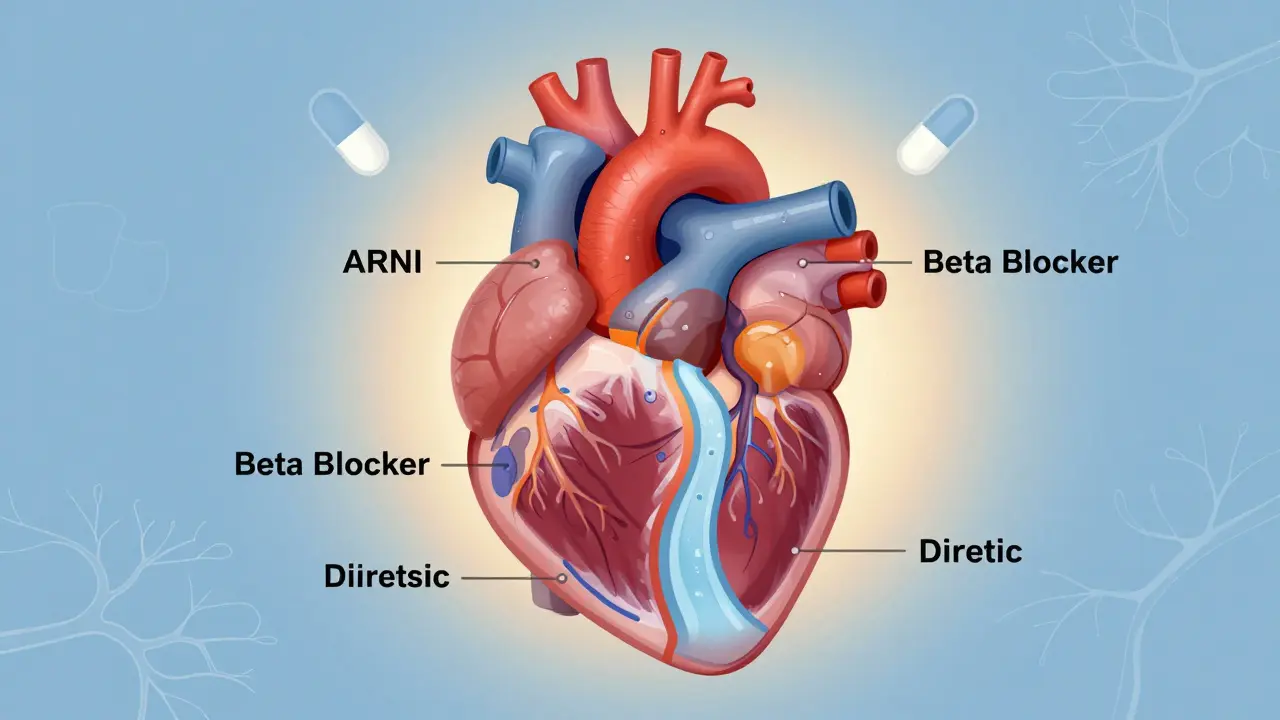
Heart failure isn’t a single disease-it’s a condition where the heart can’t pump enough blood to meet your body’s needs. And while it sounds scary, modern medicine has made huge strides in helping people live longer, feel better, and avoid hospital stays. At the core of this progress are four key drug classes: ACE inhibitors, ARNIs, beta blockers, and diuretics. Together, they form what doctors now call guideline-directed medical therapy-the best, most proven way to treat heart failure with reduced ejection fraction (HFrEF).
What ACE Inhibitors Do and How They Work
ACE inhibitors were the first real game-changer in heart failure treatment. Back in the 1980s, studies like the CONSENSUS trial showed that enalapril cut death rates by 27% in people with severe heart failure. That was revolutionary. Today, drugs like lisinopril, enalapril, and ramipril are still widely used because they block a hormone system called RAAS-the same one that raises blood pressure and makes the heart work harder.
By stopping the body from turning angiotensin I into angiotensin II, ACE inhibitors relax blood vessels, lower blood pressure, and reduce the strain on the heart. That means less fatigue, less shortness of breath, and better long-term survival. But they’re not perfect. About 1 in 5 people get a dry, annoying cough. Some develop high potassium levels, which can be dangerous. And in rare cases (less than 1%), people get angioedema-a sudden swelling of the face or throat that needs emergency care.
Start doses are low: lisinopril at 2.5-5 mg daily, enalapril at 2.5 mg twice daily. Doctors slowly increase the dose every few weeks, aiming for the highest tolerated amount. If you can’t handle the cough, you might switch to something else.
Why ARNI Is Now the Gold Standard
If ACE inhibitors were the first big step, ARNIs are the leap forward. The drug sacubitril/valsartan (brand name Entresto) was approved in 2015 after the PARADIGM-HF trial proved it was better than enalapril. In that study of nearly 8,400 people across 47 countries, ARNI reduced the risk of death or hospitalization from heart failure by 20%. That’s more than any new heart drug in decades.
What makes ARNI special? It’s a two-in-one pill. Sacubitril blocks an enzyme called neprilysin, which lets your body keep more of its own natural heart-protecting chemicals (natriuretic peptides). These help you pee out extra fluid, relax blood vessels, and reduce heart stress. Valsartan blocks angiotensin receptors, just like an ARB. Together, they do more than ACE inhibitors alone.
Doctors now recommend ARNI as the first choice for most people with HFrEF-unless you’ve just been on an ACE inhibitor. You must wait at least 36 hours after stopping an ACEI before starting ARNI. Why? Mixing them too soon raises the risk of angioedema. Start with 24/26 mg twice daily, and double the dose every 2-4 weeks if your blood pressure stays above 100 mmHg. Side effects? Dizziness, low blood pressure, and high potassium. But most people stick with it because they feel better: less breathless, more energy.
Beta Blockers: Slowing Down to Save the Heart
It sounds backwards, right? Give a heart failure patient a drug that slows the heart? But beta blockers like carvedilol, metoprolol succinate, and bisoprolol aren’t just for high blood pressure. In heart failure, they protect the heart muscle from the damaging effects of stress hormones.
The CIBIS-II and MERIT-HF trials showed these drugs cut death rates by up to 34%. They improve the heart’s pumping ability over time-even if you feel worse at first. That’s why doctors start them at super low doses. Carvedilol begins at 3.125 mg twice daily. Metoprolol at 12.5 mg once a day. You might feel tired, dizzy, or have a slow pulse. That’s normal. The key is patience. Doses are doubled every 2-4 weeks, as long as you’re stable.
People on beta blockers report fatigue, especially early on. One Reddit user said, “I thought I was getting worse until my doctor explained it was the drug working.” Over months, many see their ejection fraction improve-from 25% to 45% or higher. The goal isn’t to make you feel great right away. It’s to help your heart heal.

Diuretics: Managing Fluid, Not Fixing the Heart
Diuretics don’t fix the broken heart. They fix the swelling. When your heart fails, fluid backs up in your lungs, legs, and belly. That’s why you’re short of breath, gain weight fast, or can’t sleep lying down. Diuretics help you pee out the extra fluid.
Loop diuretics like furosemide, torsemide, and bumetanide are the go-to. Furosemide starts at 20-80 mg daily. Torsemide is longer-lasting and may be more effective-studies show it lowers hospital readmissions by 18% compared to furosemide. Thiazides like hydrochlorothiazide are used for milder cases or combined with loops. And don’t forget spironolactone-it’s both a diuretic and a mineralocorticoid receptor antagonist (MRA). The RALES trial showed it cut death risk by 30% in severe heart failure.
But diuretics come with trade-offs. You’ll be running to the bathroom more. Some get leg cramps from low potassium or magnesium. One patient on PatientsLikeMe said, “I started taking potassium pills and magnesium supplements-my cramps vanished.” Blood tests are key: check potassium and kidney function every 1-2 weeks after starting or changing doses. Diuretics save your comfort. But they’re not a cure. They’re a tool to make life bearable while the other meds do the real healing.
How These Medications Work Together
These four drug classes aren’t meant to be used alone. The current standard is quadruple therapy: ARNI (or ACEI/ARB), beta blocker, MRA (like spironolactone), and SGLT2 inhibitor (like dapagliflozin). Diuretics are added as needed.
This combo reduces death risk by up to 20% and hospitalizations by 21%. But here’s the problem: only about 35% of eligible patients get all four drugs within a year of diagnosis. Why? Side effects, fear of low blood pressure, kidney issues, or just not knowing how to titrate doses safely.
Specialized heart failure clinics get it right 85% of the time. General practices? Only 52%. The gap isn’t about science-it’s about access, follow-up, and patient education. If you’re on these meds, make sure you’re seeing a heart failure specialist or a team that tracks your labs, symptoms, and doses closely.

Real People, Real Experiences
Behind every drug name is a person trying to live.
One user on Reddit switched from lisinopril to Entresto and said, “My shortness of breath improved in two weeks.” Another said furosemide gave him awful leg cramps until he added magnesium. A third shared, “Carvedilol made me tired for months-but now my ejection fraction is 45%. Worth it.”
On Amazon, ARNI has the highest rating (4.3/5), but people complain about the cost-$550 a month without insurance. Generic lisinopril? $4. Metoprolol? $6. That’s why many still start with ACEIs, even though ARNI is better. Insurance often requires prior authorization for Entresto. Medicare covers it, but only after paperwork.
Cost isn’t the only barrier. In rural areas, only 28% of eligible patients get guideline-recommended therapy. If you’re in a small town or on a tight budget, talk to your doctor about patient assistance programs. Many drugmakers offer discounts.
What to Watch For and When to Call Your Doctor
These meds work best when you’re monitored. Here’s what to track:
- Weight: Gain 2+ pounds in a day? That’s fluid. Call your doctor.
- Blood pressure: Systolic below 90? Dizziness? Your dose might be too high.
- Potassium: Above 5.0 mmol/L? Can be deadly. Get tested every 1-2 weeks after starting or changing meds.
- Creatinine: A 30% rise from baseline? Your kidneys may be struggling. Dose adjustment needed.
- Cough: If it’s persistent and dry, you might need to switch from ACEI to ARNI or ARB.
- Swelling or breathing trouble: If it’s getting worse despite meds, you may need a higher diuretic dose or hospital care.
Don’t stop these meds on your own-even if you feel better. Stopping beta blockers or ARNI suddenly can trigger dangerous heart rhythm problems or sudden worsening.
The Future: What’s Next?
Heart failure treatment keeps evolving. ARNI is now approved for people with mildly reduced ejection fraction (EF 41-49%), which opens the door for millions more. SGLT2 inhibitors, originally for diabetes, are now recommended for all heart failure patients-even those with preserved ejection fraction. And drugs like vericiguat are being added to the mix for those who still struggle.
By 2027, experts predict ARNI will be first-line for 70% of new HFrEF cases. But the real challenge isn’t the science-it’s making sure everyone gets it. Right now, too many people are stuck on old regimens because their doctors don’t know how to switch, or they can’t afford the new drugs.
If you or someone you love has heart failure, ask: Am I on the best combination? Am I getting monitored? Can I afford this? The tools exist. The science is clear. What’s missing is consistent, personalized care.
Can I take ACE inhibitors and ARNI together?
No. You must wait at least 36 hours after stopping an ACE inhibitor before starting ARNI. Taking them too close together increases the risk of angioedema-a serious swelling of the face, lips, or throat. Always follow your doctor’s timing instructions exactly.
Why do beta blockers make me feel so tired?
Beta blockers slow your heart rate and reduce the heart’s workload, which can cause fatigue, especially at first. This usually improves over weeks or months as your heart gets stronger. Don’t stop them unless your doctor advises it. If fatigue is severe, your dose may need adjusting-not stopping.
Are diuretics dangerous long-term?
Diuretics aren’t dangerous if monitored. The main risks are low potassium, low sodium, dehydration, and kidney strain. Regular blood tests and staying hydrated help prevent these. Many people take them for years without issues. But they don’t improve survival on their own-they’re for symptom relief while other meds treat the root cause.
Is ARNI worth the high cost?
Yes, for most people with HFrEF. ARNI reduces hospitalizations and death more than ACE inhibitors. While it costs $550/month without insurance, many drug manufacturers offer patient assistance programs. Medicare and private insurers often cover it after prior authorization. The long-term savings from fewer ER visits and hospital stays often outweigh the cost.
Can I stop my heart failure meds if I feel better?
Never stop without talking to your doctor. Feeling better means the meds are working. Stopping beta blockers or ARNI suddenly can cause dangerous heart rhythms or rapid worsening of heart failure. Even if you’re stable, these drugs need to be taken daily, for life.
What if I have kidney problems?
Kidney issues are common in heart failure, and they can limit the use of ACEIs, ARNIs, and MRAs because they raise potassium and affect kidney function. But that doesn’t mean you can’t use them. Your doctor will start low, monitor closely, and adjust doses. Many people with mild to moderate kidney disease still benefit safely from these drugs.





8 Comments
Really appreciate this breakdown-especially how you clarified that diuretics don't fix the heart, just the symptoms. So many people think popping a water pill is a cure, and it’s not. It’s like using a sponge to mop up a leaky pipe while ignoring the broken pipe itself.
I’ve seen patients on furosemide gain 10 pounds in two days and panic, not realizing it’s fluid, not fat. Tracking weight daily is the simplest, most powerful tool out there.
It’s appalling that anyone would still start with an ACE inhibitor when ARNI has been proven superior for over a decade. The PARADIGM-HF trial wasn’t a fluke-it was a paradigm shift. If your doctor hasn’t switched you to Entresto by now, they’re practicing medicine from 2008. And yes, I’m aware of the 36-hour washout. I’ve read the guidelines. Thoroughly. With footnotes.
Also, the cost argument is lazy. Yes, it’s $550 without insurance-but so is a single hospitalization for decompensated HF. Insurance companies know this. They just drag their feet because they can. Push back. File appeals. Call patient advocacy groups. This isn’t a luxury-it’s standard of care.
And for the love of all that’s medical, stop calling spironolactone a ‘diuretic’ like it’s just a fancy water pill. It’s an MRA. It blocks aldosterone. It reduces fibrosis. It saves lives. Terminology matters. If you can’t say ‘mineralocorticoid receptor antagonist,’ at least say ‘aldosterone antagonist.’ Don’t reduce science to slang.
As someone from Kenya who’s worked in cardiac care in rural clinics, I’ve seen firsthand how access gaps kill. In Lagos, a guy on lisinopril for years couldn’t get ARNI because the pharmacy didn’t stock it-and no one knew how to apply for the manufacturer’s program. Meanwhile, in Boston, someone gets it on day one because their PCP has a clinical pharmacist on staff.
This isn’t about science anymore. It’s about equity. We need community health workers trained to walk patients through prior auth forms. We need pharmacies that stock generics AND brand-name drugs side by side. We need telehealth follow-ups for folks who live 50 miles from the nearest cardiologist.
And honestly? The fact that only 35% of patients get quadruple therapy? That’s a system failure. Not a patient failure.
beta blockers make u tired??? no shit sherlock. lol
It’s funny how we treat heart failure like it’s a math problem you solve with pills-take A, then B, then C, and poof, you’re fixed. But the heart isn’t a car engine. It’s a living organ that remembers trauma, stress, grief. The meds help it heal, but they don’t erase the years of neglect, the fried diets, the 12-hour shifts, the sleepless nights raising kids while your own body screamed for help.
Maybe the real question isn’t ‘are you on the right drugs?’ but ‘did anyone ever teach you how to listen to your body before it broke?’
I’ve seen people on all four meds still feel broken. Not because the drugs failed. Because they were never taught they deserved to feel whole.
Have you ever considered that the entire heart failure drug paradigm is orchestrated by Big Pharma to keep people on lifelong meds? ACE inhibitors were pushed hard in the 90s, now ARNI is the new gold standard-same playbook. And don’t get me started on SGLT2 inhibitors being repurposed from diabetes drugs. Coincidence? Or is this just profit-driven medicalization disguised as science?
Also, why do all the trials have 47 countries? That’s a lot of data… but who’s funding it? And why do they never mention the placebo groups in the real-world outcomes? Just saying.
It is with profound respect for the scientific literature that I must respectfully submit, with due deference to the peer-reviewed evidence, that the assertion regarding the superiority of ARNI over ACE inhibitors, while statistically significant in the PARADIGM-HF cohort, may not be universally generalizable across all ethnic subpopulations, particularly those with non-European ancestry, wherein pharmacogenomic variability may influence drug metabolism and adverse event profiles.
Furthermore, the assertion that diuretics are merely symptomatic interventions is, in my considered opinion, an oversimplification. The renal hemodynamic modulation induced by loop diuretics, particularly in the context of neurohormonal activation, may exert downstream anti-remodeling effects that are underappreciated in current clinical discourse.
It is therefore imperative that clinicians exercise caution in adopting sweeping recommendations without individualized risk-benefit analysis.
Dr. Weber’s point about terminology is precisely correct. In clinical practice, precision in language prevents errors. Calling spironolactone a ‘diuretic’ without specifying its MRA mechanism invites confusion among nurses, pharmacists, and patients alike. It’s not pedantry-it’s patient safety.
Additionally, the 36-hour washout period for ARNI after ACEI is not arbitrary. It’s based on pharmacokinetic overlap of the angiotensin receptor blockade and neprilysin inhibition. The angioedema risk is real and documented in the FDA’s Adverse Event Reporting System.
Thank you for the thorough, evidence-based summary. This is the kind of clarity the field needs.