Statin Exercise Safety Calculator
Statin Exercise Safety Calculator
Find out if your exercise plan is safe based on your statin type and dose
When you're on statins and want to stay active, the fear of muscle pain can stop you before you even lace up your shoes. You’ve heard the warnings: statins cause muscle aches. You’ve also heard that exercise is medicine. So what’s the truth? Can you still run, walk, lift, or bike without risking serious damage? The answer isn’t simple-but it’s not as scary as you might think.
Statins and Muscle Pain: It’s Not Always the Statin
About 5 to 10% of people on statins report muscle pain, but real-world numbers suggest it could be as high as 29%. That’s a big gap. Why? Because not all muscle soreness comes from the drug. Many people start statins around the same time they begin a new workout, gain weight, or hit middle age-all common causes of muscle discomfort. The pain often shows up within 30 days of starting the medication, but it doesn’t always get worse with activity. True statin-related pain is constant, dull, and doesn’t go away with rest. Exercise-induced pain, on the other hand, shows up after a hard session and fades in a day or two.Not All Statins Are Created Equal
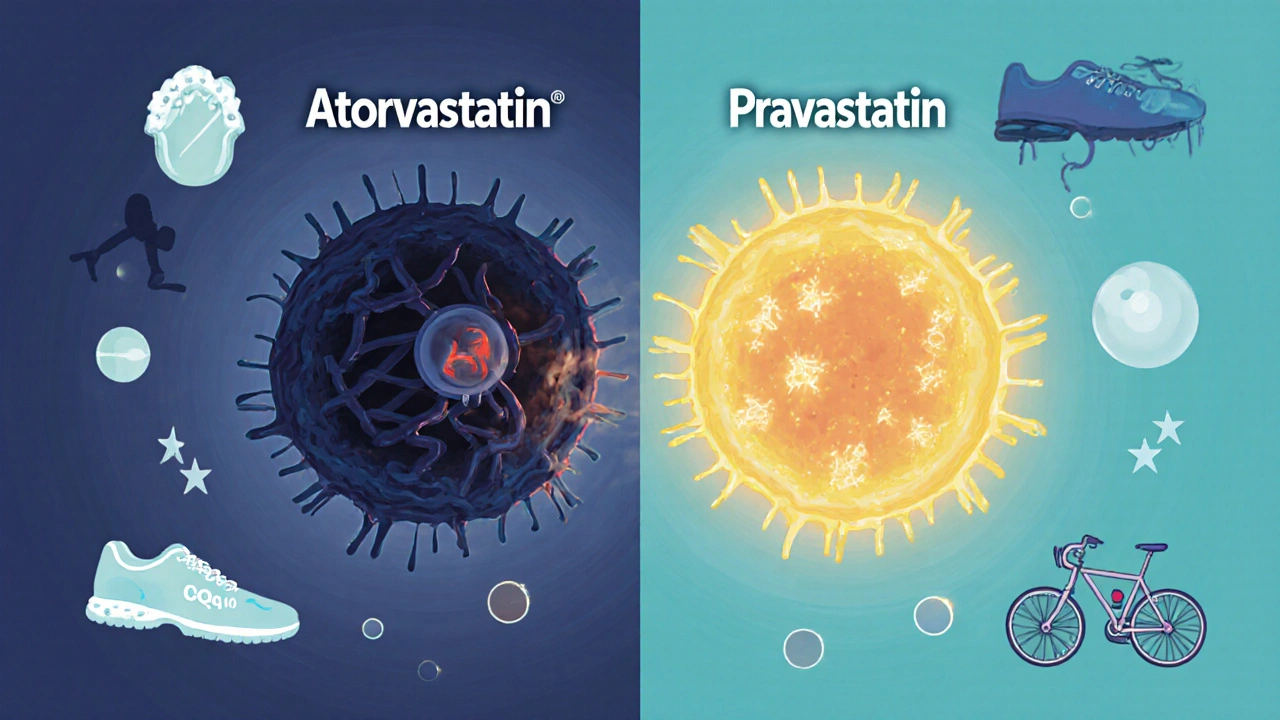
The type of statin you take matters a lot. Lipophilic statins like atorvastatin, a cholesterol-lowering drug that easily enters muscle tissue, increasing the risk of muscle symptoms, and simvastatin, a high-dose statin linked to a 10.5-fold higher risk of muscle damage compared to pravastatin, are more likely to cause issues. They slip into muscle cells more easily, disrupting energy production by lowering coenzyme Q10 (CoQ10) levels by up to 40% within a month. Hydrophilic statins like pravastatin, a water-soluble statin with lower muscle penetration and fewer side effects and rosuvastatin, a statin with minimal muscle uptake and lower risk of myopathy, are much gentler on muscles. A 2023 study found that switching from atorvastatin to rosuvastatin helped marathon runners keep training without pain. If you’re struggling, talk to your doctor about switching-65% of people see improvement.Exercise: Friend or Foe?
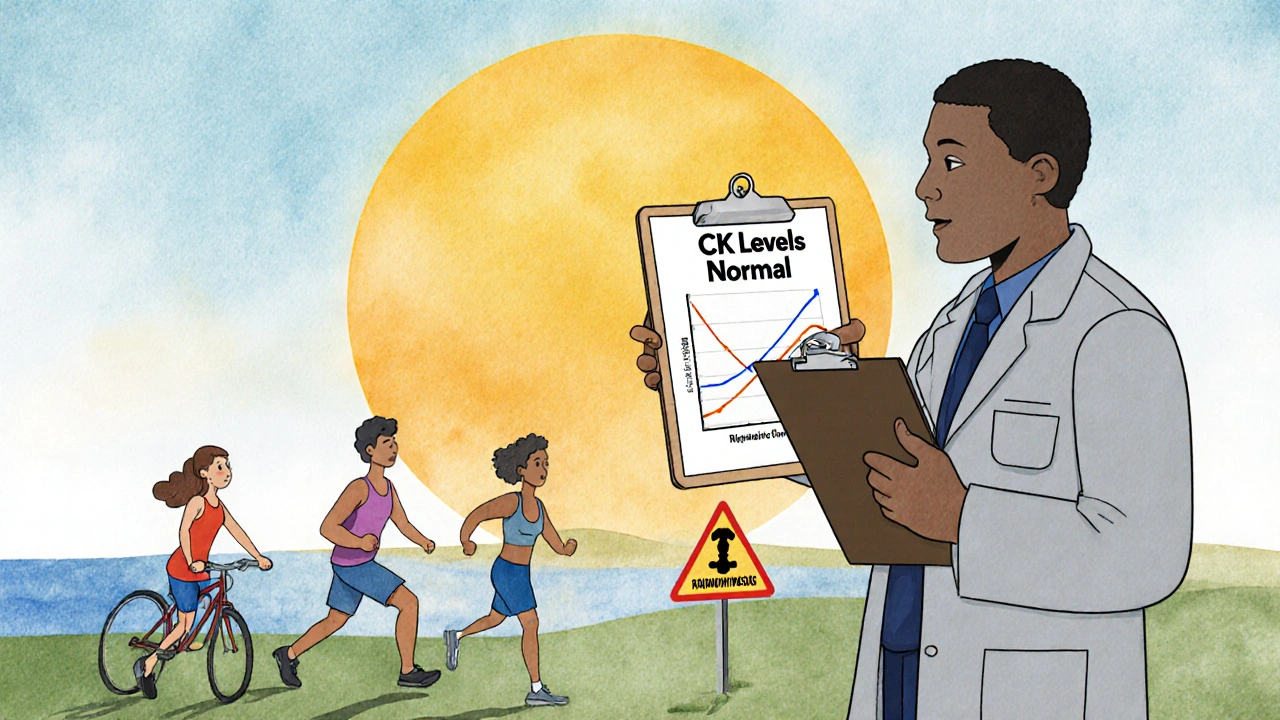
Here’s the good news: moderate exercise doesn’t make statin muscle pain worse. A 2023 study from Radboud University Medical Center tracked 105 people-some on statins with pain, some without, some not on statins at all. Everyone did 30 minutes of moderate cycling. Muscle damage markers like creatine kinase (CK) didn’t spike higher in statin users. In fact, their numbers were nearly identical to those not taking statins. The danger comes with intensity. High-dose statins combined with intense, eccentric exercise-like downhill running, heavy weightlifting, or HIIT-can push CK levels dangerously high. One cyclist, Maria Rodriguez, ended up in the hospital with CK levels of 12,450 U/L (normal is 30-200) after combining high-dose simvastatin with intense training. That’s rhabdomyolysis, a rare but life-threatening condition. The 4Days Marches study in the Netherlands gave 100 athletes statins and had them walk 30-50 km a day for four days. Their CK levels rose, but so did everyone else’s. No difference. That’s proof that long, steady, moderate activity is safe-even for people with muscle symptoms.What Intensity Is Safe?
Stick to moderate exercise. That means:- Walking at a pace where you can talk but not sing
- Cycling on flat ground, not climbing hills hard
- Swimming or using an elliptical with light resistance
- Staying at 40-70% of your maximum heart rate
- High-intensity interval training (HIIT)
- Heavy eccentric lifts (like deep squats or plyometrics)
- Marathons or ultra-endurance events if you’re on high-dose lipophilic statins
What If You Already Have Muscle Pain?
Don’t quit. Quitting exercise is worse than the pain. A 2023 survey found 61% of statin users stopped moving after muscle pain started. That increases heart disease risk-exactly what statins are meant to prevent. Start slow. The American College of Cardiology recommends:- Begin with 10-15 minutes of walking daily at a comfortable pace
- Gradually add 5 minutes per week
- Only increase intensity when pain doesn’t return
Can You Still Get Fit on Statins?
Yes-but your gains might be slower. A 2013 study found people on simvastatin improved their VO2 max (a measure of aerobic fitness) 6.9% less than those on placebo after 12 weeks of training. High-dose atorvastatin reduced mitochondrial efficiency by 15% in another trial. That doesn’t mean you can’t get stronger or fitter-it means you might need to train smarter, not harder. John Davis, a marathoner profiled in Runner’s World, kept running 40 miles a week after switching from atorvastatin to rosuvastatin. He didn’t lose his performance-he just changed his medication.Supplements and Other Fixes
CoQ10 supplements (200 mg daily) are often recommended. They don’t cure everything, but a 2023 meta-analysis showed they improved muscle symptoms in 40% of users. It’s low-risk and may help with energy production. Other strategies:- Switch to a lower dose or take statin every other day (58% success rate)
- Try a hydrophilic statin (65% success rate)
- Use graded exercise programs (72% success rate)
Genetics Play a Role
Some people are just more sensitive. The SLCO1B1 gene variant, found in about 1 in 10 people, increases the risk of muscle pain during exercise by 2.3 times. If you’ve had bad reactions to statins before, genetic testing might be worth discussing. By 2030, this could become standard practice.What Doctors Are Saying Now
The message from top medical groups has shifted. The American College of Cardiology now says: “Moderate exercise is safe for statin users, even those with muscle symptoms.” The American College of Sports Medicine adds: “Don’t stop moving-adjust your plan.” Dr. Michelina Catacola, lead author of the 2023 JACC study, put it plainly: “Statin therapy does not augment exercise-induced muscle injury.” The real risk isn’t exercise. It’s inactivity.Final Takeaway: Move-But Move Smart
Statins save lives. Exercise saves more. You don’t have to choose between them. Most people can-and should-keep moving. The key is matching your activity to your medication. If you’re on a high-dose lipophilic statin like atorvastatin or simvastatin, avoid HIIT and heavy lifting. Stick to walking, swimming, cycling on flat terrain. If you’re on pravastatin or rosuvastatin, you have more freedom. Start slow. Listen to your body. Don’t ignore pain that lingers. Talk to your doctor about switching statins or adding CoQ10. And don’t let fear stop you from moving. The best thing you can do for your heart isn’t a pill-it’s getting up and walking.Can I still run marathons if I take statins?
Yes-but it depends on the statin and your history. High-dose atorvastatin or simvastatin users should avoid long-distance events due to higher risk of rhabdomyolysis. Switching to rosuvastatin or pravastatin reduces that risk significantly. Marathon runners who continue training often do so after switching statins or reducing dosage. Always monitor for dark urine, extreme weakness, or prolonged pain after long runs. Get CK levels checked if symptoms appear.
Does CoQ10 really help with statin muscle pain?
It helps some people, but not everyone. Studies show about 40% of users report reduced pain with 200 mg of CoQ10 daily. It doesn’t fix the root cause, but it may improve muscle energy production since statins lower your body’s natural CoQ10 levels. It’s low-risk and worth trying if you’re experiencing discomfort. Don’t expect miracles, but many find it makes a noticeable difference in daily movement.
How do I know if my muscle pain is from statins or exercise?
Statin pain is constant, dull, and present even on rest days-it usually starts within 30 days of starting the drug. Exercise pain comes on after activity, feels sore or stiff, and fades within 48 hours. If pain appears after a new workout and goes away with rest, it’s likely exercise-related. If it’s there all the time, especially in your thighs or shoulders, it’s more likely statin-related. Tracking your symptoms over time helps your doctor tell the difference.
Should I stop exercising if I have statin muscle pain?
No. Stopping exercise increases your risk of heart attack and stroke more than continuing it with modifications. The goal is to adjust-not quit. Start with low-intensity walking, build slowly, avoid high-risk activities like HIIT or heavy lifting, and work with your doctor to check your statin type and dose. Most people can return to regular activity within weeks with the right plan.
What’s the safest statin for active people?
Pravastatin and rosuvastatin are the safest choices for active individuals. They don’t penetrate muscle tissue as deeply as atorvastatin or simvastatin, so they’re less likely to cause muscle pain. A 2022 FDA analysis found atorvastatin 80 mg carries a 10.5-fold higher risk of muscle damage than pravastatin 40 mg. If you’re active and experiencing side effects, ask your doctor about switching to one of these hydrophilic statins.
Can statins permanently damage muscles?
Rarely. Most muscle symptoms go away once the statin is stopped or switched. Permanent damage only happens in extreme cases like rhabdomyolysis, where muscle tissue breaks down severely and releases toxins into the blood. This is very rare-less than 1 in 10,000 users-and usually occurs with high doses, intense exercise, or other risk factors like kidney disease or older age. With proper monitoring and smart exercise, permanent damage is avoidable.










14 Comments
i literally started statins last month and began walking 30 mins a day-now my thighs feel like they’re full of wet cement. i thought it was just aging, but now i’m wondering if it’s the pill. thanks for this post, it’s the first time i’ve heard someone say it might not be the exercise.
While the article presents a compelling case for the safety of moderate exercise in statin users, one must remain cognizant of the potential for individual variability in pharmacokinetic response. The distinction between lipophilic and hydrophilic statins is clinically significant and warrants personalized therapeutic consideration.
Yo, let’s be real-statins are basically the silent muscle thieves of middle age. 😅 But here’s the twist: moving your body doesn’t make it worse, it makes you *aware*. I switched from atorvastatin to rosuvastatin and went from ‘can’t climb stairs’ to ‘doing 10Ks on weekends.’ CoQ10? Yeah, I take it like vitamins. Not magic, but it’s like giving your mitochondria a pep talk. Don’t quit. Just switch gears. Your heart will thank you. 🏃♂️💪
Wait-so if you’re on simvastatin and do HIIT, you could end up in the ER with CK levels over 12,000? That’s insane! I’ve been doing CrossFit on 40mg atorvastatin for two years and never thought twice. I’m getting my levels checked tomorrow. This post literally saved me from a medical nightmare. Thank you. 🙏
statins are just big pharma’s way of making you pay for being lazy and then telling you to exercise more so you dont sue them. also coq10 is just sugar pills with a fancy name. the real cause of muscle pain? too much sitting and too much processed food. they dont want you to know that. also why are there so many studies from 2023? coincidence? i think not
You don’t have to be a marathoner to beat heart disease-you just have to move. I’m 68, on pravastatin, and walk 5 miles every morning. My knees creak, my back groans, but my blood pressure? Perfect. My doctor says I’m the poster child for ‘smart movement.’ If you’re scared, start with 10 minutes. Do it. Then do it again tomorrow. That’s how you win.
Let’s not romanticize this. Exercise on statins is like driving a car with worn brakes-you can still get somewhere, but you’re playing Russian roulette with your muscle tissue. The studies say ‘safe,’ but safety is a statistical abstraction. Your body isn’t a dataset. If your muscles ache, stop. Don’t ‘adjust.’ Don’t ‘try CoQ10.’ Just stop. Your heart doesn’t need you to suffer to prove you’re disciplined.
Another ‘statins are fine if you’re careful’ article. Where’s the data on long-term mitochondrial damage? Where’s the follow-up on people who switched statins and still had chronic fatigue? This is corporate medicine dressed up as empowerment. They don’t want you to know that 20% of statin users quit because they felt like zombies. And now they’re telling you to ‘walk more’ like it’s a virtue. Wake up.
I’ve been on rosuvastatin for 5 years and walk 6 days a week. I used to get cramps in my calves at night. After reading this, I cut out evening HIIT and added a 200mg CoQ10. The cramps? Gone. Not a miracle, but a shift. I just wish my doctor had mentioned this earlier. To anyone scared: you’re not broken. You just need to tweak the plan. Talk to your doc. Try one thing at a time. You’ve got this.
OH MY GOD I’M NOT ALONE!!! I thought I was just getting old and weak… I’ve been on atorvastatin for 3 years and stopped biking because my legs felt like jelly. I cried. I felt like a failure. Then I read this and switched to rosuvastatin last week. Today I rode 20 miles. I’m sobbing again-but this time from joy. Thank you. 🥹❤️
As a physical therapist who works with cardiac patients, I see this every day. The fear of muscle pain leads to deconditioning, which increases cardiovascular risk more than the statin itself. The key is structured, graded progression-start low, go slow, track symptoms. Many patients think they need to ‘push through’ pain, but it’s about listening. Small wins build confidence. And yes, switching statins works more often than people realize.
Of course exercise is ‘safe’-the CDC and AMA are in bed with Big Pharma. Why else would they tell you to move more while you’re on a drug that drains your energy? You think they care about your heart? They care about your insurance premiums. Walk if you want. But don’t believe the hype. The truth? Statins are overprescribed, and exercise is the scapegoat.
OMG I’ve been saying this for YEARS. Statins are poison. My cousin’s husband died from rhabdo after a hike. And now they want us to walk more? That’s like telling someone with a bullet wound to go for a jog. CoQ10? That’s just a placebo. The real fix? Get off the statin. Ditch the processed carbs. Eat real food. But no one wants to say that because it’s not profitable. I’m not a doctor but I play one on Reddit. 🤡
Just switched from simvastatin to pravastatin last month and started walking again 🚶♂️✨ CoQ10 + low intensity = life back. No more 3-day muscle hangovers. Also, if you’re reading this and scared? You’re not alone. Talk to your doc. Try one change. Celebrate tiny wins. You’re doing better than you think 💪❤️