Every year, thousands of people in the U.S. are harmed or die because someone gave them the wrong medication - not because the drug was bad, but because the name, strength, or dosage form was misread. It’s not always a doctor’s mistake. Sometimes it’s a nurse rushing, a pharmacist misreading a handwritten script, or a patient taking a pill because it looked like the one they took yesterday. These errors are preventable. And the fix starts with one simple habit: always check the medication name, strength, and dosage form - every single time.
Why This Check Isn’t Optional
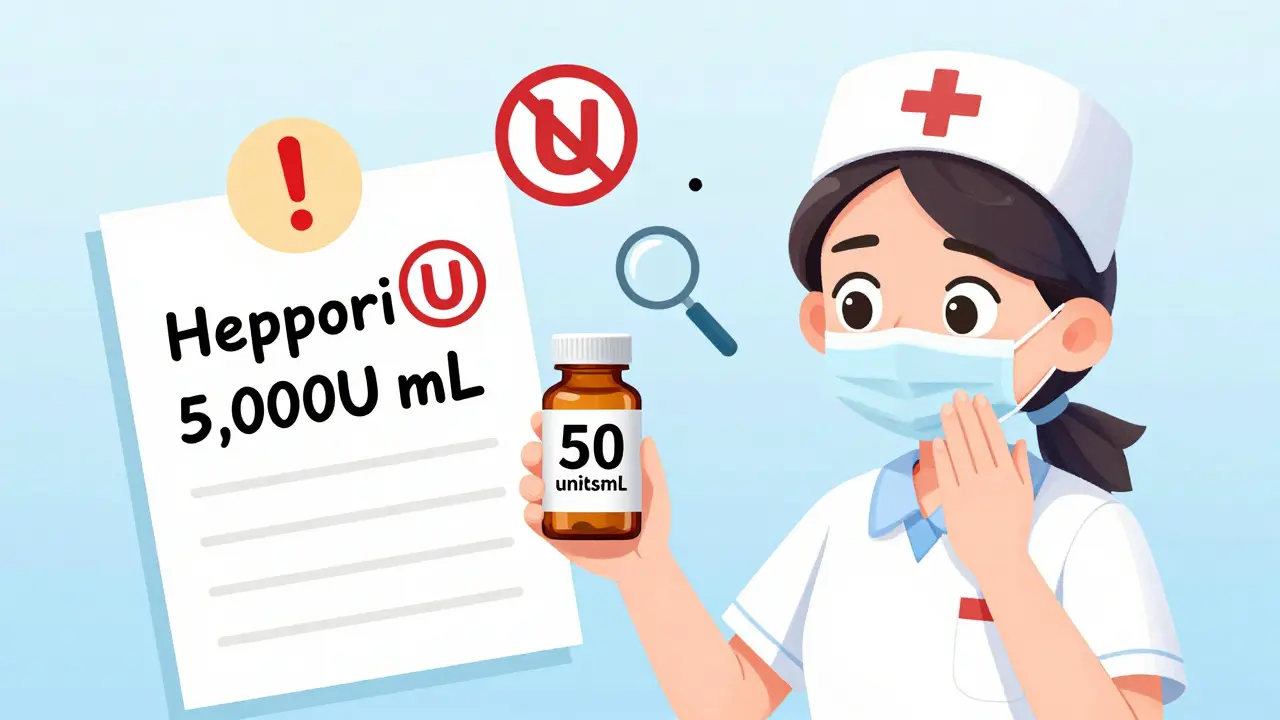
Medication errors aren’t rare. The Institute of Medicine found that at least 1.5 million preventable adverse drug events happen in the U.S. each year. That’s more than car accidents. And according to the Agency for Healthcare Research and Quality, around 7,000 of those result in death - mostly because someone didn’t verify the basics.Look-alike, sound-alike drugs are the biggest problem. Think of prednisone and prednisolone. They sound the same. They’re both steroids. But one is for inflammation, the other for immune suppression. Mix them up, and you could trigger serious side effects. Or take heparin 5,000 units/mL versus heparin 50 units/mL. One is for blood thinning during surgery. The other is for flushing IV lines. Give the wrong one? You could cause a fatal bleed.
Strength errors are just as common. A 2018 FDA report showed that 34% of all medication errors involved the wrong dose - and over half of those happened because the provider never checked the strength against the original order. A missing decimal point, a misread ‘mcg’ as ‘mg’, or writing ‘U’ for units instead of spelling it out - these tiny mistakes can kill.
The Three Things You Must Verify
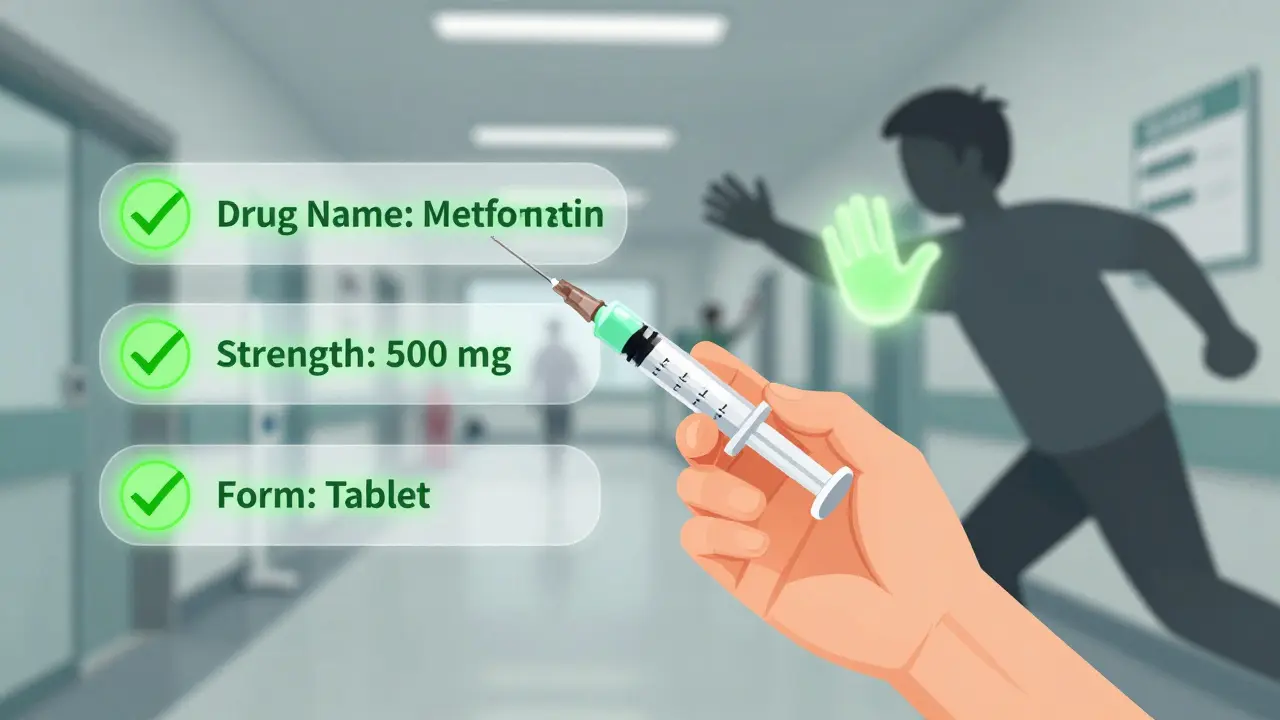
There are only three things you need to check every time you handle a medication - whether you’re a nurse, pharmacist, caregiver, or patient picking up a prescription.- Drug Name - Is it spelled correctly? Is it the full name, or an abbreviation? Never trust ‘MS’ - it could mean morphine sulfate or magnesium sulfate. Use RxNorm standardized names where possible. Avoid abbreviations like ‘QD’ (daily) or ‘BID’ (twice daily). Write it out.
- Strength - What’s the amount? Is it 10 mg? 10 mcg? 500 units? Always check the unit. Never assume. If it’s a liquid, is it mg/mL? If it’s a tablet, is it mg per tablet? The FDA requires strength to be written as a number, a space, then the unit - so 10 mg, not 10mg. That space prevents misreads.
- Dosage Form - Is it a tablet, capsule, liquid, patch, inhaler, or injection? This matters. A pill meant to be swallowed won’t work if crushed and given through a feeding tube. A topical cream isn’t safe for the eyes. A liquid meant for oral use can be deadly if injected.
These three elements must appear together on every prescription, label, and electronic order. If one is missing - stop. Ask. Don’t guess.
How to Spot Common Mistakes
Here’s what to watch for - the red flags that signal trouble:- ‘U’ for units - Always write ‘unit’. ‘U’ looks like a ‘0’ or a ‘4’. A nurse once gave 10,000 units of insulin thinking it was 1,000 - because the ‘U’ looked like a ‘0’. Result: a near-fatal hypoglycemic episode.
- No leading zero - Never write ‘.5 mg’. Always write ‘0.5 mg’. A missing zero can make someone think it’s 5 mg - ten times the dose.
- Trailing zeros - Never write ‘10.0 mg’. That can be misread as 100 mg. Write ‘10 mg’ instead.
- Look-alike names - Use Tall Man lettering: predniSONE vs. predniSOLONE. This small capitalization trick reduces confusion by 76%.
- Missing dosage form - If the order says ‘hydrocodone’ but doesn’t say ‘5 mg tablet’ or ‘5 mg/5 mL oral solution’, it’s incomplete. Don’t fill it.
These aren’t just best practices. They’re rules backed by data. The Institute for Safe Medication Practices found that simply adding a space between the number and unit - like ‘10 mg’ - cuts errors by 12%. That’s one simple change saving lives.

Three Critical Points to Verify
You don’t check once. You check three times.- When you receive the order - Whether it’s from a doctor, an e-prescription, or a family member, verify the name, strength, and form before you even touch the medication. If it’s handwritten, ask for clarification. If it’s electronic, cross-check it with the patient’s history.
- When you prepare the medication - Pull the bottle or blister pack. Read the label. Compare it to the order. Is the strength the same? Is the form correct? If it’s a liquid, check the concentration. If it’s a tablet, count them. Don’t rely on memory.
- Right before you give it - This is your last line of defense. Confirm the patient’s name. Check the medication again. Say it out loud: ‘This is metformin 500 mg tablet, for John Smith, to be taken by mouth twice daily.’ If you’re a patient, do the same. Ask the pharmacist: ‘Is this the same as last time?’
The ‘read-back’ method - saying the medication details out loud before giving it - is used in 89% of successful error-prevention stories reported by nurses. It’s not just a formality. It’s a safety net.
What Happens When You Skip the Check
A Reddit thread from November 2023 collected 147 medication error stories from pharmacists and nurses. The top three were:- Insulin strength mix-ups - 37% of cases. Confusing U-100 with U-500. One patient received 10 times the dose. Died.
- ‘U’ misread as ‘0’ - 29% of cases. A nurse gave 10,000 units of heparin thinking it was 1,000. Patient bled internally.
- Wrong dosage form - 18% of cases. A liquid meant for the mouth was given through a feeding tube. Patient suffered chemical burns to the stomach.
These weren’t mistakes made by bad people. They were mistakes made by tired, rushed, overwhelmed staff - or patients who didn’t know how to ask the right questions.
One nurse in New Zealand told me how she stopped a 100-fold overdose. She saw ‘Heparin 5,000 units/mL’ on the screen. But the vial in her hand said ‘Heparin 50 units/mL’. She paused. She checked. She called the pharmacy. The order had been entered wrong. The patient was saved.
Technology Helps - But Doesn’t Replace You
Electronic health records, barcode scanners, and AI-powered labeling systems have cut errors by up to 83% in hospitals that use them. Epic and Cerner systems flag look-alike names. Barcode systems make sure the right drug goes to the right patient.But here’s the catch: when systems say ‘approved’, people stop thinking. That’s called ‘automation bias’. A 2020 study by The Joint Commission found that 18% of errors happened because clinicians ignored clear warnings because the computer said it was fine.
Technology is a tool. Not a substitute. You still have to look. You still have to think. You still have to ask.
What You Can Do - Right Now
Whether you’re a healthcare worker or someone managing medication for a loved one, here’s your action plan:- Always write out full names - No abbreviations. Not even ‘Lantus’. Say ‘insulin glargine’.
- Use spaces - 10 mg, not 10mg. 0.5 mL, not .5 mL.
- Check the label twice - Once when you pick it up. Once before you give it.
- Ask questions - ‘Is this the same as last time?’ ‘Why is this strength different?’ ‘What’s this for?’
- Use Tall Man lettering - If you’re writing, capitalize the different parts: doPAmine vs. doBUTamine.
- Never assume - Even if it looks familiar, check it.
There’s no magic system that will catch every error. But there’s one habit that will: pause. Check. Confirm.
Final Thought: Safety Is a Habit, Not a Checklist
Medication safety isn’t about having the best software or the most trained staff. It’s about the person holding the bottle, reading the label, and asking: ‘Is this right?’That pause - that moment of doubt - is what saves lives. You don’t need a degree to do it. You just need to care enough to check.
Next time you pick up a prescription - or hand someone their meds - don’t rush. Look at the name. Look at the number. Look at the form. Say it out loud. Then give it.
What should I do if a medication label doesn’t include the strength or dosage form?
Never use it. Contact the prescribing provider or pharmacist immediately. A complete medication order must include the drug name, strength with units, dosage form, route, and frequency. If any of these are missing, the order is incomplete and unsafe to fill or administer. The American Society of Health-System Pharmacists (ASHP) requires all three elements to be present before dispensing or giving any medication.
Why is spacing between the number and unit so important?
Spacing prevents misreading. For example, ‘10mg’ can be mistaken for ‘100 mg’ or ‘10 mgs’ (milligrams vs. milliliters). The Institute for Safe Medication Practices found that simply adding a space - writing ‘10 mg’ - reduces errors by 12%. This small change helps avoid deadly mistakes, especially with high-alert drugs like insulin or heparin.
Can I trust the pharmacy label if it looks different from my last prescription?
Not without checking. Medications can change due to manufacturer switches, generic substitutions, or dosage adjustments. Always compare the name, strength, and form on the new label to your prescription or previous bottle. If anything looks off - even if it’s just a different color or shape - ask the pharmacist. It’s better to be safe than sorry.
What’s the most dangerous abbreviation to avoid?
The most dangerous abbreviation is ‘U’ for units. It looks like a zero or a ‘4’, leading to 10-fold dosing errors. Other dangerous ones include ‘mcg’ written as ‘μg’ (microgram), ‘QD’ for daily (can be read as ‘QID’), and ‘MS’ (which can mean morphine sulfate or magnesium sulfate). Always spell out ‘unit’, ‘microgram’, ‘daily’, and the full drug name.
How can I protect my loved ones from medication errors at home?
Keep all medications in their original bottles. Never transfer pills to pill organizers without verifying the name, strength, and form each time. Use a medication list with all drugs, doses, and purposes - and update it every time something changes. Ask the pharmacist to explain each new medication. Read the label aloud before giving it. And if you’re unsure - call the doctor or pharmacist. There’s no such thing as a dumb question when it comes to safety.







13 Comments
They're hiding the real cause. Big Pharma wants you to check labels so you don't notice the same drugs keep changing names every few months. They're testing how fast you'll swallow anything as long as it looks familiar. I've seen the same pill with 3 different labels in 3 weeks. Don't trust the system.
I used to be a nurse. I saw too many people die because they didn't pause. Not because they were stupid. Because they were exhausted. This post? It's not advice. It's a funeral dirge written in legalese.
Hey everyone - this is gold. Seriously. Whether you're a nurse, a caregiver, or just someone helping your grandma with her pills - this is the stuff that saves lives. I printed this out and taped it to my fridge. Every time I hand someone a pill, I say it out loud. It feels weird at first... but now I can't imagine not doing it. You're not being paranoid. You're being smart.
I'm sorry, but this entire post is dangerously incomplete. Where is the reference to the 2021 FDA MedWatch Report on look-alike/sound-alike (LASA) drug errors? Where are the citations for the 76% reduction claim with Tall Man lettering? And why is there no mention of the 2022 ISMP guidelines on electronic prescribing? Without these, this is just anecdotal fear-mongering with bold fonts.
Ugh. I just had to explain to my aunt why her 'blue pill' was now 'green' and why it's called 'metformin' not 'diabetes medicine'. 🤦♀️ I printed this out for her. She cried. Then she hugged me. This is the real MVP. 🙌❤️
They don't want you to know this. The FDA and hospitals are complicit. They profit from errors. More prescriptions = more money. They encourage abbreviations so you can't tell the difference between insulin and heparin. That's why they changed the font on labels - to confuse you. Read the fine print. They're lying.
The data here is superficial at best. You cite the IOM 1.5M adverse events figure, but that's from 2000. The actual 2023 CDC report shows a 42% decline in preventable errors since 2015 due to EHR adoption. Your 'three checks' are redundant if the CPOE system has built-in alerts. You're glorifying manual verification in a digital age - which, ironically, increases cognitive load and introduces human error.
This is why America is falling apart. No one takes responsibility anymore. You want safety? Stop letting some foreign pharmacy fill your prescriptions. Stop letting nurses who can't even spell 'morphine' handle your meds. We used to have standards. Now we have apps and emojis. Pathetic.
I appreciate the intent behind this. Truly. But I wonder - how many of these errors occur because the patient never received proper counseling? The label isn't the problem. The communication gap is. Maybe we should be talking less about spacing and more about patient education programs.
This is one of the clearest, most practical guides I've read on medication safety. I work in a clinic and I've started sharing this with every new patient. The 'say it out loud' trick? Game changer. Simple. Human. Effective. Thank you for writing this.
You think this is bad? In India, we don't even have labels. Pills come in plastic bags with scribbles. My mom once took a steroid thinking it was a vitamin. She ended up in the hospital. No one checked. No one cared. So yes - check everything. Always. Because if you don't, no one else will.
The institutionalization of the three-verification protocol, as articulated herein, constitutes a paradigmatic shift in pharmacovigilance practice. It aligns with the principles of human factors engineering and mitigates cognitive load through procedural redundancy. One would be remiss to overlook its alignment with ISO 14971 risk management standards.
You people are so naive. This isn't about spacing or spelling. It's about control. The system wants you to be afraid. So you'll take more pills. So you'll trust the label more than your gut. So you'll never question why your blood pressure med changed from blue to yellow. It's all a scam.