What CPAP and BiPAP Actually Do
Both CPAP and BiPAP machines help you breathe better while you sleep. They push air through a mask to keep your airway open so you don’t stop breathing during the night. This is critical for people with sleep apnea - a condition where breathing pauses again and again, often dozens of times an hour. Without treatment, those pauses strain your heart, wreck your sleep, and leave you exhausted even after a full night in bed.
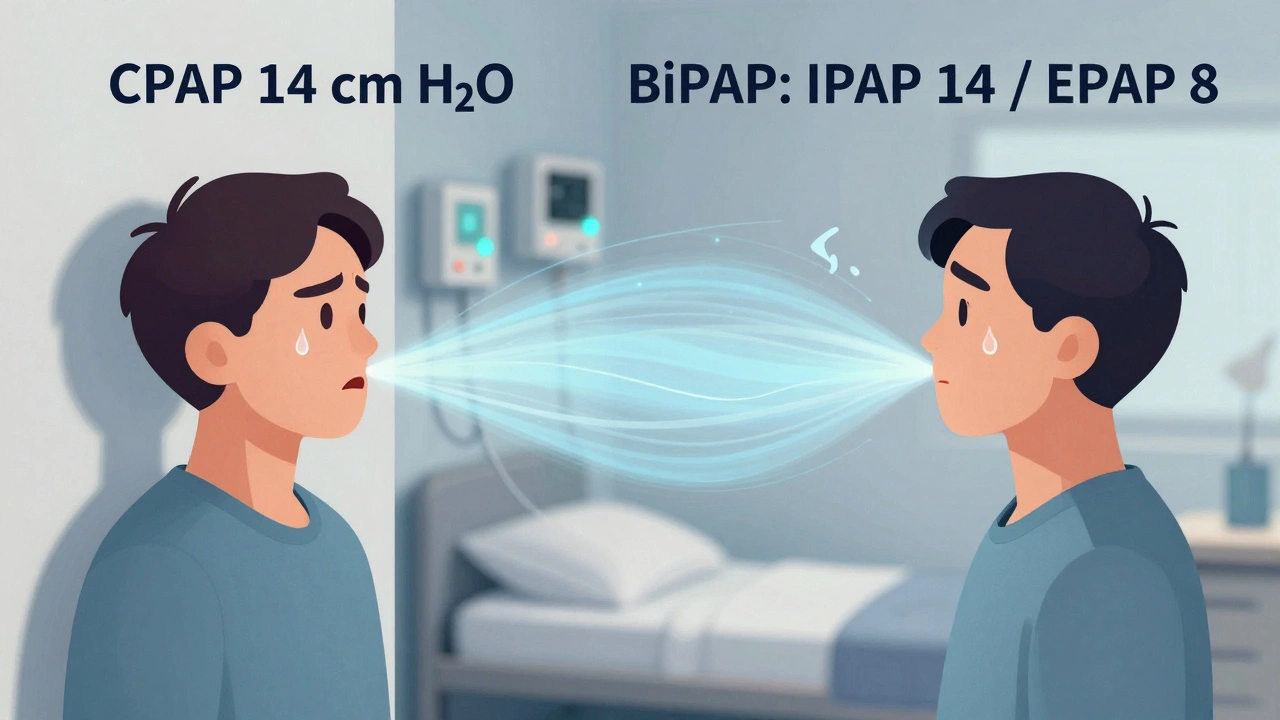
CPAP stands for Continuous Positive Airway Pressure. It delivers one steady pressure all night long - whether you’re inhaling or exhaling. Think of it like a gentle, constant breeze holding your throat open. BiPAP, short for Bilevel Positive Airway Pressure, gives you two different pressures: a higher one when you breathe in (called IPAP), and a lower one when you breathe out (called EPAP). That difference makes it easier to exhale, especially if you’re used to fighting against high pressure.
The machines look similar - small boxes with tubes and masks - but inside, they’re built for different jobs. CPAP has been the go-to for over 40 years. It’s simple, reliable, and works for most people with obstructive sleep apnea. BiPAP came later, designed for those who struggle with CPAP’s constant pressure or have other breathing problems beyond just a collapsed airway.
How Pressure Settings Work
CPAP pressure is set between 4 and 25 cm H₂O, and it stays the same all night. Most people need between 8 and 15 cm H₂O, but your doctor won’t guess - they’ll find the right level during a sleep study. That’s when you sleep overnight in a lab with sensors tracking your breathing, heart rate, and oxygen levels. The machine adjusts pressure until your apneas stop.
BiPAP is more complex. It uses two numbers: IPAP (inhalation pressure) and EPAP (exhalation pressure). IPAP usually runs between 8 and 30 cm H₂O, while EPAP sits between 4 and 25 cm H₂O. The gap between them - called pressure support - must be at least 3 cm H₂O to work properly. For example, a common setting might be IPAP 14 / EPAP 8. That means you get 14 cm H₂O when you breathe in, then it drops to 8 when you breathe out. That 6 cm H₂O drop makes exhaling feel much easier.
Some BiPAP machines also have a backup rate. If you stop breathing for more than 20 seconds, the machine will force a breath. That’s crucial for people with central sleep apnea, where the brain forgets to tell the lungs to breathe. CPAP can’t do that. It only pushes air - it doesn’t create breaths.
Who Gets CPAP and Who Gets BiPAP
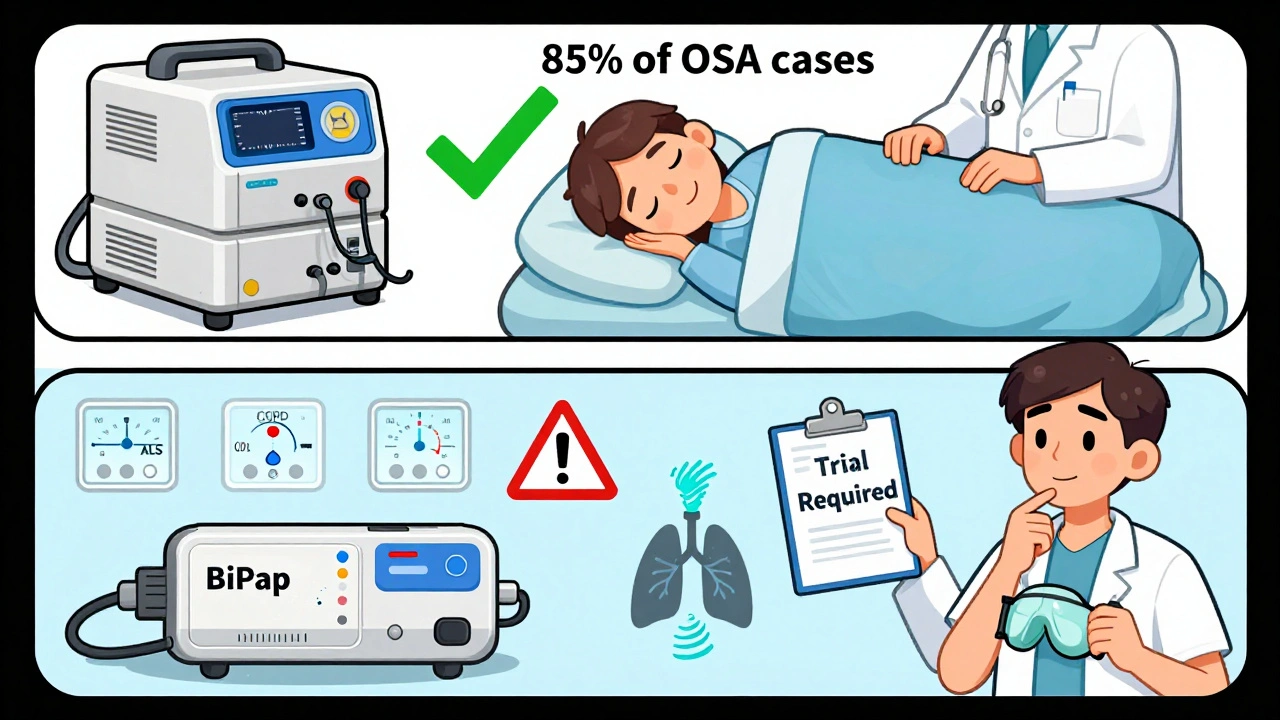
CPAP is the first choice for about 85% of people with obstructive sleep apnea. If your only problem is your throat closing during sleep, CPAP fixes it. It’s cheaper, simpler, and just as effective as BiPAP for most cases. Studies show both machines improve sleep quality and reduce daytime fatigue equally in standard OSA patients.
BiPAP is reserved for specific situations:
- You need high pressure (15 cm H₂O or more) and can’t tolerate it on CPAP
- You have COPD with high carbon dioxide levels in your blood (hypercapnia)
- You have central sleep apnea - your brain isn’t sending the right signals
- You have obesity hypoventilation syndrome (BMI over 30 with low oxygen during the day)
- You have a neuromuscular disease like ALS or muscular dystrophy
For example, someone with severe COPD might struggle to exhale against a high CPAP pressure. Their lungs are already stiff. BiPAP’s lower exhale pressure lets them push air out more easily. A person with central apnea might go 30 seconds without breathing on CPAP - but BiPAP’s backup breaths kick in and prevent that.
Some doctors now consider BiPAP as a first option for people with very severe OSA (AHI over 30) and high BMI, because the pressure relief can improve early use. But that’s still debated. Most guidelines still say: start with CPAP unless you have one of those specific conditions.
Cost, Insurance, and Accessibility
CPAP machines cost between $500 and $1,200. Basic models like the ResMed AirSense 10 retail around $899. BiPAP machines are pricier - $800 to $1,800. The Philips DreamStation BiPAP Auto sells for about $1,499. That’s not just the machine - it includes the humidifier, tubing, and mask.
Insurance coverage is where things get tricky. Medicare and most private insurers cover CPAP without much fuss if you’re diagnosed with OSA. But for BiPAP, they usually require proof you failed CPAP. That means you tried it for 30 days, used it at least 4 hours a night, and still couldn’t handle the pressure - especially if it was above 15 cm H₂O. Without that documentation, you’ll pay out of pocket.
Even if you get approved, BiPAP machines are harder to get. Fewer suppliers carry them. Sleep clinics often stock CPAP for convenience. BiPAP requires more training to set up, so not every respiratory therapist is comfortable handling it.
Real User Experiences
People who use CPAP often say it’s simple. They like that there’s only one setting to worry about. A 2023 survey of over 12,000 users found 78% were satisfied, and 62% used it 6+ hours a night. For many, the biggest win is waking up refreshed after years of feeling drained.
But users who switched to BiPAP after struggling with CPAP tell a different story. On Reddit’s r/CPAP community, one user wrote: ‘BiPAP at 14/8 felt like breathing normally. CPAP at 14 felt like choking.’ That’s common among people who needed high pressure. They say BiPAP made the difference between quitting therapy and sticking with it.
But BiPAP isn’t perfect. Some users say the machine feels ‘clunky’ - it doesn’t always sync with their breathing. One survey found 27% of BiPAP users complained about the machine cycling too early or too late. Others say the settings are confusing. If you accidentally change the backup rate or switch modes, the machine might not work right. CPAP doesn’t have those options - so there’s less to mess up.
What Happens After You Start
Getting used to either machine takes time. Most people need 2 to 4 weeks to adjust to CPAP. For BiPAP, it can take 3 to 6 weeks because of the added complexity. You’ll likely have a follow-up with your sleep specialist after 30 days. They’ll check your usage data - most modern machines upload this automatically to your provider’s portal.
Insurance requires you to use your device at least 4 hours a night for 70% of nights in the first 3 months. If you don’t meet that, they may stop covering it. About 65% of CPAP users hit that mark. For BiPAP users, it’s closer to 60%. That’s not because BiPAP doesn’t work - it’s because the setup is harder. If you’re struggling, don’t give up. Talk to your respiratory therapist. A better mask, adjusted humidity, or a different pressure setting can fix most problems.
Mask fit is the #1 reason people quit. Seven out of ten complaints about discomfort come from a poorly fitted mask. It doesn’t matter if you’re on CPAP or BiPAP - if air leaks, your therapy fails. Make sure your mask isn’t too tight. It should seal without pulling on your face. Many clinics offer mask fitting sessions. Use them.
The Bigger Picture: Technology and Trends
The sleep therapy market is growing fast. CPAP still makes up 68% of sales, but BiPAP is catching up. Newer models from ResMed and Philips now use AI to adjust pressure automatically. The ResMed AirCurve 10 VAuto, for example, changes IPAP and EPAP in real time based on your breathing patterns. That blurs the line between BiPAP and traditional machines.
Some devices now track your oxygen levels and even detect when you’re snoring or having a central apnea. That’s helpful, but it also means more data to understand. You don’t need to be a tech expert, but you do need to be willing to learn.
There’s a growing concern that BiPAP is being overused for simple OSA. One study estimated that inappropriate BiPAP prescriptions cost the U.S. healthcare system $420 million a year. That’s money spent on more expensive machines when CPAP would’ve worked fine. Doctors are getting better at choosing the right tool - but it still happens.
What to Do Next
If you’ve been diagnosed with sleep apnea, your doctor will likely start you on CPAP. Don’t assume you need BiPAP just because it sounds more advanced. It’s not. It’s for specific cases.
If you’ve tried CPAP and can’t tolerate it - especially if you’re gasping on exhale or your pressure is above 15 cm H₂O - talk to your sleep specialist about BiPAP. Ask for a trial. Some clinics let you test a BiPAP machine for a week before committing.
Either way, stick with it. The benefits are real: better sleep, lower blood pressure, less risk of heart attack, and more energy during the day. It’s not glamorous. But it works.






8 Comments
Been using a CPAP for 5 years now. Honestly? The mask fit is everything. I went through 7 different masks before finding the right one. Once it sealed right, I stopped waking up gasping and started actually sleeping. Don't overthink the machine type - get the right fit first. 😊
I switched to BiPAP after my CPAP pressure hit 18 and I felt like I was breathing through a straw. Game changer. Now I sleep 7+ hours straight. Also, the auto-adjust feature on my new ResMed? Pure magic. 🤖💤
The entire CPAP/BiPAP discourse is a capitalist mirage. We’ve reduced the sublime act of breathing - a biological symphony - to algorithmic pressure gradients and insurance-driven compliance metrics. BiPAP isn’t a machine; it’s a symptom of our failure to address the ontological rupture between the body and the medical-industrial complex. Your exhale is not a variable to be optimized.
Everyone says CPAP is the first line, but let’s be real - most docs just prescribe it because it’s cheap and they don’t wanna deal with the paperwork for BiPAP. I had a guy with AHI 45 and BMI 42 on CPAP at 20 cm H₂O for 8 months. He was miserable. BiPAP would’ve saved him a year of suffering. Stop pretending CPAP is always enough.
Sleep apnea isn’t just a breathing problem - it’s a life interruption. I used to wake up 20 times a night. Now, with BiPAP at 16/9, I dream again. I remember what it feels like to wake up without a headache. This isn’t about machines. It’s about reclaiming your nights. You owe it to yourself to keep trying. The first week sucks. The second week? Better. Third week? You’ll thank yourself.
I tried CPAP for 3 weeks and gave up. I felt like I was suffocating. My wife said I was snoring louder than before. I cried. I felt like a failure. Then I got BiPAP. The difference? It’s like my lungs finally remembered how to breathe. I don’t care what the guidelines say. This saved my marriage. My life. My sanity.
BiPAP is just CPAP with extra buttons and a higher price tag. Most people don’t need it. I saw a guy on Reddit who switched to BiPAP because he didn’t like the noise. Bro. It’s a fan. Get over it. Stop letting marketing trick you into thinking more features = better sleep. CPAP works. Use it. Stop whining. 🤷♂️
The real tragedy isn’t the machine. It’s that we treat sleep as a technical problem to be solved by devices, rather than a sacred ritual to be honored. We’ve turned rest into a KPI. Your CPAP compliance rate is not your worth. Your breath is not a metric. You are not a data point. Breathe. Just breathe.