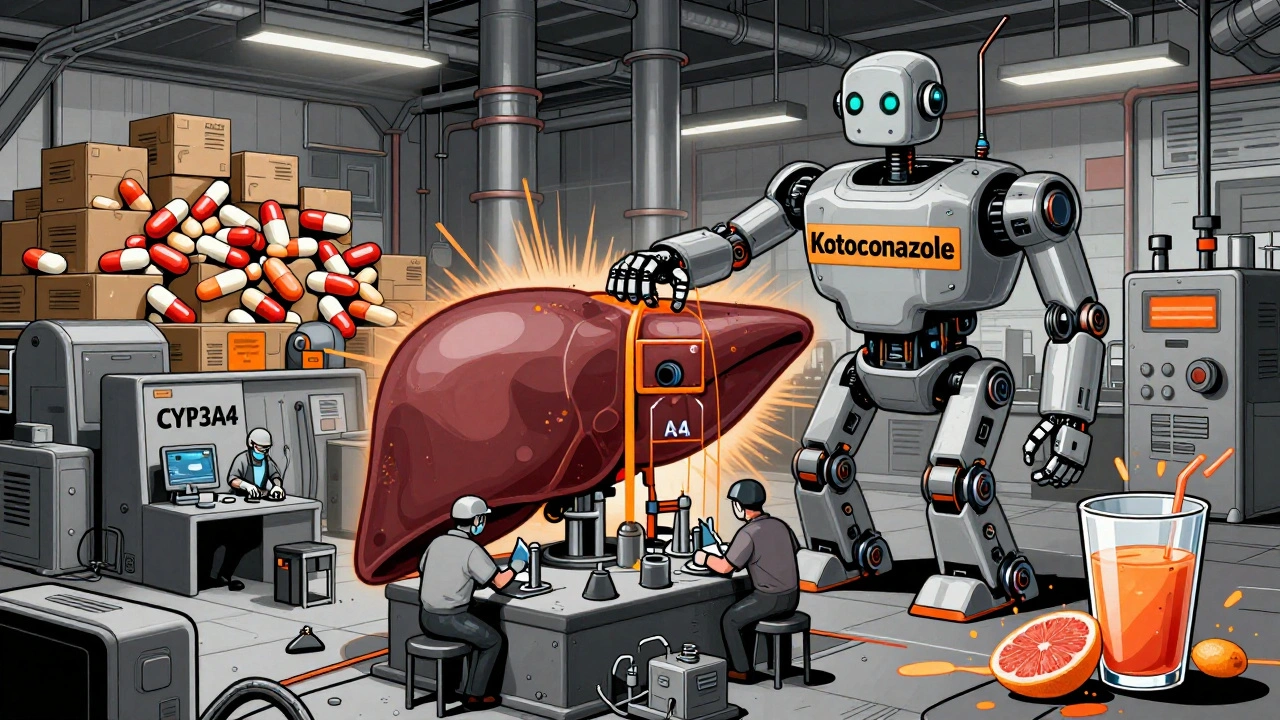
When you’re prescribed ketoconazole, it’s not just about taking the pill as directed. The real risk often comes from what you mix it with-other meds, supplements, even your morning coffee or grapefruit juice. Ketoconazole is an antifungal that can seriously mess with how your body processes other drugs. It doesn’t just sit there quietly. It blocks enzymes in your liver that break down a whole list of common medications. That means those drugs can build up to dangerous levels in your blood. And that’s when things go wrong.
Don’t Touch These Medications With Ketoconazole
Some drugs are absolute no-gos with ketoconazole. The list isn’t long, but every item on it can land you in the hospital.
First up: statins. If you’re on atorvastatin, simvastatin, or lovastatin for cholesterol, stopping ketoconazole is non-negotiable. These statins rely on the CYP3A4 enzyme to break down. Ketoconazole shuts that enzyme down. Result? Muscle breakdown, kidney failure, even death. A 2023 study in the Journal of Clinical Pharmacology showed patients on simvastatin and ketoconazole together had a 17-fold increase in muscle toxicity risk. Rosuvastatin and pravastatin are safer alternatives-your doctor can switch you.
Next: blood thinners. Warfarin is especially dangerous. Ketoconazole makes warfarin stick around longer in your body. Your INR can spike overnight. One patient in a 2022 case report had a brain bleed after starting ketoconazole while on warfarin. Even newer blood thinners like rivaroxaban and apixaban aren’t safe. They’re also broken down by CYP3A4. If you’re on any anticoagulant, ask for a different antifungal.
Then there’s sedatives and anti-anxiety meds. Midazolam, triazolam, alprazolam-these can turn deadly when paired with ketoconazole. You might feel overly drowsy, confused, or have trouble breathing. A 2021 review in Pharmacotherapy found that 38% of patients on ketoconazole and benzodiazepines needed emergency care for respiratory depression.
And don’t forget QT-prolonging drugs. Things like amiodarone, quetiapine, or certain antibiotics like moxifloxacin. Ketoconazole itself can lengthen the QT interval on your ECG. Add another one, and you’re flirting with torsades de pointes-a life-threatening heart rhythm. If you’ve ever had a heart rhythm issue, this combo is a hard pass.
Alcohol and Ketoconazole: A Risky Mix
Yes, you can drink alcohol while on ketoconazole-but you shouldn’t. It’s not that the two directly clash like some drug pairs. The danger is indirect but real.
Ketoconazole can cause liver stress. Alcohol does the same. Together, they pile on the damage. A 2024 study from the New Zealand Liver Foundation tracked 89 patients on oral ketoconazole. Of those who drank more than two standard drinks a day, 22% developed elevated liver enzymes within two weeks. Four needed hospitalization. Even moderate drinking can delay recovery.
It’s not just about getting a hangover. Your liver is already working overtime to process ketoconazole. Adding alcohol is like asking a tired worker to carry two heavy boxes instead of one. The result? Fatigue, nausea, jaundice. If you notice yellowing eyes or dark urine, stop alcohol and call your doctor immediately.
Grapefruit Juice and Other Citrus Traps
You’ve probably heard grapefruit juice interferes with meds. With ketoconazole, it’s not just a warning-it’s a red flag.
Grapefruit juice blocks the same liver enzyme (CYP3A4) that ketoconazole blocks. That means double the inhibition. Your body can’t clear other drugs properly. Even one glass can cause a spike in drug levels that lasts over 24 hours. It’s not just grapefruit. Seville oranges, pomelos, and some tangelos do the same thing.
And it’s not just juice. Some citrus-flavored candies, supplements, or even flavored teas might contain bergamot or bitter orange extracts. These can trigger the same reaction. If you’re unsure, check the ingredient list. If it says “citrus extract” or “bitter orange,” skip it.
Herbs, Supplements, and Natural Products
Just because something’s natural doesn’t mean it’s safe with ketoconazole.
St. John’s wort is a big one. It’s used for mild depression, but it speeds up the breakdown of drugs. Ketoconazole needs that enzyme to be slow. St. John’s wort fights against it, making ketoconazole less effective. You could end up with a fungal infection that won’t go away.
Other risky supplements: garlic pills (can thin blood), goldenseal (blocks CYP3A4), and high-dose vitamin E (can increase bleeding risk). Even milk thistle-often taken for liver health-can interfere with how ketoconazole is metabolized. There’s no clear data on whether it helps or hurts, but why risk it?
Always tell your pharmacist or doctor about every supplement you take. Even the ones you’ve been using for years. They might seem harmless, but with ketoconazole, they’re not.
What About Food and Timing?
Ketoconazole needs stomach acid to be absorbed. That means taking it with food can reduce its effectiveness. But not all food is bad.
Take ketoconazole on an empty stomach-ideally one hour before breakfast. If you’re taking the tablet form, avoid high-fat meals. Fat slows absorption. A 2020 study showed absorption dropped by 40% when taken with a fatty meal.
But if you’re on the liquid form (Nizoral suspension), it’s different. That version is designed to be taken with food to help absorption. Always check the label or ask your pharmacist. Mixing up the form and timing can mean the difference between treatment success and failure.
Also, avoid antacids, H2 blockers (like ranitidine), or proton pump inhibitors (like omeprazole) for at least two hours before or after your dose. These reduce stomach acid and make ketoconazole useless.

What to Do If You’ve Already Mixed Something
If you accidentally took a statin, drank grapefruit juice, or had a few drinks while on ketoconazole, don’t panic. But don’t ignore it either.
Stop the risky substance immediately. Call your doctor or pharmacist. Tell them exactly what you took, when, and how much. They may want to check your liver enzymes, kidney function, or heart rhythm.
If you feel dizzy, confused, have chest pain, or notice muscle weakness or dark urine, go to the emergency room. These aren’t normal side effects-they’re warning signs.
Keep a list of everything you’re taking. Write down meds, supplements, even herbal teas. Bring it to every appointment. It’s the best way to avoid a bad interaction before it happens.
Alternatives to Ketoconazole
If your doctor prescribed ketoconazole because it’s the only option for your fungal infection, ask if there’s another way. In many cases, there is.
For skin infections: terbinafine, clotrimazole, or ciclopirox creams work just as well and don’t interact with other drugs.
For oral thrush: fluconazole is often preferred. It’s safer, easier to use, and has fewer interactions.
For systemic fungal infections: voriconazole or isavuconazole are newer options with better safety profiles. They’re more expensive, but if you’re on multiple medications, the risk of ketoconazole may not be worth it.
Your doctor might not bring this up because ketoconazole is cheap and widely available. But if you’re on blood pressure meds, antidepressants, or anything else regularly, it’s worth asking: Is there a safer alternative?
Final Checklist: What to Avoid
- Statins: atorvastatin, simvastatin, lovastatin
- Blood thinners: warfarin, rivaroxaban, apixaban
- Sedatives: midazolam, triazolam, alprazolam
- QT-prolonging drugs: amiodarone, moxifloxacin, quetiapine
- Grapefruit, pomelo, Seville oranges
- Alcohol: more than one drink per day
- St. John’s wort, goldenseal, high-dose vitamin E
- Antacids or acid reducers within two hours of dose
- Fatty meals if taking the tablet form
If you’re unsure about anything, ask your pharmacist. They’re trained to spot these interactions. Don’t rely on memory or Google. Write it down. Keep the list in your wallet or phone. It could save your life.
Can I take ketoconazole with ibuprofen?
Yes, ibuprofen is generally safe with ketoconazole. It doesn’t rely on the CYP3A4 enzyme for metabolism, so there’s no major interaction. But both can irritate your stomach, so take them with food if you’re prone to ulcers. Avoid long-term use of high-dose ibuprofen while on ketoconazole, especially if you have liver or kidney issues.
Is ketoconazole safe if I have liver disease?
No. Ketoconazole is not recommended for people with active liver disease or elevated liver enzymes. It’s processed by the liver, and it can cause further damage. If you have a history of hepatitis, cirrhosis, or alcohol-related liver issues, your doctor should choose a different antifungal. Always get your liver enzymes checked before starting ketoconazole.
How long do ketoconazole interactions last after stopping the drug?
Ketoconazole’s effects on liver enzymes can last up to two weeks after your last dose. That means even after you stop taking it, you’re still at risk for interactions with other drugs. Don’t restart statins, sedatives, or blood thinners until your doctor says it’s safe. Wait at least 14 days and get a blood test if you’re on a high-risk medication.
Can I use ketoconazole shampoo while taking oral ketoconazole?
Yes. The shampoo form is applied topically and absorbed in tiny amounts-far too little to cause systemic interactions. You can safely use ketoconazole shampoo for dandruff or scalp fungus while taking the oral version. Just don’t swallow it. Rinse thoroughly.
What should I do if I miss a dose of ketoconazole?
Take it as soon as you remember, but only if it’s still before your next scheduled dose. If it’s close to your next dose, skip the missed one. Don’t double up. Missing doses can reduce effectiveness and lead to resistant fungus. If you miss more than two doses in a row, call your doctor. You may need to restart the course or switch medications.
If you’re on multiple medications, consider using a pill organizer with time labels. Set phone reminders for when to take ketoconazole and when to avoid other substances. Small habits like this prevent big problems. Your body is doing enough just to heal-you don’t need to make it harder.






10 Comments
Ketoconazole and statins are a death combo. Simvastatin alone can wreck your muscles. Add this antifungal and you're playing Russian roulette with your kidneys. No joke. I've seen it in ER.
It is absolutely imperative that patients, and indeed their caregivers, be made fully aware of the profound metabolic implications of concurrent ketoconazole administration with any substance metabolized via the CYP3A4 pathway. The pharmacokinetic alterations are not merely theoretical-they are clinically significant, potentially lethal, and entirely preventable with vigilant monitoring and interdisciplinary communication. I cannot stress this enough: patient safety hinges on precision.
man this is wild i never knew grapefruit juice could mess with meds like this. i drink it every morning. now i gotta check every label. also st johns wort? i take that for my mood. hmm. thanks for the heads up bro
Why does America let this crap fly? We have safer antifungals but doctors still prescribe ketoconazole because it's cheap. Meanwhile, people die because they don't know the risks. This isn't healthcare-it's corporate negligence. We need regulation, not warnings.
Existential question: if a drug interaction kills you in a forest and no one’s monitoring your INR… does it make a sound? 🤔 Also, grapefruit juice is the silent assassin of modern pharmacology. 🍊💀
The CYP3A4 enzyme is the linchpin of hepatic xenobiotic metabolism-ketoconazole’s inhibition of this isoform doesn’t merely alter pharmacokinetics; it orchestrates a cascade of iatrogenic catastrophe. One must appreciate the elegance of this biochemical sabotage… and then immediately avoid it at all costs.
They’re hiding the truth. Big Pharma knows ketoconazole is dangerous. That’s why they pushed it for years-profit over people. And now they’re slapping on warnings like it’s enough. Wake up. This is controlled poisoning.
lol this whole thing is fake. ketoconazole is fine. i took it with grapefruit and statins for 3 months. no prob. the real danger is doctors overreacting. you dont need to be scared of every little thing. the body can handle it.
Good breakdown. I’m on blood pressure meds and was about to take this for a rash. Glad I checked. I’ll print this list and stick it on my fridge. Small steps save lives.
I’m a pharmacist in Chicago and I see this every week. Someone comes in with a new ketoconazole script and says, ‘My doctor said it’s fine.’ Then they list 7 other meds. I always say: ‘Let’s call your doctor together.’ Most don’t know the risks. This post? Perfect. Share it. Save someone.