Millions of people believe they’re allergic to penicillin-or amoxicillin, or another common antibiotic-because they had a rash as a kid, or their mom said so, or a doctor wrote it down once and never checked again. But here’s the truth: over 95% of those labels are wrong. And that mistake is making your future infections harder, more expensive, and riskier to treat.
Why a False Allergy Label Matters More Than You Think
If you’re labeled allergic to penicillin, doctors can’t give you the safest, most effective antibiotic for common infections like strep throat, urinary tract infections, or pneumonia. Instead, they turn to broader-spectrum drugs like vancomycin, clindamycin, or fluoroquinolones. These aren’t just less targeted-they’re more likely to cause side effects, trigger C. diff infections, and fuel antibiotic resistance. In the U.S., 10-15% of hospitalized patients carry a penicillin allergy label. But when tested, only 1-2% actually have a true IgE-mediated allergy. That means roughly 9 out of 10 people are avoiding a safe, effective drug for no reason. The result? Hospitals use 30% more broad-spectrum antibiotics than they need to. That’s not just bad medicine-it’s a public health crisis. A 2022 study in JAMA Internal Medicine found that each false penicillin allergy label adds about $1,000 in extra costs per patient. Why? Longer hospital stays, more lab tests, and pricier drugs. And it’s not just money. The CDC estimates false labels contribute to 50,000 extra cases of C. diff each year in the U.S. alone. That’s a dangerous, hard-to-treat gut infection that can be fatal.How Do You Know If Your Allergy Label Is Real?
Most people don’t remember why they got the label. Was it a rash? A stomach ache? A family member had a reaction? None of those are reliable signs of a true allergy. True drug allergies involve the immune system and usually show up within minutes to an hour after taking the drug. Symptoms include hives, swelling, trouble breathing, or anaphylaxis. A mild rash that appeared days later? That’s often not an allergy at all-it could be a viral rash, a side effect, or something else entirely. The only way to know for sure is to get tested. And it’s not complicated.The Three-Step Testing Process
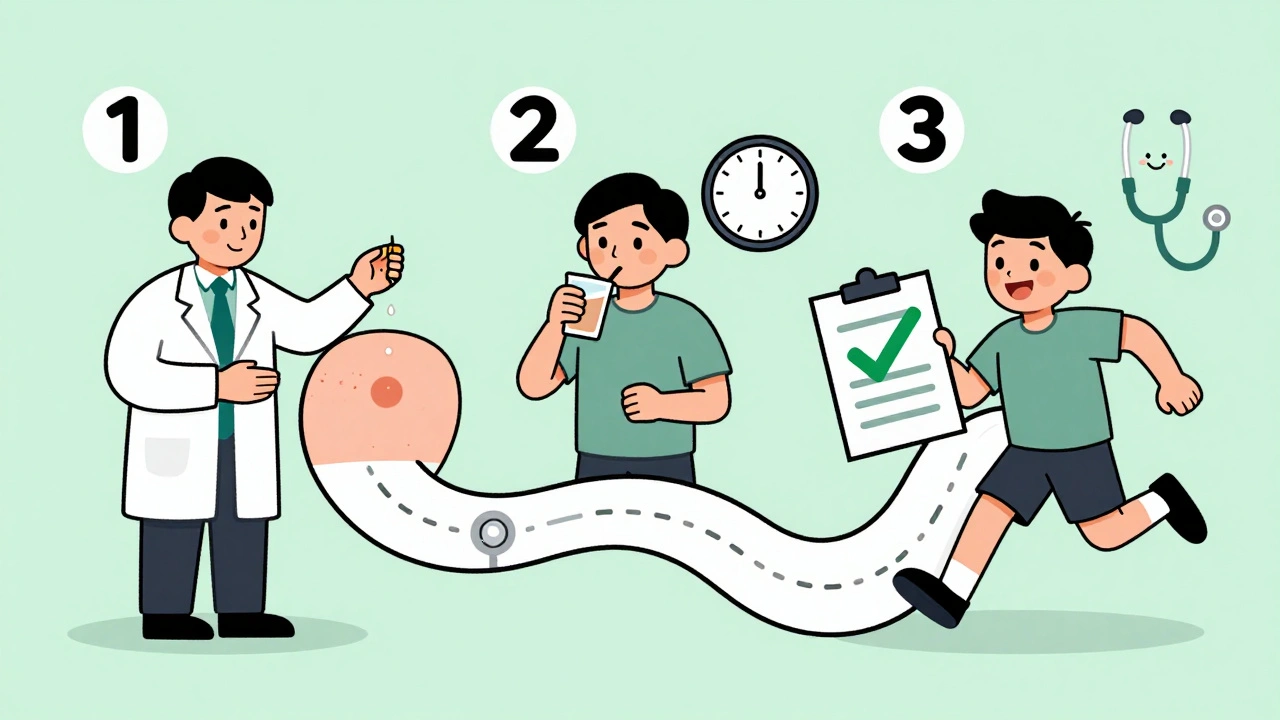
There are three main ways to confirm or remove a false allergy label, and the right one depends on your risk level.- Low-risk patients (no history of anaphylaxis, no severe reactions): Can often skip skin testing entirely. Doctors give you a full therapeutic dose of the antibiotic (like amoxicillin) under observation for 30-60 minutes. If you don’t react, the label is removed. This is safe, fast, and works in 94.5% of cases.
- Moderate-risk patients (history of rash or mild reaction): Usually get skin testing first. A tiny amount of the drug is placed under the skin (skin prick test), then a small injection (intradermal test). If both are negative, you get a graded oral challenge-starting with a small dose, then increasing over time. This approach has a 98% negative predictive value.
- High-risk patients (past anaphylaxis, swelling, breathing issues): Need evaluation by an allergist. Testing is done in a controlled setting with emergency equipment on hand.
What Happens After Testing?
If the test is negative, your allergy label is removed. That’s it. No more warnings on your chart. No more avoiding penicillin-based drugs. You can now take amoxicillin for a sinus infection, or penicillin for a heart valve infection, without worry. But here’s the catch: the label doesn’t disappear on its own. You need to make sure your medical records are updated. Many EHR systems still show “penicillin allergy” even after testing. Ask your doctor to change it to “Penicillin allergy ruled out” or “No true allergy confirmed.” Some hospitals now use automated tools in their electronic records to flag these cases and prompt updates. One patient from Massachusetts General Hospital had a 40-year-old penicillin label. She avoided antibiotics for years, got recurrent UTIs, and was hospitalized twice. After testing and de-labeling, she took amoxicillin for her next infection-and never went back to the hospital. Her care costs dropped by $28,500 over two years.Why Isn’t Everyone Getting Tested?
The science is clear. The guidelines exist. The tools are ready. So why aren’t more people getting tested? Barriers are mostly systemic:- Lack of access: In rural areas, allergists are scarce-sometimes fewer than one per 500,000 people.
- Workflow gaps: Most doctors don’t know how to start the process. They assume it’s too complicated or requires a specialist.
- Patient fear: People are scared to take the drug again, even if they’ve never had a real reaction.
- Electronic health record problems: Many systems don’t let you easily update allergy status. One survey found 37% of hospitals don’t even have the right test formulations on hand.
What If You Have a Reaction During Testing?
It’s rare. Less than 2% of people have any reaction during testing. And most are mild-like a small rash or stomach upset. Severe reactions are extremely uncommon. If you do react, the medical team is ready. They have epinephrine, oxygen, and emergency protocols in place. The test is designed to be safe. You’re not being thrown into the deep end-you’re being guided through it step by step. One Reddit user wrote: “I was terrified. But after the skin test was negative, they gave me 25mg, then 100mg, then the full dose. No reaction. Now I can take amoxicillin instead of Z-Pak, which always gave me stomach cramps.”
Who Should Get Tested?
If any of these sound like you, you’re a candidate:- You were told you’re allergic to penicillin as a child, but never had a serious reaction.
- You’ve never taken the drug since the label was added.
- You’ve taken penicillin or amoxicillin since and had no reaction.
- You’ve had a rash after antibiotics, but no swelling, breathing issues, or anaphylaxis.
- You’ve been prescribed clindamycin, vancomycin, or another broad-spectrum drug because of your allergy label.
What About Other Antibiotics?
Penicillin is the most common false label, but it’s not the only one. Other beta-lactams like cephalosporins and carbapenems can also be mislabeled. Cross-reactivity is often overestimated. Just because you’re labeled allergic to penicillin doesn’t mean you’re allergic to all similar drugs. Testing should be specific. If you’re cleared for amoxicillin, that doesn’t automatically clear you for cefdinir. But many patients can safely take other beta-lactams after penicillin testing. Your doctor can help determine which ones are safe based on your history and test results.What’s Next?
By 2028, experts predict 70% of penicillin allergy assessments will happen through automated tools in hospital systems-no specialist visit needed. You’ll get a prompt in your patient portal: “Your record shows a penicillin allergy. Would you like to get tested?” That’s the future. And it’s already starting. You don’t need to live with an outdated label. You don’t need to risk worse infections or pay more for care. If you’ve been told you’re allergic to penicillin-or any antibiotic-ask your doctor: “Could this label be wrong? Can I get tested?” It’s not just about saving money. It’s about getting the right treatment when you need it most.Can I outgrow a penicillin allergy?
Yes. Most people who had a penicillin allergy as a child lose it over time. Studies show that 80% of people who were allergic in childhood are no longer allergic after 10 years. Even if you had a true reaction decades ago, you might still be able to take penicillin safely today. Testing is the only way to know for sure.
Is penicillin allergy testing safe?
Extremely. Over 94% of people who undergo testing tolerate penicillin without issue. Reactions are rare and usually mild-like a small rash or stomach upset. Severe reactions are extremely uncommon. Testing is done in controlled settings with emergency equipment ready. The risk of not testing-using stronger, riskier antibiotics-is far greater.
Do I need to see an allergist to get tested?
Not necessarily. Many primary care doctors, nurse practitioners, and pharmacists are now trained to perform low-risk de-labeling using direct oral challenges. You don’t need to travel to a specialty clinic. Ask your regular doctor if they offer penicillin allergy testing. If they don’t, they can refer you to a program nearby.
What if my doctor says I’m allergic and won’t test me?
You have the right to ask for testing. The guidelines from the American Academy of Allergy, Asthma & Immunology and the CDC clearly support de-labeling for low- and moderate-risk patients. If your doctor refuses, ask for a referral to an infectious disease specialist or an allergy clinic. You can also search for hospitals with “penicillin allergy relief programs”-many now have dedicated teams for this.
Will insurance cover the test?
Yes, in most cases. Medicare and private insurers cover allergy testing when it’s medically necessary. Since false allergy labels increase healthcare costs, removing them saves money overall. Many hospitals now include testing as part of routine care for patients with allergy labels. Ask your provider to code it as “drug allergy evaluation” or “antibiotic stewardship assessment.”
Can I get tested if I’ve never taken penicillin before?
Absolutely. Many people have allergy labels based on family history, a childhood rash, or a misdiagnosis. If you’ve never taken penicillin and were never tested, you’re a perfect candidate for direct oral challenge. There’s no need to wait for a reaction. Testing can safely confirm you’re not allergic-and open up better treatment options for life.











14 Comments
My grandma had a penicillin label for 50 years because she got a rash as a kid. She finally got tested last year and now she takes amoxicillin like it’s candy. No more hospital trips for UTIs. It’s wild how something so simple can change your whole life.
THEY’RE LYING TO US. This is all part of the Big Pharma agenda. They want you stuck on $800 antibiotics so you keep coming back. Penicillin costs 2 bucks. They make billions off vancomycin. Don’t fall for the ‘testing’ scam-it’s just a trap to make you pay more for ‘specialist visits.’
So let me get this straight. We’re supposed to trust a 10-minute test over 40 years of medical history? What’s next, ‘hey you’re not allergic to peanuts, just eat a whole jar’? This is dangerous nonsense.
OMG I just realized I’ve been avoiding penicillin since I was 6 😭 I got a rash after some ear drops and my mom freaked out. I just took amoxicillin for a sinus infection last month and nothing happened… maybe I should get tested? 🤔
Wow. So the solution to antibiotic overuse is… giving people more antibiotics? Genius. Next they’ll tell us to stop washing hands to prevent ‘germophobia.’
In India, we don’t even have penicillin allergy labels. People just take what’s prescribed. If you get a rash, you stop. No testing, no records. It works. Maybe we don’t need all this bureaucracy.
I work in a clinic. We started doing oral challenges last year. 87 patients. Zero severe reactions. One guy cried because he finally got to eat his mom’s chicken soup without worrying about ‘penicillin contamination’ in the broth. This isn’t medicine-it’s liberation.
THIS IS THE MOST IMPORTANT THING YOU’LL READ THIS YEAR. I was labeled allergic at 8. Took clindamycin for every infection. Got C. diff twice. Got tested at 32. Now I take amoxicillin like a boss. My insurance saved $12k. My body saved its microbiome. Do the test. Please.
i just had a rash after penicillin as a kid but i never had trouble breathing… so i guess its not a real allergy? my doctor said ‘eh its better to be safe’ but now im scared to take anything. help?
That’s exactly what I thought. But the test isn’t scary-it’s just a few hours of watching. They give you tiny doses and monitor you. If you’re nervous, start with the skin test. No needles, just a little scratch. I did it with my mom holding my hand.
They’re testing penicillin but not asking why the system labels people so carelessly. Who wrote that ‘allergy’ in 1978? A tired intern? A nurse who didn’t know the difference between a viral rash and anaphylaxis? This isn’t medical progress-it’s institutional negligence.
My cousin is a nurse in rural Kansas. She does penicillin challenges in her clinic now. No allergist needed. She just follows the checklist. People are so scared of ‘trying again’-but it’s the safest thing they’ll do all year. 🌻
I had my label removed after a 2-hour observation. No drama. No panic. Just a nurse handing me a cup of water and saying ‘here’s your antibiotic, you’re good to go.’ I’ve been taking it for two years now. No issues. Why did I wait 25 years?
if you’re scared to get tested, just take one pill at home and see what happens 😅 i did and nothing happened. now i’m a penicillin believer. life’s too short for bad antibiotics.