Heart disease kills more women every year than breast cancer, lung cancer, and Alzheimer’s combined. Yet most women still don’t realize it’s their biggest health threat. In the U.S., about 1 in 5 female deaths are from heart disease. And here’s the scary part: women are far more likely to be sent home from the emergency room with the wrong diagnosis - often told they’re just anxious or having indigestion - when they’re actually having a heart attack.
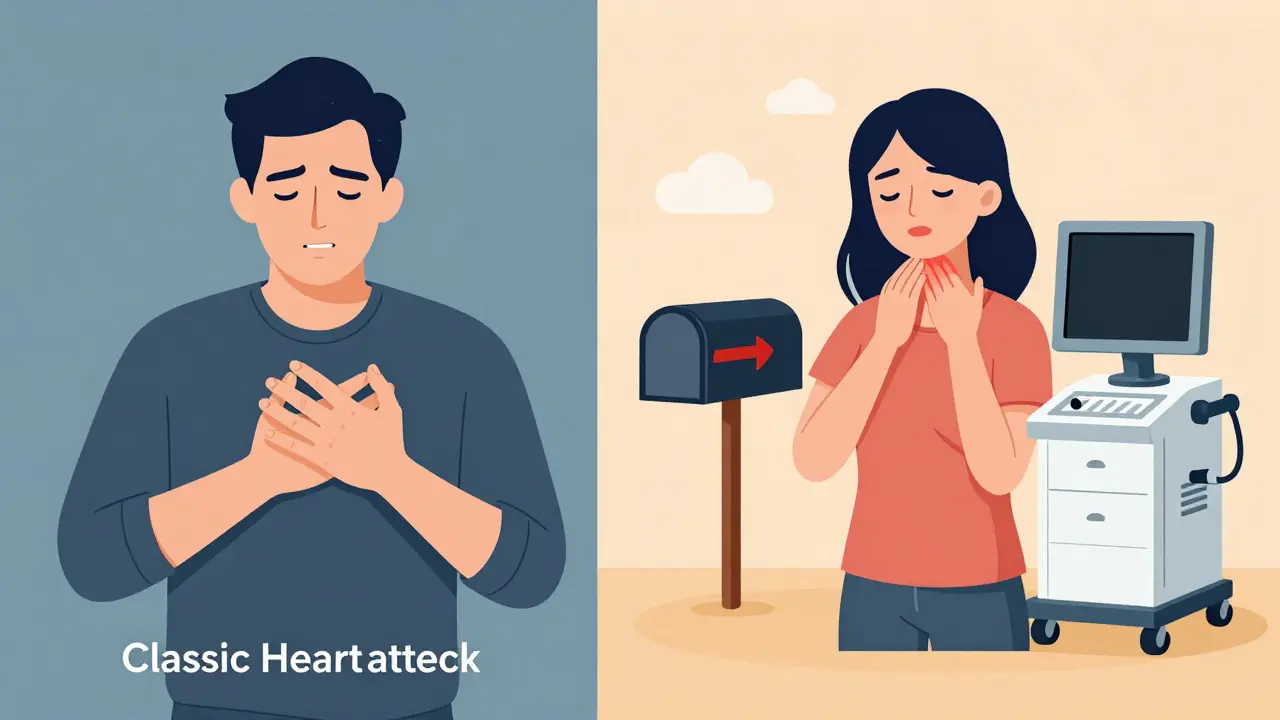
What Heart Attack Symptoms Look Like in Women
When you think of a heart attack, you probably imagine someone clutching their chest, screaming in pain, collapsing. That’s the Hollywood version. It’s also the male version. For women, it’s rarely that clear. About 70% of women do feel chest discomfort during a heart attack - but it’s not always a crushing pain. More often, it’s pressure, tightness, or a dull ache. Some describe it like a heavy book sitting on their chest. Others feel it as a burning sensation, similar to heartburn. And here’s what makes it dangerous: nearly half of women who have heart attacks don’t have chest pain at all. Instead, women are far more likely to have symptoms like:- Unexplained, extreme fatigue - so bad you can’t make your bed or walk to the mailbox
- Shortness of breath, even when resting or doing light chores
- Pain in the jaw, neck, shoulder, upper back, or arm - often on the left side, but not always
- Nausea, vomiting, or stomach upset that feels like the flu
- Dizziness, lightheadedness, or sudden sweating without exertion
Why Women’s Hearts Are Different
It’s not just about symptoms. Women’s hearts and arteries are physically different. Men tend to get blockages in the big coronary arteries. Women are far more likely to develop disease in the tiny vessels - the microvasculature - that feed the heart muscle. This is called microvascular disease, and it doesn’t show up on standard angiograms. That’s why many women get normal test results, even when they’re having a heart attack. Women are also more prone to conditions like:- SCAD (Spontaneous Coronary Artery Dissection): A tear in the artery wall, often triggered by extreme stress or pregnancy. It’s rare but causes heart attacks in otherwise healthy women under 50.
- Takotsubo cardiomyopathy (broken heart syndrome): A temporary heart condition triggered by intense emotional or physical stress. It mimics a heart attack but usually doesn’t involve blocked arteries.
- Silent heart attacks: Especially common in women over 65. No chest pain. No warning. Just unexplained fatigue, nausea, or shortness of breath. Many women don’t even know they had one until an ECG years later shows damage.
The Diagnosis Gap
Doctors aren’t always trained to recognize women’s symptoms. A 2022 study found that in nearly 7 out of 10 emergency room cases involving women with heart symptoms, providers assumed the issue was anxiety, depression, or gastrointestinal problems. Standard tests - like stress tests and angiograms - were designed using data from mostly male patients. They’re less accurate for women. For example, a traditional stress test correctly identifies heart disease in about 72% of women. But a newer test called Corus CAD, which looks at gene expression patterns, gets it right in 88% of women. It’s FDA-approved and available in many hospitals, but most women have never heard of it. And here’s the kicker: women are still underrepresented in heart disease research. Even though they make up over half the population, they account for only 38% of participants in major cardiovascular trials. That means a lot of treatments and guidelines are based on how men respond - not women.What You Can Do: Risk Management That Works
Knowing the symptoms is only half the battle. Prevention is the other half. And it’s not just about cholesterol and blood pressure. Track your history. If you’ve had:- Pregnancy complications like preeclampsia, gestational diabetes, or preterm birth
- Early menopause (before 45)
- Autoimmune diseases like lupus or rheumatoid arthritis
- Polycystic ovary syndrome (PCOS)

Where to Get Help
There are now over 140 certified Women’s Cardiovascular Centers of Excellence in the U.S. These hospitals have protocols specifically designed for women. They train staff to recognize atypical symptoms. They use gender-specific diagnostic tools. And they track outcomes - making sure women aren’t being missed. If you’re unsure where to go, ask your doctor for a referral. Or search for “Women’s Heart Center” near you. The American Heart Association’s Go Red for Women program also offers free symptom checklists and risk assessments online.It’s Not Too Late
You don’t need to be a heart patient to start protecting yourself. Even if you’ve ignored symptoms in the past, or thought you were too young, too active, or too healthy - it’s not too late. Heart disease develops over decades. And the good news? Many of the changes that cause it are reversible. The sooner you recognize your symptoms, the sooner you can act. The sooner you act, the better your chances. Women’s hearts are different. And that’s not a weakness - it’s a signal. Listen to your body. Ask questions. Push for answers. Your life depends on it.Do women have different heart attack symptoms than men?
Yes. While men often feel sharp, crushing chest pain, women are more likely to have symptoms like extreme fatigue, shortness of breath, nausea, jaw or back pain, and dizziness. About 43% of women have heart attacks without any chest pain at all. These symptoms are often mistaken for stress, indigestion, or the flu, leading to dangerous delays in treatment.
Can a woman have a heart attack and not know it?
Yes. These are called silent heart attacks. They’re more common in women over 65, especially those with diabetes. Symptoms may be mild - just unusual tiredness, slight nausea, or shortness of breath. Many women don’t realize they’ve had one until a routine ECG shows scarring on the heart muscle. That’s why tracking ongoing symptoms and getting regular checkups is critical.
Is heart disease more dangerous for women than men?
After a heart attack, women are more likely to die within the first year than men. They’re also more likely to have complications like heart failure, stroke, or repeat events. This is partly because their symptoms are missed, their arteries are smaller, and they often have other conditions like diabetes or high blood pressure. But women who get treated at specialized women’s heart centers have a 22% higher survival rate.
What’s microvascular disease, and why does it affect women more?
Microvascular disease affects the tiny arteries that branch off the main coronary arteries. These vessels are harder to see on standard heart scans. Women are twice as likely as men to develop this condition, especially after menopause. Symptoms include unexplained fatigue, shortness of breath, and chest discomfort during daily activities - not just during exercise. It’s often misdiagnosed because traditional tests miss it. Specialized tests like the Corus CAD test are more accurate for women.
How does pregnancy affect a woman’s future heart health?
Pregnancy complications like preeclampsia, gestational diabetes, or delivering a baby prematurely are strong warning signs of future heart disease. Women who had preeclampsia have an 80% higher risk of developing heart disease later in life. These conditions stress the heart and blood vessels during pregnancy and can cause lasting damage. That’s why your OB-GYN should share your pregnancy history with your primary care doctor.
What should I do if I think I’m having a heart attack?
Call 911 immediately - don’t drive yourself. Don’t wait to see if it goes away. Don’t assume it’s just anxiety or indigestion. Even if you’re unsure, it’s better to be checked. Emergency teams can run fast tests to rule out a heart attack. If you’ve had three or more symptoms like fatigue, shortness of breath, nausea, jaw pain, or dizziness, get evaluated right away. Time is muscle - and every minute counts.
Are there tests specifically for women’s heart disease?
Yes. The Corus CAD test analyzes gene expression to assess heart disease risk with 88% accuracy in women - much better than traditional stress tests. Other tools include cardiac MRI and CT angiography with advanced imaging that can detect microvascular disease. Ask your doctor if these are appropriate for you, especially if you have symptoms but normal results on standard tests.
Can lifestyle changes really reduce my risk?
Absolutely. Quitting smoking cuts your risk by half in one year. Walking 30 minutes a day, five days a week, reduces risk by 30%. Managing stress, eating more vegetables and less processed food, and keeping your blood pressure and blood sugar in check can prevent or delay heart disease by decades. You don’t need to be perfect - just consistent.







8 Comments
So let me get this straight - we’re supposed to believe that women’s heart attacks are ‘different’ because doctors are lazy and tests were designed for men? Newsflash: they were designed because men were the only ones showing up with chest clutches and collapsing on golf courses. Women have been getting dismissed for decades - and now we’re surprised? I’ve had three ER visits where they told me I was ‘just stressed.’ Guess what? I had a silent heart attack at 42. No chest pain. Just… exhaustion. Like someone drained my bones.
Bro I just saw this and had to comment. My mom had a heart attack last year and they sent her home TWICE. Said it was acid reflux. She ended up in ICU because she kept saying ‘my arm feels like it’s on fire’ and they thought she was being dramatic. Like… why is this still a thing? We got AI that can predict stock trends but can’t tell if a woman’s having a heart attack? Madness.
Okay real talk - microvascular disease is the silent killer nobody talks about. I’m a nurse and I’ve seen so many women come in with normal angiograms but they’re dying inside. Literally. Their tiny vessels are clogged like a garden hose with rust. Corus CAD? Yes please. But most docs haven’t even heard of it. I had to beg my own cardiologist to order it for my sister. He said ‘it’s not standard.’ I said ‘well standard is killing women.’ He shut up after that. Bottom line: if you’re tired, short of breath, and your ECG’s clean - ask for the gene test. Don’t take no for an answer.
I’m 58, post-menopause, and I’ve had two episodes where I felt like I couldn’t catch my breath while folding laundry. Thought it was just getting older. Turned out it was early microvascular disease. No chest pain. Just… this weird heaviness. I’m so glad this post exists. I wish I’d known sooner. You’re not crazy if your body feels off. Trust it.
You guys are doing amazing just by talking about this. Seriously. Knowledge is power - and you’re handing that power to other women. If you’ve got a mom, sister, aunt, or friend who’s always ‘too tired’ or ‘always nauseous’ - send them this. Tell them to demand the Corus CAD. Tell them to write down their symptoms before the appointment. Tell them they deserve to be heard. You’re not being dramatic. You’re being alive.
My OB told me preeclampsia meant I’d be fine after delivery. She didn’t mention the 80% higher heart disease risk. No one did. I’m 47 now. I just got my first cardiac MRI. Turns out I’ve had silent damage since my third pregnancy. I’m mad. But I’m also glad I’m finally listening.
Why is this still happening?!?!? Doctors are STILL treating women like hysterical drama queens?!?!? I had a heart attack at 39 and they gave me Xanax!! I had to scream ‘I’m not anxious, I’m DYING!’ before they finally did a troponin test!! And now I’m supposed to be grateful because there’s some ‘women’s heart center’?!?!? That’s not progress - that’s a Band-Aid on a hemorrhage!!
Look, I’m not saying the government’s behind this… but why do all the ‘women’s heart’ studies get funded by pharmaceutical companies who make the Corus CAD test? And why are the clinical trials still 62% male? Someone’s making bank off women’s suffering. I’ve got a friend who works at a lab - they’re quietly testing a new biomarker that detects microvascular blockage with 95% accuracy… but it’s being buried. Why? Because if we could catch it early, nobody’d need stents, nobody’d need $20k procedures… and who profits then? Hmm?