Stopping benzodiazepines suddenly can cause dangerous withdrawal symptoms like seizures or psychosis. But with a careful benzodiazepine tapering a systematic, gradual reduction of benzodiazepine dosage to minimize withdrawal symptoms, you can safely reduce dependence. This guide explains proven strategies based on the latest clinical guidelines from 2024.
Why tapering is necessary
Abruptly stopping benzodiazepines after long-term use carries serious risks. Research shows 20-40% of people experience severe withdrawal symptoms, including seizures, psychosis, or life-threatening complications. The FDA required label changes in 2019 after reports of harm from sudden discontinuation. For example, someone using alprazolam (Xanax) daily for 3 months could have seizures within 24 hours of stopping. This is why medical professionals emphasize gradual reduction over abrupt cessation.
How benzodiazepine tapering works
Standard tapering involves reducing your dose by 5-10% every 2-4 weeks. This slow approach minimizes withdrawal symptoms while avoiding rebound anxiety or insomnia. The Joint Clinical Practice Guideline (2024) confirms this method is effective for most patients. Doctors monitor symptoms after each reduction to adjust the pace. For instance, if tremors or panic attacks appear, the next reduction might be delayed or made smaller. Consistency is key-skipping doses or varying the schedule can trigger withdrawal.
Personalized tapering schedules
| Duration of Use | Recommended Taper Duration |
|---|---|
| 2-8 weeks | At least 2 weeks |
| 8 weeks to 6 months | At least 4 weeks |
| 6 months to 1 year | At least 8 weeks |
| Over 1 year | 6-18 months |
This table shows how taper length depends on how long you’ve taken benzodiazepines. The Oregon Health Authority (2022) developed these timelines based on clinical evidence. For example, someone using benzodiazepines for 2 years would need at least 6 months to taper safely. Rushing this process increases relapse risk and worsens symptoms.

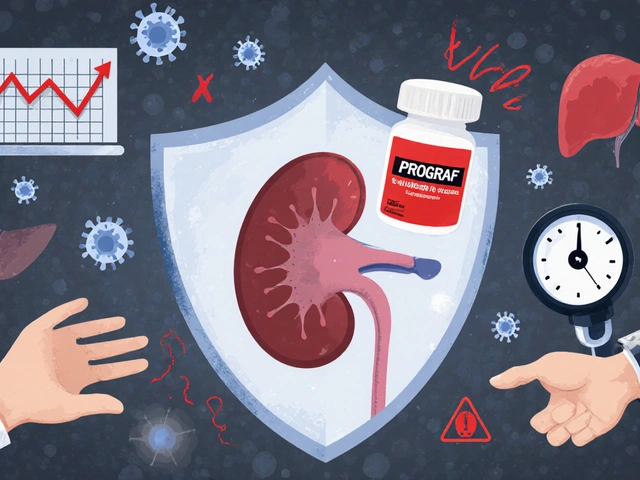
Choosing the right medication for tapering
Switching to a longer-acting benzodiazepine like diazepam often makes tapering smoother. Diazepam has a half-life of 20-100 hours, compared to alprazolam’s 6-12 hours. This means fewer withdrawal spikes between doses. Conversion rates are precise: 1mg alprazolam equals 20mg diazepam. For instance, if you take 1mg Xanax daily, you’d start with 20mg diazepam before gradually reducing. This approach is recommended by the Joint Guideline for patients on short-acting benzos.
Support during the tapering process
Professional support dramatically improves success rates. Cognitive behavioral therapy (CBT) helps patients manage anxiety without medication. A 2024 JAMA Psychiatry study found 68.3% of people successfully discontinued benzodiazepines when CBT was combined with tapering, versus 42.1% with medication alone. The VA also uses team-based care-clinical pharmacists monitor doses, and peer-support providers share lived experience. Regular check-ins with your doctor are essential. They’ll track symptoms and adjust your plan in real-time.

When to seek professional help
Seek immediate help if you experience severe symptoms like seizures, hallucinations, or chest pain during tapering. These indicate dangerous withdrawal. Other red flags include inability to sleep for more than 3 days, extreme panic attacks, or thoughts of self-harm. Never adjust your dose without consulting a doctor. For example, if you feel anxious after a reduction, your provider might slow the taper or add temporary support medications like gabapentin. Remember: tapering is a medical process, not a DIY project.
Common challenges and solutions
Anticipatory anxiety-worrying about withdrawal before it happens-is common. This often worsens symptoms. Techniques like deep breathing or mindfulness can help. Breakthrough insomnia? Your doctor might recommend short-term sleep aids like melatonin, not more benzodiazepines. Some people face rebound anxiety when reducing doses. In these cases, the taper schedule may need to be slower. For example, reducing by 5% every 4 weeks instead of 2. Patience is critical-rushing increases relapse risk.
Can I stop benzodiazepines cold turkey?
No. Abrupt discontinuation after regular use for over a month carries high risks. Studies show 20-40% of people experience severe withdrawal symptoms like seizures or psychosis. The FDA mandates gradual tapering for safety. Always work with a doctor to create a personalized plan.
How long does a benzodiazepine taper take?
It depends on how long you’ve used benzodiazepines. For 2-8 weeks of use, tapering takes at least 2 weeks. For 6 months to 1 year, it’s 8 weeks. Over a year requires 6-18 months. The Joint Guideline (2024) emphasizes that slower tapers reduce symptom severity. Rushing the process can cause relapse or dangerous complications.
Why switch to diazepam for tapering?
Diazepam has a longer half-life (20-100 hours) than short-acting benzos like alprazolam (6-12 hours). This means fewer withdrawal spikes between doses. For example, 1mg alprazolam equals 20mg diazepam. The Joint Guideline recommends this switch for smoother tapering, especially for patients on high-dose or frequent dosing schedules.
Does cognitive behavioral therapy help during tapering?
Yes. A 2024 JAMA Psychiatry study found 68.3% of people successfully discontinued benzodiazepines when CBT was combined with tapering, compared to 42.1% with medication alone. CBT teaches coping skills for anxiety without relying on medication. It’s especially effective for managing anticipatory anxiety and sleep issues during the taper process.
What should I do if withdrawal symptoms get severe?
Contact your doctor immediately. Severe symptoms like seizures, hallucinations, or chest pain require urgent medical attention. Never increase your dose on your own. Your provider may temporarily slow the taper, add short-term medications like gabapentin for symptom relief, or switch to a longer-acting benzodiazepine. Safety always comes first.