Why Your Antifungal Might Not Be Working
If you’re taking a proton pump inhibitor (PPI) like omeprazole or pantoprazole for heartburn-and also an antifungal like itraconazole for a fungal infection-you could be fighting a silent battle inside your stomach. The very drug meant to calm your acid might be quietly starving your antifungal of what it needs to work. This isn’t speculation. It’s documented, measurable, and happening to thousands of people every month.
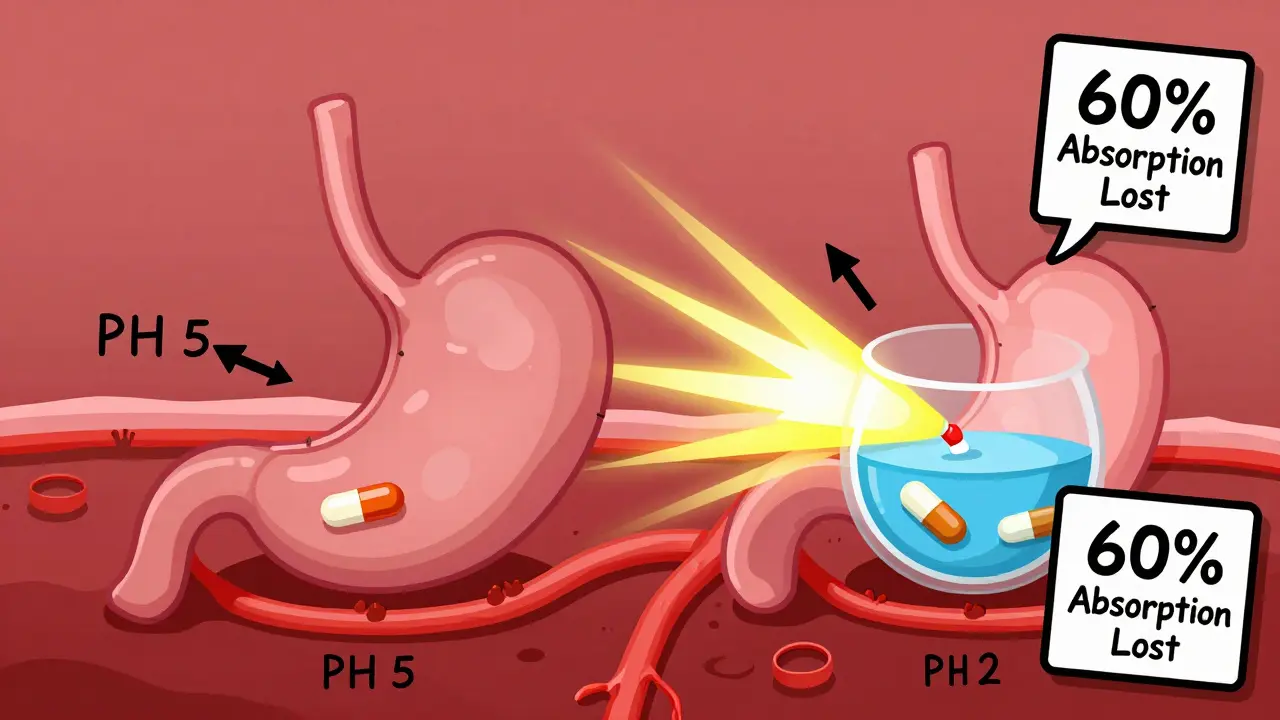
Take itraconazole, one of the most common antifungals used for serious infections like aspergillosis or coccidioidomycosis. It’s a weak base. That means it needs a low pH-below 3-to dissolve properly in your stomach. Without that acidic environment, it just sits there, undissolved, and gets passed through your gut without being absorbed. PPIs raise your stomach pH to 4-6. That’s not just a little change. It’s enough to drop itraconazole absorption by 50-60%. That’s not a minor reduction. That’s treatment failure territory.
The Real Numbers Behind the Interaction
Studies show clear, hard numbers. When omeprazole is taken with itraconazole capsules, the area under the curve (AUC)-a measure of total drug exposure over time-plummets by 60%. That means your body gets less than half the drug it’s supposed to. In one case, a patient with chronic pulmonary aspergillosis had itraconazole levels of just 0.3 mcg/mL. After switching from omeprazole to famotidine, levels jumped to 1.7 mcg/mL. That’s a five-fold increase. And it wasn’t luck. It was physics.
Not all antifungals are affected the same way. Fluconazole? No problem. It’s highly water-soluble and doesn’t care what your stomach pH is. Voriconazole? It takes a hit-about 22% lower exposure with PPIs. Posaconazole delayed-release tablets? Down 40%. But here’s the twist: posaconazole oral suspension doesn’t drop as much. Why? Because it’s already in liquid form. It doesn’t rely on stomach acid to dissolve.
The solution form of itraconazole-liquid, not capsules-also avoids this issue. It’s pre-dissolved. So if you’re on a PPI and need itraconazole, ask your doctor: Can we switch to the solution? That’s not just a workaround. That’s a proven fix.
PPIs vs. H2 Blockers vs. Antacids
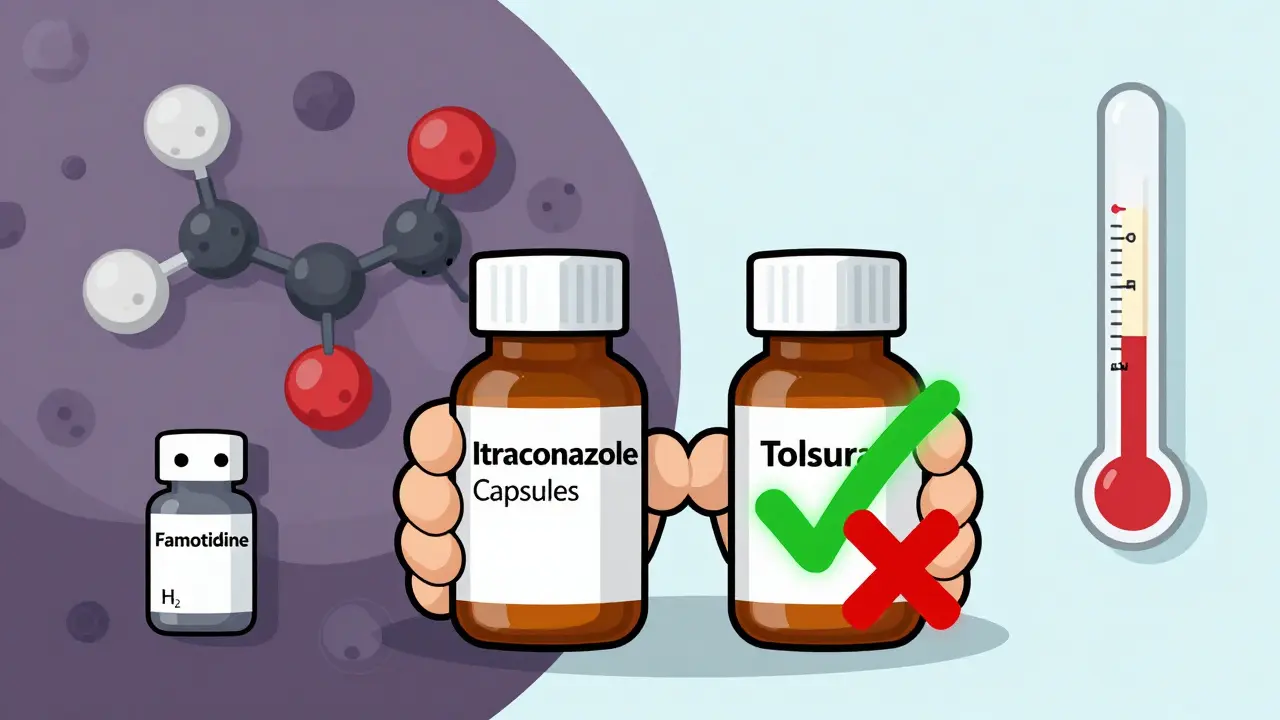
Not all acid reducers are created equal. PPIs shut down acid production for 12-24 hours. That’s a long time. H2 blockers like famotidine only last 4-10 hours. Studies show omeprazole cuts itraconazole AUC by 57%. Famotidine? Just 41%. That’s a big difference.
Antacids? They work fast but don’t last. If you take Tums or Maalox two hours before or after your antifungal, the impact is minimal. The timing matters. PPIs? They’re a constant background hum of high pH. You can’t time around them.
So if you need acid suppression while on a pH-sensitive antifungal, H2 blockers are your better bet. But even then, give it a 10-hour window after your antifungal dose. Don’t just take them together.
What About Newer Formulations?
There’s good news on the horizon. In 2023, the FDA approved a new version of itraconazole called Tolsura. Unlike the old capsules, it’s designed to absorb without needing stomach acid. With PPIs, its absorption drops by only 8%-not 60%. That’s a game-changer.
For patients who’ve had multiple treatment failures or are on long-term PPIs, Tolsura is now the preferred option. It’s not cheap, but it’s worth it if your life depends on this drug working. Ask your pharmacist: Is Tolsura an option for you?
The Hidden Risk: Subtherapeutic Levels Create Resistance
Here’s the scary part. If your antifungal levels are too low, you’re not just failing treatment-you’re breeding resistance.
The European Committee on Antimicrobial Susceptibility Testing (EUCAST) warned in 2021 that low drug concentrations from PPI interactions can turn a susceptible fungal strain into a resistant one. That means the fungus survives, mutates, and comes back stronger. Now you need a stronger drug. Maybe one with more side effects. Maybe one that’s more expensive. Maybe one that doesn’t even exist yet.
This isn’t theoretical. There are documented cases where patients with invasive aspergillosis failed treatment because their itraconazole levels were too low-due to PPIs-and later developed resistant strains. That’s not just a drug interaction. That’s a public health concern.
What Can You Actually Do?
Here’s your action plan:
- Check your antifungal. Is it itraconazole capsules? Posaconazole delayed-release tablets? Voriconazole? These are the ones at risk.
- Check your acid reducer. Are you on omeprazole, esomeprazole, lansoprazole, pantoprazole? If yes, you need to act.
- Don’t stop your PPI without talking to your doctor. If you’re on a PPI for a bleeding ulcer or severe GERD, stopping it could be dangerous.
- Ask about switching to the itraconazole solution or Tolsura. These avoid the interaction entirely.
- Ask about switching to famotidine. If you still need acid suppression, H2 blockers are safer.
- Ask about therapeutic drug monitoring. For itraconazole, levels should be 0.5-1.0 mcg/mL. If you’re below that, your dose isn’t working.
One hospital pharmacist in Massachusetts reported that 68% of pharmacists see at least one of these interactions every month. That’s not rare. That’s routine. And too often, it’s missed.

The Unexpected Twist: Could PPIs Help?
Here’s where it gets weird. In a 2025 lab study, researchers found that when omeprazole and itraconazole were mixed together in a petri dish, they killed 77.6% of resistant fungal strains-even those that had survived other antifungals. The same combo worked against azole-resistant Aspergillus fumigatus.
That’s not a mistake. That’s synergy. The same mechanism that blocks absorption in the gut might be enhancing antifungal action in the bloodstream. Researchers at the NIH are now testing low-dose omeprazole with subtherapeutic itraconazole in early-phase clinical trials (NCT05678901). If this works, we might be looking at a new way to treat resistant fungal infections.
But don’t try this at home. This is still experimental. The dose, timing, and patient selection are being carefully studied. What we know for sure is that taking your PPI and antifungal together at random won’t help. It’ll just make things worse.
Who’s at Risk?
You’re more likely to face this interaction if:
- You’re over 65 (PPI use jumps sharply after 60)
- You’re hospitalized (5-7% of inpatients get systemic antifungals)
- You have cancer, HIV, or are on immunosuppressants
- You’ve been on a PPI for more than 3 months
- You’ve had a fungal infection that didn’t improve
Medicare data shows 38.7% of patients prescribed itraconazole capsules also got a PPI in the same month. Only 12.3% of those on itraconazole solution did. That gap tells you something: some doctors know. But many don’t.
The Bottom Line
This interaction isn’t a footnote. It’s a major clinical problem. It costs the U.S. healthcare system $287 million a year in wasted drugs and failed treatments. It leads to hospital readmissions. It creates drug-resistant fungi. And it’s often invisible-because no one checks.
If you’re on a PPI and an antifungal, ask these questions:
- Is my antifungal affected by stomach acid?
- Is there a version of this drug that doesn’t need acid to work?
- Can I switch to famotidine instead of my PPI?
- Can we check my drug levels?
Don’t assume your doctor knows. Don’t assume your pharmacist caught it. This interaction is so common, it’s almost expected. But that doesn’t make it okay. It makes it urgent.
One simple change-switching from itraconazole capsules to the solution, or from omeprazole to famotidine-could mean the difference between recovery and relapse. Don’t wait for a failure to happen. Ask now.
Can I take omeprazole and itraconazole together?
No, not if you’re using itraconazole capsules. Taking them together can reduce itraconazole absorption by up to 60%, making the drug ineffective. If you must take both, switch to the itraconazole solution or Tolsura-these formulations aren’t affected by stomach pH. If you need acid control, use famotidine instead of omeprazole, and take it at least 10 hours after your antifungal.
Does fluconazole interact with PPIs?
No. Fluconazole is highly water-soluble and doesn’t rely on stomach acid for absorption. It works just as well whether you’re on omeprazole, pantoprazole, or nothing at all. You can take fluconazole with a PPI without worrying about reduced effectiveness.
Why does itraconazole need stomach acid to work?
Itraconazole is a weak base. That means it dissolves best in an acidic environment (pH below 3). PPIs raise stomach pH to 4-6, which prevents the drug from dissolving properly. If it doesn’t dissolve, your body can’t absorb it. That’s why capsules fail-but the liquid solution, which is already dissolved, still works.
What’s the difference between itraconazole capsules and solution?
Itraconazole capsules require stomach acid to dissolve and release the drug. The solution is already in liquid form and doesn’t need acid. With PPIs, capsules lose 50-60% of their absorption. The solution only loses 10-15%. That’s why the solution is preferred when PPIs are needed.
Can PPIs make fungal infections worse?
Yes, indirectly. By lowering antifungal drug levels, PPIs can cause treatment failure. That lets the fungus survive and possibly develop resistance. Once resistant, the infection becomes harder-or impossible-to treat with standard drugs. This is why experts warn that PPIs can turn a treatable infection into a life-threatening one.
Should I stop my PPI if I need an antifungal?
Don’t stop it on your own. If you’re on a PPI for a serious condition like a bleeding ulcer or Barrett’s esophagus, stopping it could be dangerous. Instead, talk to your doctor about switching to an antifungal that doesn’t need acid (like fluconazole or itraconazole solution) or switching your acid reducer to famotidine. Your doctor can weigh the risks of stopping the PPI versus the risk of antifungal failure.
Is there a new antifungal that doesn’t interact with PPIs?
Yes. Tolsura, a newer form of itraconazole approved in 2023, is designed to absorb without needing stomach acid. With PPIs, its absorption drops by only 8%, compared to 60% for regular capsules. If you’re on long-term PPI therapy and need itraconazole, Tolsura is now the preferred option.