Doctors prescribe generic drugs every day - but how many truly believe they work as well as brand-name meds? The answer isn’t as simple as you might think. Despite generics making up 90.1% of all U.S. prescriptions, many physicians still hesitate to recommend them, especially for serious or chronic conditions. This isn’t about cost - it’s about trust. And that trust is built on what doctors believe they know, what they’ve seen, and what they’ve been taught.
Why Do Some Doctors Doubt Generic Drugs?
It’s not that doctors are anti-generic. Most know generics are cheaper. But a surprising number still question whether they’re just as safe and effective. A 2017 study of 134 Greek physicians found that over 27% didn’t believe generic drugs were therapeutically equivalent to brand-name versions. Even more troubling: 25% of doctors across multiple studies thought generics were lower quality.
These beliefs don’t come out of nowhere. Many doctors remember cases where a patient switched from a brand-name drug to a generic - and then reported side effects, lack of effect, or even a flare-up of their condition. One common example? Levothyroxine. For thyroid patients, even tiny changes in hormone levels can cause fatigue, weight gain, or heart palpitations. Some physicians swear they’ve seen patients destabilize after switching to a different generic manufacturer. While the FDA says all approved generics must be within 80-125% of the brand’s bioavailability, doctors who’ve seen bad outcomes don’t always trust the numbers.
Another issue? Manufacturing. Generic drugs are made by dozens of companies - some based overseas. A 2017 survey found that 57.8% of physicians worried about inconsistent quality between different generic makers. That’s not paranoia. There have been FDA warnings about contamination and quality lapses at foreign facilities. When a doctor’s patient gets sick after a switch, it’s easy to blame the generic - even if the real cause is something else.
Who’s Most Skeptical? Age, Experience, and Specialty Matter
Not all doctors feel the same way. Research shows clear patterns. Older physicians, especially those with more than 10 years of experience, are significantly more likely to distrust generics. Male doctors also show stronger skepticism than female ones - a reversal of older assumptions that women were more cautious about cost-cutting meds.
Specialists are more hesitant than primary care doctors. Cardiologists, neurologists, and endocrinologists often treat conditions where small changes in drug levels matter. They’re more likely to stick with brand names for drugs like warfarin, lithium, or levothyroxine. Primary care doctors, who see more routine conditions like high blood pressure or diabetes, are more open to generics - but even they’re not always prescribing them first.
A 2018 study found that only 32.7% of doctors routinely prescribed generics as first-line treatment, even though nearly 50% agreed generics could benefit patients financially. That gap? It’s the gap between knowing something is right and actually doing it.

The Knowledge Gap: Most Doctors Don’t Fully Understand Bioequivalence
Here’s one of the biggest problems: doctors think they know how generics work - but many don’t. An Oxford study found that only 43.7% of primary care physicians correctly understood the FDA’s bioequivalence standards, even though 78.4% claimed to be familiar with them.
Some believe generics need higher doses to work. Others think the inactive ingredients (fillers, dyes, coatings) are more likely to cause reactions. A CDC rural study found patients were told by doctors that generics were “stronger” - which led them to believe they caused more side effects. That’s not just misinformation. It’s a dangerous misunderstanding that gets passed down.
Medical schools aren’t helping much. Only 38.7% of U.S. medical schools include structured education on generic drugs in their curriculum, according to the AAMC. Most doctors learn about generics on the job - from pharmacists, from patients, or from old habits. And if they were never taught how to interpret bioequivalence data, how can they confidently recommend a switch?
Patients Trust Doctors - and That’s Both a Blessing and a Burden
Doctors aren’t just prescribing drugs. They’re shaping beliefs. A systematic review found that 68.4% of patients get their information about generic drugs from their doctor. That means if a doctor says, “I don’t trust this generic,” the patient believes it. And that belief can lead to non-adherence - or worse.
The CDC found that in rural areas, 41.7% of patients stopped taking their medication after being switched to a generic - not because it didn’t work, but because they didn’t trust it. And once that trust is broken, it doesn’t just affect one drug. Patients start doubting all medical advice. That’s the “mistrust cascade” - and it’s one of the biggest hidden costs of provider skepticism.
On the flip side, when doctors explain generics clearly - when they say, “This is the same active ingredient, just made by a different company under the same rules” - patients are far more likely to accept the switch. But few doctors take the time. In one study, 74.3% of primary care physicians said they didn’t have enough time during appointments to discuss drug substitutions.

What’s Changing? Education, Data, and Real-World Evidence
Change is happening - slowly. A 2017 study in Greece gave doctors a 90-minute workshop on bioequivalence and real-world outcomes. Six months later, those doctors increased their generic prescribing by 22.5%. The biggest jump? Among physicians with 5-10 years of experience. Not the veterans. Not the new grads. The ones in the middle - the ones still open to learning.
Real-world data is starting to shift minds. Johns Hopkins ran a pilot where providers got access to post-market data showing how patients did on newly approved generics. Within months, generic prescribing for those drugs rose by 28.6%. That’s not magic. That’s transparency.
Organizations are stepping in. The FDA’s GDUFA III program now requires more post-market monitoring of generics. The American Medical Association pushed for simpler generic names - not chemical jargon like “metformin hydrochloride,” but clearer labels like “Metformin HCl.” That’s a small change, but it matters. When a doctor says, “I’ll give you the generic,” and the patient sees a name they recognize, it reduces fear.
And the ROI? It’s huge. One study found every $1 spent on physician education led to $17.30 in savings from increased generic use. Yet, only 0.7% of total drug marketing dollars go toward educating doctors about generics. Most of that money goes to promoting brand-name drugs.
What Needs to Happen Next?
Here’s what’s working:
- Education in medical school - not as an afterthought, but as core curriculum.
- Peer-led training - doctors who successfully switched to high generic prescribing have 43.2% more influence than outside speakers.
- Real-time data access - giving providers dashboards showing how patients on generics are doing in the real world.
- Clear communication tools - handouts, scripts, or apps that help doctors explain generics to patients in under 60 seconds.
It’s not about forcing doctors to prescribe generics. It’s about giving them the facts, the data, and the confidence to make informed choices. When they do, patients get better care - and the system saves billions.
Generic drugs aren’t second-rate. They’re the same medicine, made under the same rules. But until doctors believe that - truly believe it - the potential will stay locked away.
Do generic drugs work as well as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also be bioequivalent - meaning they deliver the same amount of medicine into the bloodstream at the same rate. Studies show that 95% of generic prescriptions are therapeutically equivalent to their brand-name counterparts. The differences most people notice - like side effects - are usually due to inactive ingredients, not the medicine itself.
Why do some doctors avoid prescribing generics?
Some doctors worry about inconsistent quality between manufacturers, especially for drugs with narrow therapeutic indexes like warfarin or levothyroxine. Others have seen patients report side effects after switching - even if those effects aren’t scientifically linked to the generic. Lack of training, time constraints, and outdated beliefs also play a role. Many weren’t taught how to interpret bioequivalence data, and they rely on anecdotal experience instead.
Are generic drugs made in the same facilities as brand-name drugs?
Sometimes. In fact, many brand-name companies also manufacture generic versions of their own drugs under different labels. The FDA inspects all facilities - whether they make brand or generic drugs - using the same standards. About 50% of generic drugs are made in U.S. facilities; the rest are made overseas, but all must meet FDA quality requirements. The issue isn’t where they’re made - it’s whether doctors trust the data.
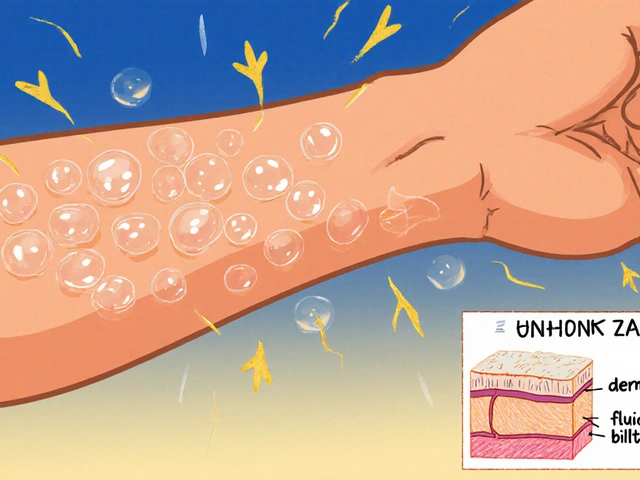
Can switching to a generic cause side effects?
It’s rare, but possible - and usually not because the active ingredient is different. Side effects can happen if the inactive ingredients (like dyes or fillers) trigger allergies or intolerance. For example, someone allergic to a dye in one generic version might react, while another generic without that dye is fine. This is why switching between different generic brands can sometimes cause issues. It’s not the medicine - it’s the packaging.
How can patients encourage their doctor to prescribe generics?
Ask directly: “Is there a generic version available? Can we try it?” Bring up cost if it’s a concern - many doctors don’t realize how much patients struggle with price. Don’t assume your doctor knows the latest data. Offer to look up the FDA’s bioequivalence info together. Most doctors are willing to switch if they feel confident the generic is safe and effective.










11 Comments
Let’s be real - this isn’t about science. It’s about habit. I’ve seen consultants in London still prescribe brand-name statins because ‘that’s what we’ve always done.’ The data doesn’t lie, but human psychology? That’s a different beast entirely.
As a pharmacist in Mumbai, I’ve seen patients panic when switched to generics - not because the drug failed, but because the pill looked different. Color, shape, size - these things matter more than bioequivalence percentages. Doctors need to explain this, not just prescribe.
My mom switched to generic levothyroxine and felt like a zombie for three weeks. She went back to brand - and boom, energy returned. I know the data says it’s the same, but lived experience doesn’t care about stats.
It’s concerning how many doctors still equate price with quality. I’ve worked in clinics where patients were switched without any counseling - and then blamed the medication when side effects appeared. Education is the missing link.
Look, most doctors are just lazy. They don’t want to look up bioequivalence studies, they don’t want to explain inactive ingredients, and they certainly don’t want to deal with patients who ‘don’t trust science.’ So they default to brand names - and call it ‘clinical caution.’ It’s not caution. It’s intellectual laziness wrapped in a white coat.
And don’t get me started on the FDA’s 80-125% window. That’s a 45% swing in absorption! If you’re dosing insulin or warfarin, that’s not ‘equivalent’ - that’s Russian roulette with your thyroid.
Medical schools are failing. Pharma reps are winning. And patients? They’re the ones paying the price - in dollars, in side effects, in lost trust.
PS: I’ve read every single FDA guidance document on generics. If you haven’t, you have no right to opine on this. 😎
Change is slow, but it’s happening. I’ve seen residents who learned about generics in med school actually prescribe them confidently - and patients respond better because they feel heard. It’s not about forcing doctors - it’s about empowering them with tools, not guilt.
Many African nations rely entirely on generics due to cost - and outcomes are comparable to Western nations. The issue is not the drug - it is the narrative. When doctors transmit fear, patients absorb it. We must reframe the conversation from suspicion to science.
Real-world data is the game-changer. My hospital started sharing dashboards showing how patients on generics had fewer ER visits than those on brand - same condition, same compliance. Within six months, our generic rate jumped from 40% to 78%. Doctors don’t resist facts - they resist assumptions.
Ugh. I’ve seen this so many times. Doctors say ‘it’s the same’ - but then they won’t take it themselves. Hypocrites. If it’s good enough for my grandma on Medicare, it’s good enough for your rich patient who won’t pay $300 for a pill.
From a pharmacoeconomic standpoint, the 17.3:1 ROI on physician education is undeniable. Yet, the system continues to incentivize brand promotion over evidence-based prescribing. This isn’t a clinical issue - it’s a structural failure of medical economics.
Here’s the truth no one wants to say: The real problem isn’t doctors - it’s the FDA’s outdated regulatory framework. The 80-125% bioequivalence window is a relic from the 1980s. We need dynamic, patient-specific thresholds - especially for narrow-therapeutic-index drugs. Until then, we’re all just guessing.
And yes, I’ve reviewed the GDUFA III documents. The loopholes are staggering. 🧪📉