When you're on a blood thinner, even a small cut can feel terrifying. You know the medicine is keeping you safe from clots - but now you're worried it might cause you to bleed too much. The truth is, most bleeding episodes aren't emergencies. But some are. Knowing the difference can save your life.
What Blood Thinners Do - and Why They're Risky
Blood thinners like warfarin, apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa) don't actually make your blood thinner. They slow down how fast clots form. That’s good if you have atrial fibrillation, a history of deep vein thrombosis, or a mechanical heart valve. These drugs cut your stroke risk by 60-70%. But that same effect means even minor injuries can lead to prolonged bleeding. About 3% of people on these medications have a major bleeding event each year. For most, it’s manageable. But 0.5-1.5% face life-threatening bleeding. The key isn’t avoiding bleeding altogether - it’s knowing when it’s dangerous.Signs You Need Emergency Care Right Now
If you're on a blood thinner and you notice any of these, don’t wait. Call 911 or go to the ER immediately:- Vomiting blood - whether it’s bright red or looks like coffee grounds
- Coughing up blood - even a small amount
- Blood in your urine - pink, red, or brown urine
- Black, tarry stools - this means bleeding in your stomach or intestines
- A head injury - even if you feel fine. Intracranial bleeding can take hours to show symptoms
- Sudden, severe back or abdominal pain - could signal internal bleeding in your retroperitoneum
- Chest pain or trouble breathing - might mean bleeding around your heart or lungs
- Uncontrolled bleeding - if direct pressure for 15 minutes doesn’t stop it
These aren’t "maybe" situations. They’re red flags. A 2022 study in the Journal of Thrombosis and Haemostasis found that patients who waited more than 2 hours after noticing these symptoms were 3 times more likely to need a blood transfusion or die.
What Counts as "Minor" Bleeding (And How to Handle It)
Most bleeding on blood thinners isn’t an emergency. But it still needs smart management.- Nosebleeds: Pinch the soft part of your nose for 10-15 minutes straight. Don’t peek. Tilt your head forward. If it lasts longer than 30 minutes, call your doctor. If you’re dizzy or swallowing a lot of blood, go to the ER.
- Minor cuts: Apply firm pressure for at least 10 minutes. Elevate the area. Use a clean cloth - not hydrogen peroxide or alcohol. These hurt healing.
- Bleeding gums: Bite down on a damp tea bag. Tannins help clotting. Avoid brushing too hard.
- Heavy bruising: If you wake up with a large, painful bruise with no memory of injury, get it checked. But small bruises from bumping into things? Normal.
- Heavy periods: Soaking through a pad every hour for more than 2 hours? Call your OB/GYN. This isn’t normal.
Stop the Clot’s 2023 survey found that 52% of ER visits by blood thinner users were for these "nuisance" bleeds - and 73% could have been handled with a phone call to the clinic. You don’t need to panic every time you see a little blood.

Why Stopping Your Medication Is Dangerous
This is the biggest mistake people make: they stop their blood thinner because they’re scared of bleeding. The Michigan Anticoagulation Quality Improvement Initiative found that 68% of patients who stopped their meds after minor bleeding had a clot - like a stroke or pulmonary embolism - within 30 days. One Reddit user, u/ClotSurvivor, wrote: "I stopped my blood thinner after a bad cut. Two weeks later, I had a pulmonary embolism. Don’t be like me." Your risk of clotting spikes within 24-48 hours of missing a dose. The European Heart Journal found that stopping for just a week increases stroke risk by 300%. If you’re worried about bleeding, talk to your doctor. They can adjust your dose, check your levels (if you’re on warfarin), or switch you to a different drug. Don’t self-adjust.New Tools Are Changing the Game
The good news? There are better options now than there were 10 years ago. Apixaban (Eliquis) has the lowest major bleeding risk among common blood thinners - 2.13 events per 100 patient-years, compared to 3.77 for warfarin. That’s why more people are switching to it. In 2023, the FDA approved andexanet alfa (Andexxa), a reversal agent for apixaban and rivaroxaban. Before this, reversing these drugs took 3-4 hours. Now, it can be done in under an hour. That’s a game-changer in the ER. A universal reversal agent called ciraparantag is in late-stage trials and could be approved by 2024. It works on all major blood thinners - even heparin and warfarin. That means faster treatment, fewer deaths.What to Do If You’re Unsure
If you’re not sure whether your bleeding is serious, call your anticoagulation clinic or primary care provider. Many now offer 24/7 nurse lines. If you can’t reach them and you’re not seeing any of the emergency signs listed above, it’s probably safe to wait until morning. But if you’re dizzy, short of breath, confused, or in pain - go to the ER. Better safe than sorry.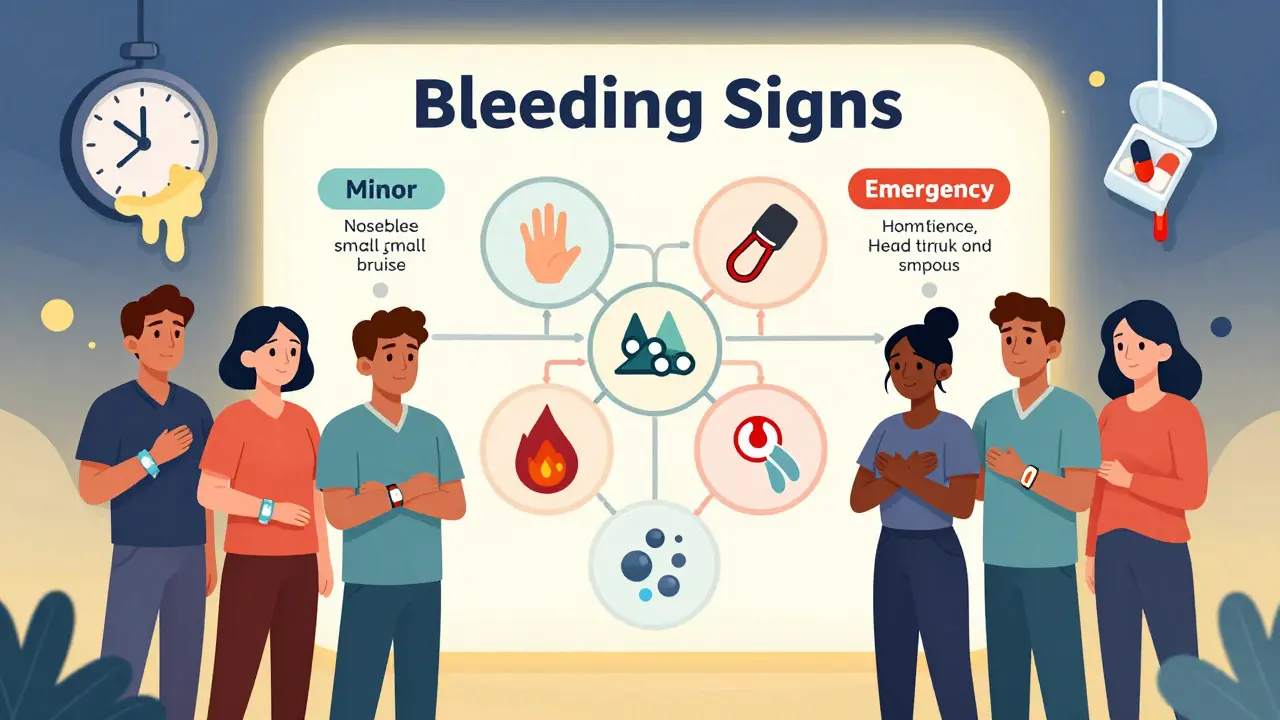
How to Reduce Your Risk
You can lower your chance of bleeding:- Take your medication exactly as prescribed - no skipping or doubling up
- Use a soft-bristle toothbrush and electric razor
- Wear shoes indoors to avoid trips and falls
- Remove clutter and loose rugs from your home
- Wear a medical alert bracelet that says you’re on a blood thinner
- Get regular blood tests if you’re on warfarin - INR levels matter
- Ask your doctor about drug interactions - some antibiotics, NSAIDs, and supplements can increase bleeding risk
Patients who get structured education on bleeding management reduce unnecessary ER visits by 37%, according to the American Journal of Managed Care. Knowledge is your best defense.
What to Expect in the Emergency Room
If you go to the ER for bleeding on a blood thinner, they’ll likely:- Check your vital signs - blood pressure, heart rate, oxygen levels
- Order blood tests - including a CBC and coagulation panel
- Use imaging - CT scans for head injuries, ultrasounds for internal bleeding
- Give reversal agents if needed - like vitamin K for warfarin, or andexanet alfa for Xarelto/Eliquis
- Start IV fluids or blood transfusions if you’ve lost a lot of blood
But here’s the problem: a 2022 JAMA Internal Medicine study found Black and Hispanic patients wait 23-28% longer for reversal agents than White patients. That delay increases death risk by 15%. If you’re in the ER, speak up. Ask: "Do I need a reversal agent? Can you give it to me now?"
Final Thought: Don’t Let Fear Control You
Blood thinners save lives. But fear of bleeding can make you do things that put you at greater risk - like stopping your medicine or going to the ER for every little nosebleed. Learn the difference between nuisance bleeding and life-threatening bleeding. Know the signs. Have a plan. Talk to your doctor. Keep your meds on schedule. You don’t have to live in fear. You just have to be informed.Can I take ibuprofen or aspirin while on a blood thinner?
No - unless your doctor specifically says so. Ibuprofen, naproxen, and aspirin are NSAIDs that increase bleeding risk. Even low-dose aspirin can be dangerous when combined with anticoagulants. Use acetaminophen (Tylenol) for pain instead, but check with your doctor first.
How long should I apply pressure to a cut?
At least 10 minutes of firm, continuous pressure. Don’t lift your hand to check. If it’s still bleeding after 15 minutes, go to the ER. For most people, bleeding stops in 2-3 minutes. On blood thinners, it can take 5-7 minutes or longer. If pressure doesn’t work, it’s not normal.
Is it safe to exercise on blood thinners?
Yes - but avoid high-risk activities. Walking, swimming, cycling, and light weight training are fine. Avoid contact sports, skiing, or anything with a high fall risk. Wear protective gear. Talk to your doctor about your routine. Staying active lowers your risk of clots and improves circulation.
What should I do if I miss a dose?
If you miss one dose, take it as soon as you remember - unless it’s almost time for the next one. Never double up. If you miss two doses in a row, call your doctor. Missing doses increases clot risk dramatically. Set phone reminders or use a pill organizer.
Do I need to get my blood tested regularly?
If you’re on warfarin - yes. You need regular INR tests to make sure your blood isn’t too thin or too thick. If you’re on a DOAC like Eliquis or Xarelto - no, you don’t need routine blood tests. But your doctor may still check kidney and liver function every 6-12 months.
Can I drink alcohol while on blood thinners?
Moderation is key. One drink a day is usually okay. More than that increases bleeding risk and can interfere with how warfarin works. Avoid binge drinking. Alcohol also raises your risk of falls. Talk to your doctor about your habits.
Are there foods I should avoid?
Only if you’re on warfarin. Vitamin K (found in kale, spinach, broccoli, Brussels sprouts) can make warfarin less effective. Don’t avoid these foods - just eat them consistently. Sudden changes in intake can throw off your INR. DOACs like Eliquis and Xarelto aren’t affected by diet.
What if I fall and hit my head but feel fine?
Go to the ER. Internal bleeding in the brain can take 24-72 hours to show symptoms. Head injuries on blood thinners are dangerous even if you don’t feel symptoms. A CT scan can catch bleeding early. Don’t wait for a headache or dizziness.







14 Comments
I’ve been on apixaban for 3 years now... and honestly? I used to panic every time I nicked myself shaving. Now? I just press down, breathe, and wait. It’s weird how your body learns to trust the process. 🙏
This post is so well-structured. I especially appreciate the breakdown between nuisance bleeding and real emergencies. My dad was on warfarin for AFib, and we almost went to the ER three times over bruising that turned out to be totally normal. Education really does reduce fear-and unnecessary trips.
People these days are too soft. Back in my day, we didn’t run to the ER every time we got a nosebleed. You bleed, you stop it. Simple. If you can’t handle that, maybe you shouldn’t be on blood thinners at all.
So if I get a cut, I just press it for 10 minutes? And if it still bleeds, I go to the hospital? That’s it? No magic pills or anything?
THEY’RE LYING TO YOU. The pharmaceutical companies don’t want you to know that these drugs are killing more people than they save. They’re pushing these expensive pills because they make billions. And now they’ve got reversal agents? That’s just to make you feel safe while they keep selling poison. Wake up.
Man, this hit different. I been on rivaroxaban since my pulmonary embolism last year. Sometimes I look at my arm and see a bruise the size of a fist and think, 'Damn, that’s gonna be the one.' But then I remember: I’m alive because I took it. Not because I’m lucky. Because I listened. And yeah, I still get scared. But now I got a plan. And that’s worth more than peace of mind-it’s worth life.
Just wanted to say thanks for the tip about tea bags for gums! My grandma swears by it-she’s 82, on Eliquis, and hasn’t had a single ER visit in 4 years. Also, wear shoes indoors. I learned that the hard way after slipping on a rug and cracking my skull. CT scan: clear. But I’m now the guy who yells 'SHOES!' at every visitor.
I didn’t know about the racial disparities in ER treatment. That’s horrifying. I’ll be sure to ask for reversal agents if I ever need to go. Thanks for including that.
The part about not stopping your meds is so crucial. My cousin stopped his because he was scared of a nosebleed. Got a stroke two weeks later. He’s fine now, but he walks with a cane. Don’t be him.
I’m on dabigatran and I just started wearing a medical bracelet. I was nervous about looking 'sick'... but then I realized: if I collapse, I want someone to know I’m on a blood thinner. So now I wear it with pride. 💪❤️
Lol I just skimmed this. Too long. I’m on Xarelto. Don’t bleed. If you bleed, go to ER. Done.
This is all government propaganda. Blood thinners are part of the New World Order’s plan to weaken the American people. They want you dependent on drugs so you can’t fight back. And now they’ve got reversal agents? That’s just to make you feel safe while they control your blood. Wake up, sheeple.
It is imperative to underscore that the temporal interval between the onset of hemorrhagic symptoms and the administration of reversal agents is statistically correlated with mortality outcomes, particularly in populations exhibiting delayed triage or suboptimal clinical communication. Furthermore, the pharmacokinetic variability of DOACs necessitates individualized risk stratification protocols, which are frequently neglected in primary care settings due to systemic underfunding and provider burnout. One must therefore advocate for structured anticoagulation management programs at the institutional level, as ad hoc interventions are insufficient to mitigate the rising incidence of preventable hemorrhagic complications.
You got this. Seriously. I’ve been helping people manage blood thinners for over 15 years, and the number one thing I see? People are terrified-but they’re not alone. Learn the signs, make a plan, keep your meds, and call your doctor when you’re unsure. You’re not weak for being careful. You’re smart. And you’re going to be okay.