When a senior falls, it’s not just a bump or bruise. It can mean a broken hip, a hospital stay, or even death. So when doctors talk about putting an 80-year-old on a blood thinner to prevent stroke, families often panic: What if they fall? Won’t that make things worse? The fear is real. But the data tells a different story.
Why Seniors Need Anticoagulants
About 9 out of every 100 adults over 65 have atrial fibrillation - an irregular heartbeat that lets blood pool in the heart. That pooling can form clots. If a clot breaks loose, it can travel to the brain and cause a stroke. And stroke risk doesn’t creep up with age - it skyrockets. At 50-59, the annual risk is 1.5%. By 80-89, it’s 23.5%. That’s more than one in four people having a stroke in a single year if nothing is done. Anticoagulants - blood thinners - cut that risk dramatically. Warfarin, used since the 1950s, reduces stroke risk by about two-thirds. Newer drugs like apixaban, rivaroxaban, dabigatran, and edoxaban (called DOACs) do just as well, sometimes better. In the ARISTOTLE trial, apixaban lowered stroke risk by 21% compared to warfarin. In the RE-LY trial, dabigatran reduced strokes by 88% compared to placebo. And here’s the kicker: anticoagulants work better than aspirin. Aspirin cuts stroke risk by only 22%. Anticoagulants cut it by 64%. That’s not a small difference. That’s the difference between living independently and being confined to a nursing home after a stroke.The Fall Fear: Real, But Overblown
Yes, seniors on blood thinners who fall are more likely to bleed - and bleed badly. A fall that might just cause a bruise in someone not on anticoagulants can lead to a brain bleed in someone who is. Minnesota hospital data shows elderly patients on anticoagulants have a 50% higher chance of intracranial hemorrhage after a fall. And 90% of fall-related deaths involve either people over 85 or those on blood thinners. But here’s what most people don’t realize: Most seniors on anticoagulants never fall. And even those who do? The chance of having a stroke without treatment is far higher than the chance of dying from a fall. A landmark study called BAFTA looked at 812 patients with an average age of 81.5. Half got warfarin. Half got aspirin. After a year, the warfarin group had 52% fewer strokes or clots traveling to other organs. And there was no significant increase in major bleeding. The same pattern held in studies of people in their 80s and 90s. In fact, the oldest patients - those 85 and up - got the most benefit. Their stroke risk was highest, so preventing even one stroke saved more lives than the extra bleeds caused.What Doctors Are Still Getting Wrong
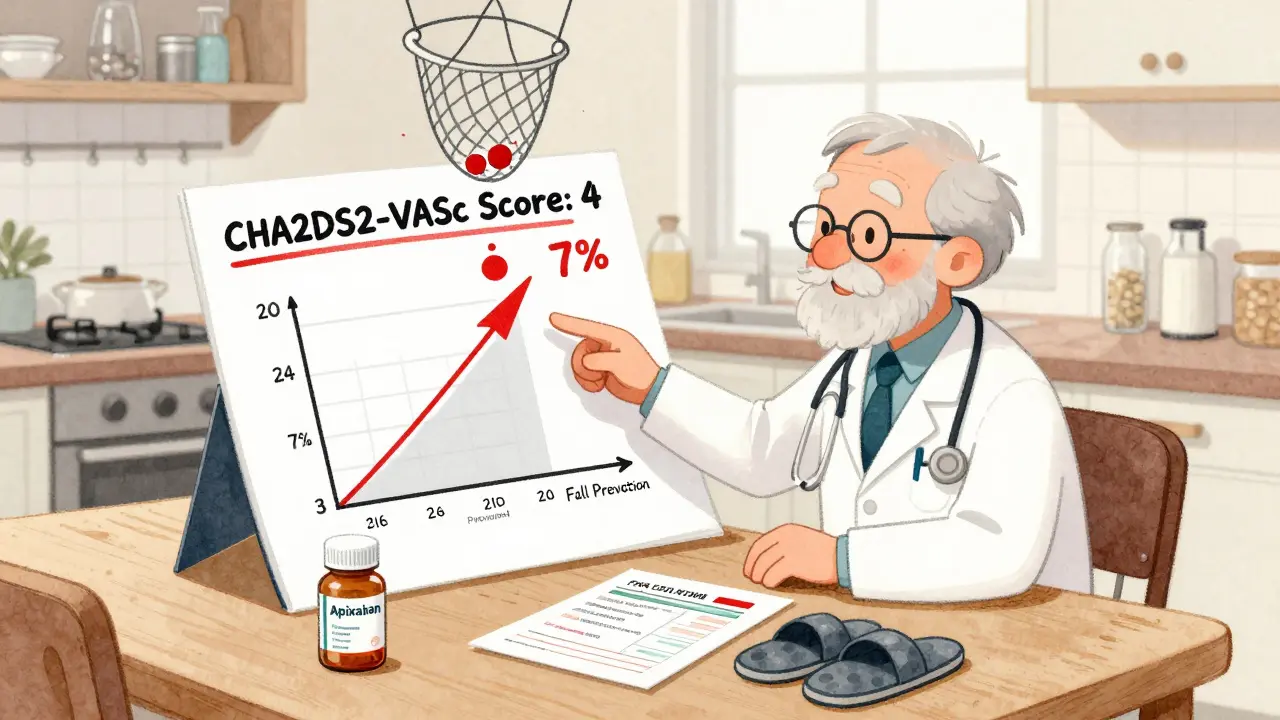
Despite all this, only about half of eligible seniors are getting anticoagulants. In those over 85, it’s as low as 48%. Why? Because many doctors still believe fall risk is a reason to avoid treatment. A 2021 survey of primary care doctors found 68% would refuse anticoagulants for an 85-year-old with two falls in the past year - even if their stroke risk score (CHA2DS2-VASc) was 4, meaning they had a 7% annual risk of stroke. That’s not cautious. That’s dangerous. Guidelines from the American College of Cardiology, American Heart Association, and Heart Rhythm Society have been clear since 2019: Age alone should not be a reason to withhold anticoagulation. And the 2020 European Society of Cardiology guidelines go even further: Anticoagulation is recommended for all AF patients with CHA2DS2-VASc ≥2 - even the very elderly. The Journal of Hospital Medicine labeled stopping anticoagulants because of fall risk as one of the “Things We Do for No Reason™.” They wrote: “While anticoagulants increase bleeding risk in older adults who fall, this risk does not outweigh the stroke prevention benefits.”
Choosing the Right Blood Thinner
Not all anticoagulants are the same, especially for seniors. Warfarin works well, but it’s tricky. It needs regular blood tests (INR checks every 4 weeks on average). Too little, and the stroke risk stays high. Too much, and bleeding risk spikes. Many seniors can’t keep up with the appointments or dietary restrictions. DOACs - apixaban, rivaroxaban, dabigatran, edoxaban - are simpler. No regular blood tests. Fixed doses. But they have downsides. Most are cleared by the kidneys. As people age, kidney function drops. A 90-year-old might have a creatinine clearance of 30 mL/min. That’s too low for full doses of some DOACs. Dose adjustments are needed. Apixaban is the most forgiving here - it’s the only DOAC with a low-dose option (2.5mg twice daily) approved for seniors with reduced kidney function. Also, DOACs don’t have universal reversal agents. But we do have options now. Idarucizumab reverses dabigatran. Andexanet alfa reverses rivaroxaban and apixaban. Both were approved by the FDA in 2015 and are available in hospitals. They’re not perfect, but they’re life-saving when a major bleed happens.How to Stay Safe While on Anticoagulants
You don’t have to just accept the risk of falling. You can reduce it. Start with a fall risk assessment. Tools like the Morse Fall Scale or the Hendrich II model help identify what’s making someone prone to falls. Then tackle the causes:- Review all medications. Sedatives, sleeping pills, opioids, and even some blood pressure drugs can make you dizzy. Cut what you can.
- Test vision and hearing. Poor sight or hearing increases fall risk.
- Remove trip hazards. Loose rugs, cluttered hallways, poor lighting - fix them.
- Install grab bars in bathrooms and handrails on stairs.
- Use a cane or walker if recommended.
- Try the Otago Exercise Program. It’s a simple home-based routine proven to reduce falls by 35% in seniors.
What the Numbers Really Mean
Let’s say you have 100 seniors with atrial fibrillation and a CHA2DS2-VASc score of 4. Without anticoagulation, about 7 will have a stroke in one year. With anticoagulation, only 1 or 2 will. How many will have a major bleed? About 3. So out of 100 people: 24 strokes are prevented. 3 major bleeds occur. That’s a net benefit of 21 avoided bad outcomes. That’s not a gamble. That’s a win. And if you add in fall prevention? The bleed risk drops even further. Studies show that when seniors on anticoagulants get proper fall risk management, their bleeding rates are no higher than those not on blood thinners.Bottom Line: Don’t Stop the Meds Because of a Fall
Falls are scary. Bleeds are scary. But strokes are worse. A stroke can steal your speech, your movement, your independence. A fall might mean a broken hip - but with rehab, many seniors recover. A stroke? Recovery is harder. Many never go home. The evidence is clear: For seniors with atrial fibrillation, the benefits of anticoagulation far outweigh the risks - even if they’ve fallen before. Stopping these medications because of fall risk is not safer. It’s riskier. Talk to your doctor. Ask about your CHA2DS2-VASc score. Ask about DOACs. Ask about fall prevention. Don’t let fear make the decision for you. The data doesn’t lie. Anticoagulants save lives in seniors. And with the right precautions, they can do it safely.Should seniors stop anticoagulants after a fall?
No. A single fall is not a reason to stop anticoagulation. The risk of stroke without treatment is much higher than the risk of a serious bleed from a fall. Stopping the medication increases the chance of a disabling or fatal stroke. Instead, focus on preventing future falls through home safety changes, medication review, and exercise programs like Otago.
Are DOACs safer than warfarin for elderly patients?
Yes, for most seniors. DOACs like apixaban and rivaroxaban have lower rates of brain bleeding and don’t require frequent blood tests. Apixaban has shown the best safety profile in patients over 75, with 31% less major bleeding than warfarin. However, DOACs need kidney function monitoring, and dosing may need adjustment in those with reduced kidney function.
Can I take aspirin instead of a blood thinner?
No. Aspirin reduces stroke risk by only about 22%, while anticoagulants reduce it by 64%. For someone with atrial fibrillation, aspirin is not enough protection. Major guidelines no longer recommend aspirin for stroke prevention in AF patients because it’s ineffective compared to anticoagulants.
What if my parent has kidney problems?
Kidney function matters. DOACs are cleared by the kidneys, so if creatinine clearance drops below 50 mL/min, dose adjustments are needed. Apixaban is the safest option for those with moderate kidney decline, as it has a low-dose form approved for seniors. Warfarin doesn’t rely on kidneys, but it requires frequent monitoring. Your doctor should check kidney function every 6-12 months and adjust treatment accordingly.
Is it safe to be on anticoagulants past age 90?
Yes. Studies show patients aged 90 and older get the greatest net benefit from anticoagulants because their stroke risk is highest. A 2015 study of 386 people over 90 found they had fewer strokes and better survival on anticoagulants than those not treated. Age alone is not a reason to avoid treatment - the key is choosing the right drug and managing fall risk.







14 Comments
My grandma was on warfarin for AFib and fell once - broke her wrist, not her skull. She’s 89, walks with a cane, does Otago twice a week, and still makes her famous apple pie. People act like anticoagulants are a death sentence, but it’s not the medicine that kills you - it’s the fear. The data doesn’t lie. If you’re not on a blood thinner and you’ve got AFib, you’re playing Russian roulette with your brain.
Stop treating seniors like fragile glass figurines. They’ve lived long enough to know what they can handle.
Also - DOACs are a miracle. No more monthly blood draws. My mom’s INR used to be all over the place. Now she just swallows her apixaban and forgets about it. Life is better.
And yes, kidney function matters. But that’s why we have labs. Not a reason to deny treatment.
Fall risk? Fix the rugs. Check the meds. Get a walker. Don’t stop the medicine that keeps them alive.
I’m so tired of doctors treating elderly patients like they’re already dead.
Oh here we go again with the ‘data says’ nonsense. You think Big Pharma doesn’t love pushing these DOACs? They cost $500 a month. Warfarin is 20 cents. And who pays for the reversal agents when someone bleeds out in the ER? YOU DO. And don’t even get me started on how many of these ‘safe’ drugs get pulled off the market 5 years later.
My uncle took rivaroxaban and ended up in the ICU with a brain bleed after tripping over his dog. He was 82. He didn’t need it. He had a CHA2DS2-VASc of 3 - barely above the line. But the cardiologist pushed it like it was a new iPhone.
Stop gaslighting families. Fear of stroke is real - but so is fear of being turned into a bleeding mess because some algorithm said ‘yes’.
Wow. Just wow. You people are so gullible. The ‘strokes are worse than bleeds’ argument is a lie. Stroke survivors often live for years - with tubes, diapers, and zero quality of life. Bleeds? They’re sudden. Quick. Sometimes peaceful. You think your grandma’s 90-year-old body is gonna recover from a stroke? She’s not gonna ‘make apple pie’ - she’s gonna sit in a chair drooling while you cry over her.
And the ‘DOACs are safer’ claim? That’s from industry-funded trials. Real-world data? DOACs have higher rates of GI bleeds. And guess who gets stuck with the bill? Medicaid. Medicare. YOU.
Also - why is aspirin ‘not enough’? Because the guidelines were rewritten by pharma lobbyists. Aspirin is 100x cheaper and has been used for 100 years. You want to live longer? Stop taking expensive junk and eat more garlic.
And yes - I’ve read every guideline. I know what they say. That doesn’t mean they’re right.
Hey everyone, i just wanted to say i really appreciate this post. My dad is 86 and has afib, and we were so scared after he slipped in the bathroom last winter. We thought we had to stop his medicine. But after reading this, we went to his doctor and asked about apixaban and fall prevention. Turns out his kidney function is okay, and they switched him from warfarin to apixaban 2.5mg twice a day. He also started the otago program and got grab bars installed. He’s been fall-free for 6 months now.
And honestly? He feels better. Less anxious. Like he’s not living in fear. That’s huge.
Also, i think we need to talk more about how doctors are still scared to prescribe these meds to seniors. My dad’s first doc said ‘you’re too old’ - but his second one actually listened. It made all the difference.
To anyone reading this: please, please, please don’t let fear make the decision. Talk to your doctor. Ask for the CHA2DS2-VASc score. Ask about kidney tests. Ask about fall prevention. You’re not being a burden - you’re being smart.
And to the family members: be the advocate. We’re the ones who see them every day. We know when they’re wobbly. We know when they’re scared. Let’s use that knowledge to protect them - not to stop their meds.
Love you all. Stay safe.
- nishant (from india, but my dad lives in florida 😊)
Let’s cut through the propaganda. The ‘net benefit’ argument is mathematically dishonest. You’re comparing 7 strokes to 3 bleeds - but you’re not accounting for the fact that 70% of those strokes are non-disabling. Meanwhile, 40% of major bleeds are fatal. And you’re ignoring the psychological trauma - the fear, the isolation, the loss of autonomy that comes with living on anticoagulants.
Also, the ‘Otago program reduces falls by 35%’? That’s from a 2012 RCT with 150 participants. Real-world adherence? Less than 20%. Most seniors can’t do it. The data is cherry-picked.
And why are we ignoring the fact that 60% of seniors on DOACs are on them because their doctor didn’t want to manage INR? That’s convenience, not care.
And what about the 12% of patients who develop spontaneous bleeds without falling? That’s not ‘fall risk’ - that’s drug risk.
This isn’t medicine. It’s corporate policy dressed up as science.
Oh, how darling. Another ‘data-driven’ sermon for the elderly. How quaint. You treat seniors like statistical abstractions - ‘7 strokes prevented, 3 bleeds incurred’ - as if they’re not people with dignity, fears, and the right to say ‘no.’
And yet - you’re the same people who would never let your 25-year-old child take a 10% risk of brain hemorrhage from a new experimental drug. But 85? Oh, they’re ‘high-risk’ so they’re fair game for pharmaceutical experiments.
How noble. How enlightened. How utterly condescending.
Let them die peacefully. Let them live without being turned into a walking bleeding risk. Not every life must be extended. Some lives deserve peace - not a pill that turns their body into a time bomb.
And please. Don’t tell me about ‘fall prevention.’ I’ve seen the ‘grab bars’ in nursing homes. They’re bolted to walls that are falling apart. It’s performative safety.
Stop pretending you’re saving them. You’re just making them compliant.
As someone who’s worked in geriatrics for 28 years, I’ve seen both sides. I’ve held the hands of patients who had strokes - silent, terrifying, irreversible. And I’ve held the hands of those who bled out after a fall - sudden, shocking, heartbreaking.
But here’s what I know: the fear of bleeding is real. But the fear of stroke is deeper. It steals identity. It steals connection. It steals the ability to hear your grandchild’s voice.
DOACs aren’t perfect. But for most seniors - especially those over 80 - they’re the best tool we have. Apixaban is the gold standard. Low dose. Kidney-friendly. Proven.
And yes - fall prevention works. Not because it’s trendy. Because it’s basic human care. Check meds. Fix lighting. Remove rugs. These aren’t ‘hacks.’ They’re dignity.
Don’t let fear silence the science. Let’s give seniors the chance to live - not just survive.
My mom’s on apixaban and she’s 88 and still dances with her grandkids 💃❤️ Stop letting fear steal their joy. Fix the house. Move the rugs. Get a walker. Don’t stop the meds. Life is worth the risk.
It is, indeed, a profoundly disconcerting phenomenon - the manner in which medical paternalism, under the guise of ‘evidence-based practice,’ has come to supplant the autonomy of the elderly. One is reminded of the early 20th-century eugenics movement, wherein the ‘greater good’ was invoked to justify the subjugation of the vulnerable.
Anticoagulants, while statistically efficacious in cohort studies, fail to account for the phenomenological reality of aging - the erosion of agency, the quiet dignity of accepting mortality, the refusal to be turned into a data point.
Moreover, the promotion of DOACs as ‘safer’ is a rhetorical sleight-of-hand. The absence of INR monitoring does not equate to safety; it equates to convenience - for the physician, for the pharmacy, for the insurer.
One must ask: who truly benefits? Not the patient. Not the family. But the pharmaceutical-industrial complex.
And so, we must resist. Not out of ignorance - but out of reverence.
For to treat the elderly as mere vessels for statistical optimization is to deny their humanity.
Just wanted to say thank you for writing this. My dad is 91 and was on warfarin for years. We were terrified after he slipped in the shower. We almost stopped the meds. But we talked to his geriatrician, got his kidney checked, switched him to low-dose apixaban, and installed a shower seat and night lights. He hasn’t fallen since. He’s still reading the newspaper every morning.
I think a lot of us are scared because we don’t know what to do. This post gave us direction.
And to the people saying ‘it’s all about money’ - I get it. But my dad’s life isn’t a profit margin. It’s a person. And he’s still here. Because we chose to act - not out of fear, but out of care.
Thanks again.
- patrick (and yes, i typed this on my phone. sorry for the typos.)
Excellent, thorough breakdown. I appreciate the nuance - especially the emphasis on dose adjustment for renal function and the distinction between warfarin and DOACs.
One point I’d add: many families don’t realize that anticoagulants aren’t ‘all or nothing.’ If a senior falls and is stable, discontinuing therapy is rarely indicated. The risk of thromboembolism increases exponentially within days of stopping.
Also - reversal agents are not theoretical. In our hospital, we’ve used andexanet alfa three times in the last year for DOAC-related bleeds. All three patients survived with no neurological deficit.
It’s not about ignoring risk. It’s about managing it intelligently.
And yes - aspirin is not a substitute. That myth needs to die.
Let me tell you about my aunt. She was 89. On apixaban. Fell. Brain bleed. Died in 48 hours. Her CHA2DS2-VASc was 3. She didn’t need it. The doctor was just lazy. Didn’t want to monitor INR. So he pushed the ‘new’ drug. Now she’s dead.
And you people are out here saying ‘the data says’? The data doesn’t know her name. The data doesn’t know she loved gardening. The data doesn’t know she was afraid of needles.
Stop weaponizing statistics to justify medical negligence.
And don’t give me this ‘fall prevention’ nonsense. You think a grab bar stops a 90-year-old from collapsing from orthostatic hypotension because their blood pressure med was increased last week?
This isn’t prevention. It’s denial.
Stop pretending you’re saving lives. You’re just pushing pills.
My grandma took apixaban, fell once, got a bruise, kept dancing 🕺💖 #DontStopTheMeds #SeniorsDeserveToLive
Just read Chris Van Horn’s comment. My grandma was his aunt. She didn’t die from a bleed. She died because they stopped her anticoagulant after one fall - and she had a massive stroke two weeks later. They told us it was ‘natural causes.’
She was 89. She loved salsa dancing. She had a CHA2DS2-VASc of 5. She was supposed to be on a blood thinner.
They took it away because they were scared.
And now I’m scared too - scared that people still believe this myth.
Don’t let fear kill your loved ones. Let data - and love - guide you.