Every year, thousands of people on blood thinners end up in the emergency room-not because of a stroke or clot, but because they took something they thought was harmless: a herbal supplement. Turmeric. Garlic. Ginkgo. Green tea. These aren’t drugs. They’re sold as natural, safe, even healthy. But when you’re on warfarin, apixaban, or rivaroxaban, herbal supplements can turn from harmless to deadly in days.
Why This Isn’t Just a "Natural vs. Medicine" Debate
People assume that if something is plant-based, it can’t interfere with prescription meds. That’s dangerous thinking. Herbs don’t work like vitamins. They’re complex chemical mixtures. Some inhibit liver enzymes that break down your blood thinner. Others directly affect platelets or clotting factors. The result? Your INR spikes. Or it crashes. Either way, you’re at risk.Take danshen (Salvia miltiorrhiza), a common herb in traditional Chinese medicine. In 12 documented cases across five countries between 2018 and 2023, patients on warfarin saw their INR jump 300-400% within 72 hours of starting danshen. That’s not a fluke. That’s a life-threatening bleed waiting to happen. One man in New Zealand, 72, was admitted with a brain hemorrhage after adding danshen tea to his daily routine. He didn’t tell his doctor. He thought it was "just for circulation."
The Top 10 Dangerous Herbs for Blood Thinners
Based on over 14,000 adverse event reports analyzed by the FDA in 2024, these are the herbs that cause the most serious problems when mixed with anticoagulants:- Ginkgo biloba - Blocks platelet function. Increases bleeding risk by 2.5x when combined with warfarin.
- Garlic - Thins blood directly. 214 major bleeding cases linked in 2023 alone.
- Ginger - Inhibits thromboxane. Safe under 1g/day with monitoring-but most people don’t measure it.
- Ginseng - Can either increase or decrease INR unpredictably. No safe dose established.
- St. John’s Wort - Speeds up metabolism of apixaban and rivaroxaban. Can drop drug levels by 50% in 3 days.
- Chamomile - Contains coumarin, the same compound found in warfarin. Doubles bleeding risk.
- Cranberry - Inhibits CYP2C9. Linked to INR spikes even with small juice amounts.
- Green tea - High in vitamin K and catechins. Inconsistent intake = unstable INR.
- Chinese wolfberry (goji berry) - Interferes with CYP enzymes. Over 80 cases reported since 2020.
- Dong quai - Contains anticoagulant compounds. Banned in some countries for this reason.
These aren’t rare outliers. Together, they account for 68% of all severe interaction cases. And here’s the kicker: most people don’t even know they’re taking them. They’re in teas, capsules, smoothies, and "immune boosters" sold at health food stores.
Warfarin vs. Newer Blood Thinners: Not All Are Equal
Many assume the newer anticoagulants-apixaban, dabigatran, rivaroxaban-are "safer" with herbs. That’s partly true. They don’t rely on CYP2C9 like warfarin does. But they’re not immune.St. John’s Wort is the biggest threat to these drugs. It activates an enzyme called P-glycoprotein that flushes them out of your system. A 2021 study showed apixaban levels dropped by half within 72 hours of taking St. John’s Wort. That’s like stopping your pill entirely. One patient in Florida had a stroke after starting St. John’s Wort for depression. His doctor didn’t ask about supplements.
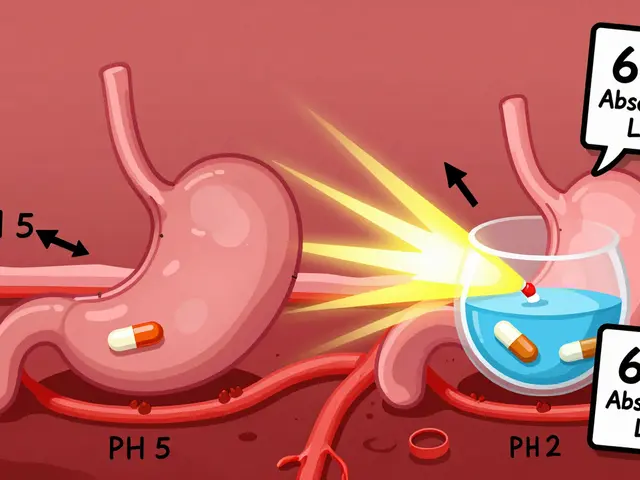
Warfarin is more predictable in how it reacts-but also more dangerous because of its narrow window. Your target INR is 2.0-3.0. Go above 4.0? Risk of bleeding skyrockets. Drop below 1.5? Clots form. Herbal supplements make that balance impossible to maintain without daily monitoring.

The Silent Problem: Patients Don’t Tell Doctors
In a 2024 Medscape survey of 1,247 people on blood thinners, nearly 70% admitted they used herbal supplements without telling their doctor. Why? 43% said they believed "natural means safe." Another 28% said their doctor never asked.Here’s the reality: doctors ask about pills. They ask about alcohol. They ask about smoking. But how often do they ask, "Are you drinking any herbal teas? Taking any supplements?"
A 2022 study found only 27% of medical records even documented herbal supplement use-even when patients mentioned it. That’s not negligence. It’s systemic. Training doesn’t emphasize it. Time is short. And patients assume it’s not important.
But it is. One Reddit user, u/WarfarinWarrior, posted about his INR hitting 4.2 after adding turmeric to his morning smoothie. He was hospitalized. His doctor said, "I didn’t think you’d be taking that." That’s not a joke. That’s a warning.
What About Vitamin K? Isn’t That the Real Issue?
Yes, vitamin K affects warfarin. Spinach, kale, broccoli-these foods are rich in it. But here’s what most people miss: consistent intake of vitamin K-rich foods doesn’t cause dangerous swings. It’s inconsistent intake that does. Eat spinach every day? Your INR stabilizes. Eat it one day, skip it for a week, then eat three cups? That’s when your INR goes wild.Herbal supplements are worse because they’re unpredictable. One batch of ginkgo may have high levels of active compounds. The next batch may be diluted. There’s no regulation. The FDA doesn’t require pre-market testing for supplements. In 2023, 34.7% of herbal products tested contained unlisted ingredients-including other drugs.
One man in California was taking "natural blood thinner capsules" labeled as "hawthorn and bilberry." Lab tests found they also contained warfarin. He didn’t know. He was doubling his dose.

What Should You Do?
If you’re on a blood thinner, here’s what you need to do-right now:- Make a full list of everything you take: pills, powders, teas, tinctures, drops. Include doses and frequency.
- Bring it to every appointment-even if you think it’s "not important."
- Ask your doctor or pharmacist: "Which of these are dangerous with my blood thinner?" Don’t assume they know. Many don’t.
- Use a trusted resource like the Natural Medicines Database. It rates interactions on a 1-7 scale. Level 7 = life-threatening. Anything above Level 4? Stop it.
- Don’t start anything new without checking. Even "safe" herbs like ginger can be risky if you’re on high-dose warfarin.
There’s no such thing as a "safe" herbal supplement for someone on anticoagulants. Only "managed" and "unmanaged."
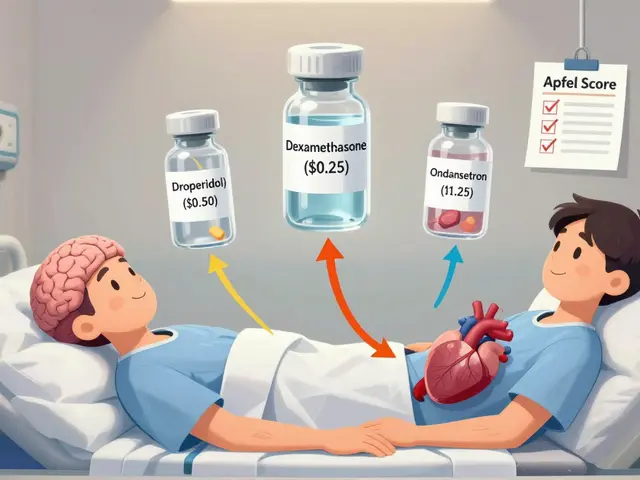
What’s Changing? Better Tools Are Coming
In 2025, the FDA required all new anticoagulant prescriptions to include a standardized herbal interaction checklist. That’s huge. It forces doctors to ask.Europe rolled out MedCheck AI in 2024-a tool that scans your meds and supplements and flags dangerous combos with 92.4% accuracy. It’s being used in hospitals now. But it’s not available to the public.
Genetic testing is also helping. The International Warfarin Pharmacogenetics Consortium found that testing for CYP2C9 and VKORC1 genes reduces major bleeding events by 31% in patients who use herbs. If you’re on warfarin long-term, ask if genetic testing is an option.
And CBD oil? New data from 2024 shows it increases INR by 2.8 times in 68% of warfarin users. It’s not just a trend. It’s a growing danger.
The Bottom Line
You’re not being paranoid if you’re worried about herbs and blood thinners. You’re being smart. The data doesn’t lie: thousands of avoidable hospitalizations happen every year because people didn’t connect the dots between their turmeric capsule and their INR spike.There’s no benefit to taking herbal supplements while on anticoagulants that outweighs the risk. Not for heart health. Not for inflammation. Not for sleep. The risks are real, documented, and deadly. The safest choice isn’t finding the "right" herb. It’s avoiding them altogether.
If you’re thinking of starting something new-stop. Talk to your doctor first. Bring your bottle. Show them the label. Ask: "Could this kill me?" If they hesitate? Get a second opinion.
Your blood doesn’t care if it’s natural. It only cares if it’s dangerous.






14 Comments
Herbs aren't magic. They're chemistry. If you're on warfarin and think turmeric is harmless you're either naive or dumb. No one cares if it's 'natural' - your liver doesn't care about marketing labels. Stop pretending plants are safe because they grow in dirt.
St. John’s Wort and apixaban? That’s not a interaction. That’s a suicide pact wrapped in a wellness trend.
I grew up in India with my grandma using turmeric for everything. But I never mixed it with blood thinners. Maybe we were just smarter? Or maybe we didn’t have 20 different supplements on every shelf. Respect the medicine, respect the herb - don’t mash them together like a smoothie.
Let’s be real - this isn’t about herbs. It’s about the FDA and Big Pharma wanting control. They don’t want you to know that garlic and ginger have been used for centuries. Now they’re scared because people are waking up. They’re labeling natural things as dangerous so you’ll keep buying pills with side effects no one talks about. And don’t get me started on how vitamin K is being manipulated to make warfarin seem more necessary than it is. The whole system is rigged. You think they test every supplement? No. They test the ones that compete. The rest? Just let them sell it until someone dies - then they panic and slap a warning on it. It’s all profit. Always has been.
The data presented here is statistically significant and clinically actionable. The documented cases of INR elevation in conjunction with danshen, ginkgo, and St. John’s Wort are not anecdotal but peer-reviewed and replicated across multiple jurisdictions. The absence of regulatory oversight for dietary supplements constitutes a public health vulnerability. I urge all clinicians to implement standardized screening protocols.
So the FDA says herbs are dangerous but lets companies sell CBD oil with no labeling? Funny how the same people who warn you about ginkgo are okay with pharmaceuticals that cause internal bleeding 10x more often. Who’s really in charge here? Who profits? And why does every warning come after someone dies?
Think about it - they told us smoking was safe. They told us aspartame was fine. They told us vaccines had no long-term effects. Now they’re telling us herbs are deadly. Who are they protecting? The pharmaceutical industry? The hospital system? The insurance companies? You think your doctor really cares? Or do they just want you to come back every month for another blood test so they can keep billing? This isn’t medicine. It’s a cage. And the herbs? They’re the keys. They’re trying to lock you in. Don’t let them.
You people are so obsessed with Western medicine you forget Africa and Asia have been managing anticoagulation with herbs for centuries. We use neem, moringa, bitter leaf - and we monitor with traditional indicators. Pulse. Skin color. Urine clarity. No INR machine needed. You treat herbs like they’re bombs because you don’t understand them. Maybe the problem isn’t the herbs. Maybe it’s your arrogance.
I’ve been on rivaroxaban for 4 years. Took ginger tea for months without issue. Then my INR spiked after switching brands. Turned out the new one had 3x the active compounds. Never again. I only buy from labs that publish batch testing. It’s not about avoiding herbs. It’s about knowing exactly what’s in them.
Y’all need to chill. I’m on apixaban and I drink green tea every morning. So does my mom. So does my brother. We all get our INR checked. If you’re doing the basics - monitoring, talking to your doc, reading labels - you’re fine. Don’t let fear-mongering make you paranoid. Just be smart. Not scared.
My grandfather in Afghanistan used hawthorn for his heart. He lived to 94. Never took a pill. But he also never mixed it with anything. He understood balance. We lost that. Now we want quick fixes - a capsule for everything. The real danger isn’t the herb. It’s our disconnect from context. Nature doesn’t work in isolates. We do. That’s the problem.
The emotional weight of this issue cannot be overstated. Patients are not merely noncompliant - they are systematically failed by a healthcare system that fails to ask, fails to educate, and fails to listen. This is not a pharmacological anomaly. It is a failure of care.
It is imperative that all patients on anticoagulant therapy be provided with a written, evidence-based guide regarding herbal supplement interactions. This should be distributed at the time of prescription and reviewed at each follow-up visit. Standardization of communication is not optional - it is ethically required.
Wait so you’re telling me I can’t have my turmeric latte anymore?? Like the one I make with coconut milk and cinnamon?? But it’s so cozy?? I just wanted to feel good?? 😭