you had to go back to your doctor for a new paper script. That changed. The DEA’s new rule (21 CFR § 1306.25) now allows one electronic transfer of Schedule II prescriptions between retail pharmacies. It’s a big deal. But it comes with strict rules. Here’s what’s required:- Transfer must be electronic-no fax, no phone call, no paper copy.
- All data must be preserved exactly as it was on the original. No trimming, no changing, no guessing.
- The transferring pharmacist must record: the date of transfer, their name, the receiving pharmacy’s name, address, and DEA number.
- The receiving pharmacist must mark the record as "transfer," and add the name of the pharmacy that sent it.
- Only one transfer is allowed. After that, you need a new prescription.
How to Transfer a Prescription Without Mistakes
You’re not just a patient. You’re part of the safety chain. Here’s how to make sure your transfer goes smoothly:- Call the new pharmacy first. Don’t assume they can take your script. Ask: "Can you accept an electronic transfer of a Schedule II prescription?" Some rural pharmacies still use old systems that can’t handle it.
- Give them your full name, date of birth, and prescription number. Even if you think they have your file, confirm it. A mismatched name or wrong date of birth can cause a transfer to fail.
- Don’t request the transfer until you’re sure they have the drug in stock. Schedule II prescriptions can only be filled once. If they transfer it and then run out? You’re stuck until your doctor reissues it.
- Ask for a confirmation. After the transfer, call back in 1-2 hours. Say: "Did my prescription transfer successfully? Can you confirm the drug, dose, and refill count?"
- Check the label when you pick it up. Compare it to your old label. Is the drug name spelled the same? Is the dose the same? Is the refill count correct? If anything looks off, don’t take it. Ask the pharmacist to double-check.
Electronic Systems Are the Only Safe Way-But They’re Not Perfect
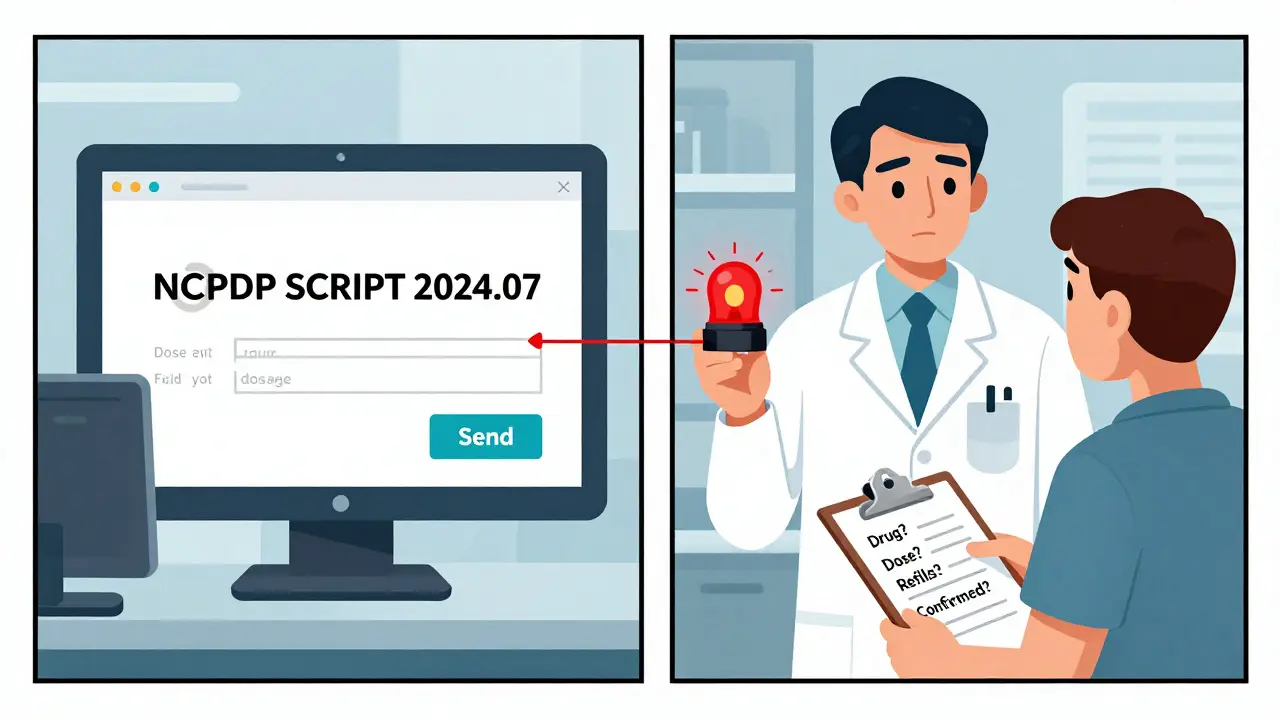
The DEA requires electronic transfers using the NCPDP SCRIPT standard (version 2017071 or newer). These systems are 98.7% accurate, according to a 2022 University of Florida study. Fax transfers? Only 82.3% accurate. Phone calls? Just 76.1%. But here’s the catch: not all systems talk to each other. A 2022 survey by the National Community Pharmacists Association found that 18% of pharmacies reported data truncation during transfers-meaning part of the label got cut off. Sometimes the directions or refill count disappeared. Independent pharmacies are more likely to have this problem. Chain pharmacies (like CVS or Walgreens) use the same software, so they’re better connected. But if you’re going to a small, local pharmacy, ask: "Do you use NCPDP SCRIPT 2024.07?" If they don’t know what you’re talking about, they might not be ready for the new rules.What Pharmacists Must Do to Stay Compliant
Pharmacists aren’t just filling scripts. They’re the last line of defense. The American Society of Health-System Pharmacists (ASHP) says every transfer should be double-checked. That means:- One pharmacist receives the transfer.
- A second pharmacist verifies: drug name, strength, dosage, refills, patient info.
- Barcode scanning is used to match the physical bottle to the digital record.
- Plain language instructions (no medical jargon)
- Warning icons for high-risk drugs
- Automated scanning to catch label errors before the bottle leaves the counter
State Rules Still Vary-Even With Federal Standards
The DEA rule set a national floor, but states can add more. Wisconsin requires the receiving pharmacy’s name and DEA number to be printed on the back of the original, invalidated prescription. Massachusetts requires additional documentation for controlled substance transfers. If you live in one state and transfer to another, you’re playing by two sets of rules. Dr. Jerry Phillips, former FDA medication errors director, called this a "patchwork of requirements" that increases the risk of mistakes. Bottom line: Don’t assume what’s legal in your state is legal everywhere. Always confirm the rules with the receiving pharmacy.What Happens If You Skip the Steps?
Skipping verification leads to:- Wrong drug or dose
- Missing refills
- Prescription rejection
- Delayed treatment
- Emergency room visits
- Legal liability for the pharmacy
What You Can Do Today
You don’t need to be a pharmacist to keep yourself safe. Here’s your quick checklist:- Always initiate the transfer yourself. Don’t let a doctor’s office or family member do it for you.
- Confirm the new pharmacy can handle electronic transfers-especially for controlled substances.
- Verify the drug name, dose, and refill count on the new label before leaving the pharmacy.
- Never accept a prescription with trailing zeros (1.0 mg) or missing leading zeros (.4 mg).
- If something looks wrong, say something. Ask to speak to the pharmacist.
Can I transfer a Schedule II prescription like oxycodone to a different pharmacy?
Yes, but only once, and only electronically. The DEA’s 2023 rule allows one electronic transfer of Schedule II prescriptions between retail pharmacies. You cannot transfer by fax, phone, or paper. After the transfer, you’ll need a new prescription from your doctor for any further refills.
Why can’t I use "1.0 mg" on my prescription label?
Writing "1.0 mg" instead of "1 mg" can cause a ten-fold overdose. Someone might read the ".0" as a decimal point and mistake it for "10 mg." The FDA and NCCMERP have documented over 300 errors since 2018 because of trailing zeros. Always write whole numbers without decimals-"1 mg," not "1.0 mg."
What happens if the pharmacy transfers my prescription incorrectly?
If the pharmacy transfers the wrong drug, dose, or refill count, it’s a violation of federal law. The DEA can issue fines or suspend the pharmacy’s license. For patients, it means taking the wrong medication-which can lead to serious harm or death. Always verify the label when you pick up your prescription.
Do I need to go to my doctor to transfer a prescription?
No, you don’t need to go back to your doctor to transfer most prescriptions. You can request a transfer directly to a new pharmacy. But for Schedule II controlled substances, you can only transfer once. After that, you’ll need a new prescription. Always confirm with the new pharmacy that they can accept the transfer before you request it.
Are electronic transfers safer than fax or phone transfers?
Yes. Electronic transfers using NCPDP SCRIPT standards are 98.7% accurate, according to a 2022 University of Florida study. Fax transfers are only 82.3% accurate, and phone transfers are just 76.1% accurate. That means one in five phone transfers has a mistake. Electronic is the only safe way for Schedule II drugs.
What should I do if my prescription label looks wrong?
Don’t take it. Ask to speak to the pharmacist immediately. Compare the label to your old one or the original prescription. Check the drug name, dose, quantity, and refill count. If anything doesn’t match, the pharmacy must recheck it before dispensing. Your safety comes first-never assume it’s correct.







15 Comments
This post saved my life last year. I almost took a 10mg dose of oxycodone because the label said "1.0 mg" and I didn’t catch it. I asked the pharmacist to double-check-and they apologized. Now I always read every word. Don’t assume it’s right.
People think pharmacies are infallible. They’re not. We’re the last line of defense.
Always check. Always ask. Always speak up.
Thank you for this. As someone who works in healthcare compliance, I can’t stress enough: trailing zeros are a silent killer. I’ve seen charts where "0.5 mg" was handwritten as ".5 mg"-and yes, someone gave a patient 5 mg. That’s not negligence. That’s a systemic failure.
Pharmacies need mandatory double-checks, not just for controlled substances, but for EVERY prescription. And yes, I’m talking about you, small-town pharmacies with one pharmacist on duty at 2 a.m.
Also: NCPDP SCRIPT 2024.07 is the bare minimum. Anything older is a liability. If your pharmacy doesn’t know what that is, find a new one.
So let me get this straight: we’re now trusting computers more than humans, but the computers still mess up because some pharmacy’s software is from 2012?
Classic America. We automate everything, then act shocked when it breaks.
Also, I’m pretty sure the DEA just gave pharmacists a new way to say "no" to patients who need meds. "Sorry, you can only transfer once. Good luck driving 90 miles." :roll_eyes:
I moved from Texas to Oregon last year and had to transfer three prescriptions-including a Schedule II. The first pharmacy I tried said they couldn’t accept it because "their system doesn’t talk to the other state’s network."
I called five places before I found one that could. Took two days. I was in pain. I cried. I felt like a criminal for needing pain meds.
This isn’t just about labels. It’s about dignity. We need better systems. Not more rules. Better tech that works across state lines.
And yes, I checked the label. Twice.
you know what? i think this whole system is rigged. why do we even need to transfer prescriptions? why cant the doctors just send it to the pharmacy we want? why are we punished for moving? why do we have to beg for our own medicine?
and dont even get me started on the "one transfer only" rule. its like they want us to suffer. its capitalism. its the pharmas. its the government. its all connected.
they dont care if you die. they just want you to keep buying pills.
peace out, bros.
My grandma used to say, "If it looks weird, it probably is."
I always check my labels now. Same drug, same dose, same refill count. If it’s different, I ask. No shame. No rush.
And I never let anyone else request the transfer for me. That’s my job. My life. My responsibility.
Simple. But it works.
Okay but can we talk about how ridiculous it is that a pharmacy can lose its license over a faxed transfer, but no one gets fined for writing "MOM" on a script?
Why are we punishing the pharmacy for the doctor’s laziness?
Also, I love that the FDA is pushing plain language on labels. "Take one tablet by mouth twice daily" is so much clearer than "Q12H PO".
Can we make this mandatory for ALL meds? Even OTC? I want to know what I’m taking without a medical dictionary.
Also: yes, I checked my label. Twice. And I high-fived the pharmacist. She smiled. We’re both alive today. :)
Let me tell you something: the real problem isn’t the transfer rule. It’s that we treat medication like a vending machine.
You don’t just "get" a Schedule II script like you get a latte. It’s a controlled substance for a reason. The system is designed to protect you, even when it feels like it’s working against you.
Yes, it’s inconvenient. Yes, it’s frustrating. But if you want to live past 40, you follow the rules. And if you’re too lazy to call the pharmacy, then you deserve the 4-day gap in your pain relief.
Don’t blame the system. Be the person who double-checks. That’s the real power move.
Let’s be brutally honest: 90% of these "adverse drug events" are caused by patients who don’t read their own labels. You think a trailing zero is the problem? No. The problem is that people don’t know what "mg" means. They don’t know the difference between a tablet and a capsule. They assume the pharmacist is a mind-reader.
And now we’re spending $18,750 per pharmacy to slap a "warning icon" on a bottle? That’s not safety. That’s performative healthcare.
Real solution? Educate the public. Teach basic pharmacology in high school. Make patients responsible for their own understanding. Stop outsourcing your brain to a pharmacy.
Also, the DEA rule? It’s a Band-Aid. The real issue is that prescribers are still using abbreviations. And the FDA’s "PMI" rule? It’s just more paperwork for people who already know what they’re taking.
Stop pretending technology fixes human stupidity.
Why are we letting foreign pharmacies handle our prescriptions? I bet half these "electronic transfers" are routed through India or the Philippines. You think they care about your 1.0 mg? They’re just typing it in while eating samosas.
And don’t even get me started on NCPDP. That’s a Canadian standard, right? We’re letting the Canadians dictate how we give out opioids?
This is why America is falling apart. We outsource everything. Even our medicine.
Build American systems. Hire American pharmacists. Stop letting the world decide how we die.
Wait. So the DEA says you can transfer a Schedule II script once… but only if it’s electronic… but only if the pharmacy uses the right software… but only if you call twice… but only if you check the label… but only if you don’t live in a rural town where the pharmacy uses a fax machine from 1997?
So the rule exists… but only for people who already have the resources to follow it?
That’s not a safety rule. That’s a privilege filter.
And you call this progress? LOL.
Meanwhile, my cousin in Alabama still gets his oxycodone from a guy who drives it from Florida. At least he doesn’t have to call five pharmacies.
System is broken. Not the patients. The system.
Wow. This is like a TED Talk disguised as a Reddit post. So many emojis I almost cried. 🧠💊📊
But seriously, I love that we’re finally acknowledging that "1.0 mg" is a death sentence. I work in med-tech and we just rolled out AI label scanning at our clinic. It flags trailing zeros, missing leading zeros, and even abbreviations like "HCTZ" in real time.
It’s expensive. But it’s worth it. I’d rather pay $20k than bury someone because someone didn’t add a zero.
Also, yes, I’m using emojis. Deal with it. 🤷♂️
I used to be the person who just grabbed the bottle and walked out. Then my sister had a reaction to a mislabeled insulin. She didn’t die, but she spent three days in the hospital.
Now I read every label like it’s a love letter from my future self.
Drug name? Check.
Dose? Check.
Refills? Check.
Pharmacy phone? I call it. Just to hear a human voice say, "Yes, we got it right."
It’s not paranoia. It’s peace of mind.
And if you’re too busy to check? You’re not busy. You’re careless.
Love you, fellow humans. Stay safe.
THEY’RE LYING TO US. I KNOW IT. WHY DO THEY MAKE US CALL TWICE? WHY CAN’T THE SYSTEM JUST WORK? I SAW A VIDEO ON TIKTOK WHERE A PHARMACIST WAS SMILING WHILE GIVING A PATIENT THE WRONG DRUG. THEY’RE ALL IN ON IT. THE DEA. THE PHARMACIES. THE GOVERNMENT. THEY WANT US TO BE AFRAID. THEY WANT US TO BE DEPENDENT. THEY WANT US TO PAY MORE. THIS ISN’T SAFETY. THIS IS CONTROL. 🚨💣
Just to clarify something I said earlier: the "one transfer" rule for Schedule II drugs? It’s not about control. It’s about preventing doctor shopping. And yes, it’s flawed-but it’s not the enemy.
The real enemy is the pharmacy that skips the double-check. The one that doesn’t scan the barcode. The one that says, "Oh, it’s probably fine."
That’s where the danger lives.
So next time you get your prescription, thank the pharmacist. And then double-check it yourself. Because if they slip up? You’re the only one who can catch it.