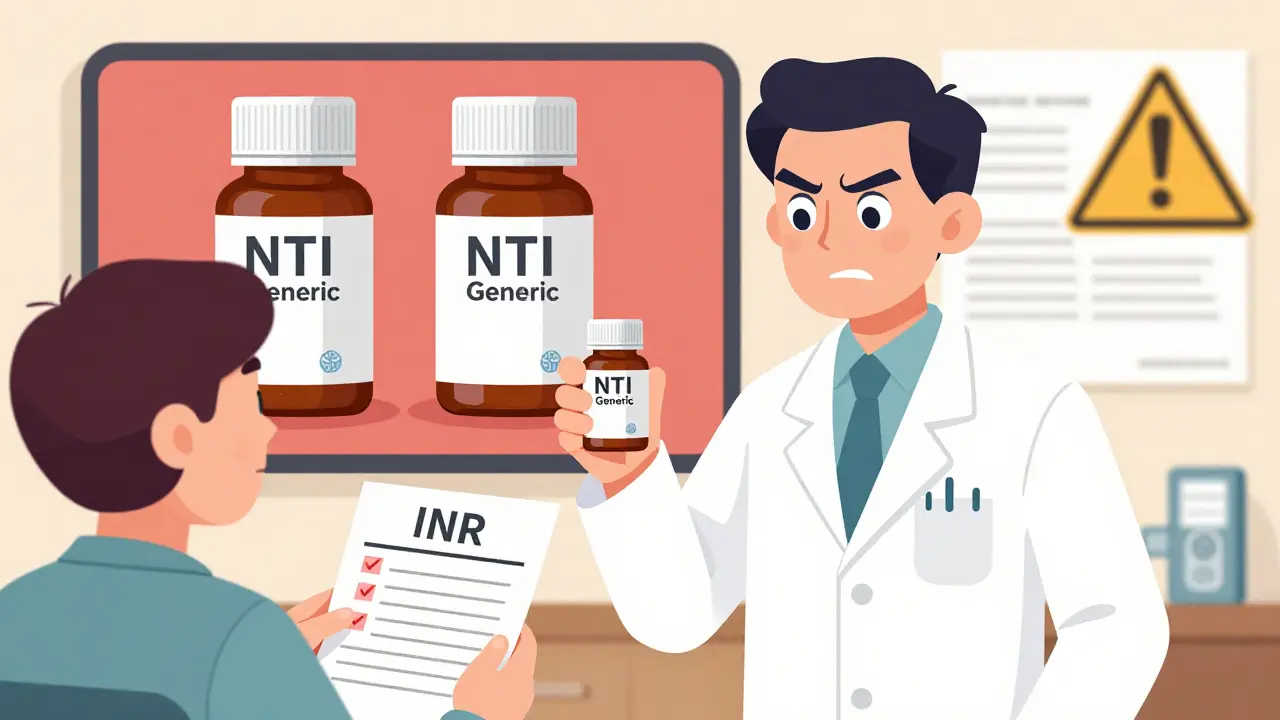
When a pharmacist hands you a pill bottle labeled NTI generics, it might look just like any other generic prescription. But behind that simple label is a complex, high-stakes decision that can mean the difference between stable health and a hospital visit. For pharmacists, NTI generics aren’t just about cost savings-they’re about patient safety, unpredictable bioavailability, and a system that’s still catching up to the risks.
What Exactly Are NTI Generics?
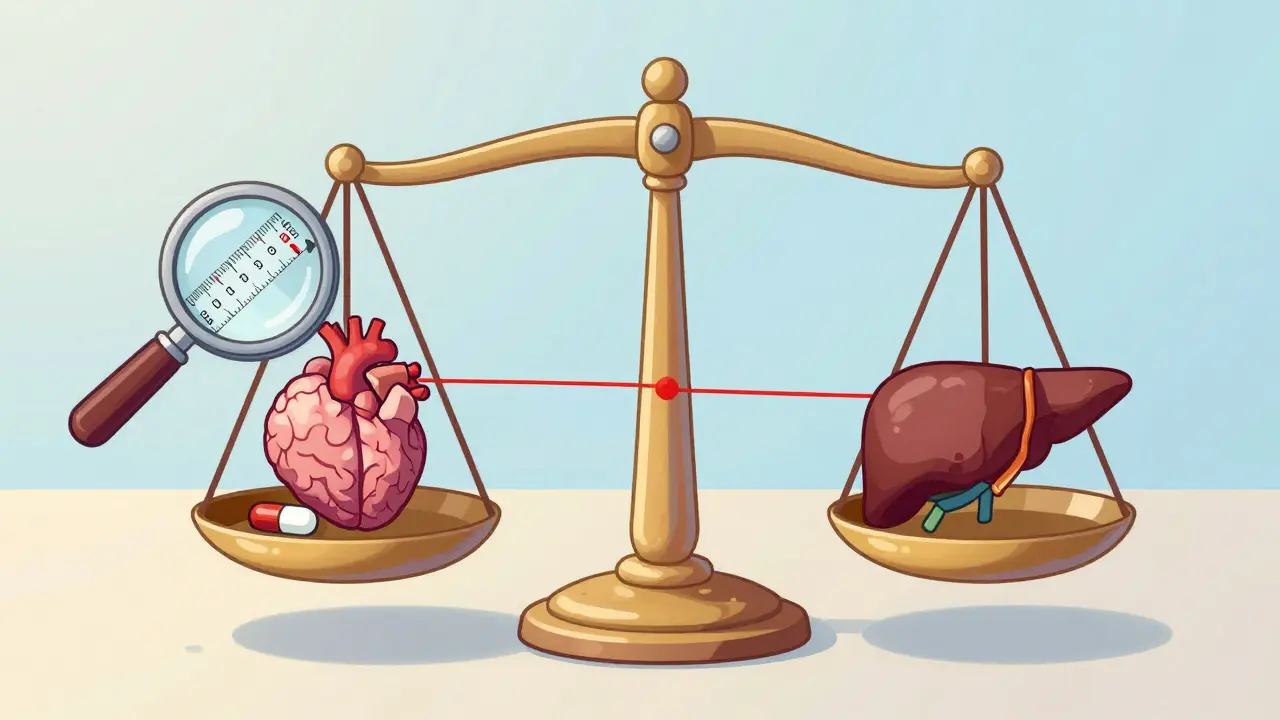
Narrow Therapeutic Index (NTI) drugs are medications where even tiny changes in blood levels can cause serious harm. A little too much, and you risk toxicity. A little too little, and the treatment fails. Think of it like walking a tightrope-there’s no room for error. Common examples include warfarin (a blood thinner), levothyroxine (for thyroid conditions), and phenytoin (for seizures). These drugs require precise dosing, and many need regular blood tests to make sure levels stay in the safe zone.
Generic versions of these drugs are approved under the same rules as other generics, but here’s the problem: the standard bioequivalence range for most generics is 80% to 125% of the brand-name drug’s absorption. For NTI drugs, that’s too wide. The FDA recommends a tighter range of 90% to 111% for these critical medications. Even then, many pharmacists say it’s not enough.
Why Pharmacists Are Worried
In 2024, the American Society of Health-System Pharmacists (ASHP) surveyed over 1,200 pharmacists. Sixty-eight percent said they have real concerns about switching patients between different NTI generics. Why? Because the drugs aren’t always the same, even when they’re labeled as identical.
One hospital pharmacist in Ohio told me about a patient on warfarin who had stable INR levels for years. After a pharmacy switch, the patient got a different generic version. Within days, their INR spiked dangerously high. They ended up in the ER with a bleeding ulcer. The new generic wasn’t defective-it was approved. But the difference in how the body absorbed it was enough to cause harm.
These aren’t isolated cases. The FDA’s Adverse Event Reporting System recorded 1,247 adverse events linked to NTI generic substitutions between 2020 and 2024. For non-NTI generics, that number was just 382. That’s more than triple the risk.
The Substitution Problem
Most states allow pharmacists to substitute generic drugs without telling the prescriber. But for NTI drugs, that’s where things get dangerous. Only 28 states have laws that restrict automatic substitution for NTI medications. In the other 22, a pharmacist might swap a patient’s brand-name levothyroxine for a cheaper generic without the doctor even knowing.
And it’s not just about switching from brand to generic. It’s about switching between different generic brands. One manufacturer’s version of phenytoin might have slightly different fillers, coatings, or manufacturing processes. Those tiny differences can change how the drug dissolves in the body. For a patient on a tight therapeutic window, that’s enough to throw off their entire treatment.
According to a 2024 University of Florida study, 34% of pharmacists would never automatically substitute warfarin generics-compared to just 8% for non-NTI drugs. That’s a huge gap in practice, and it shows how deeply pharmacists understand the risk.

Supply Chain Chaos
NTI drugs are also more vulnerable to shortages. In 2024, the FDA reported 47 shortages of NTI drugs-17.4% of all drug shortages, even though NTI generics make up only 6% of generic prescriptions. Why? Because most generics are manufactured overseas. The University of Minnesota found that 80% of all generics are finished in foreign countries, and for NTI drugs, that number is even higher.
When one overseas factory has a quality issue, it doesn’t just delay one drug-it can disrupt treatment for hundreds of patients. And when a pharmacy switches to a different generic supplier because the first one ran out, that’s another potential trigger for instability. The FDA says 23% of NTI drug shortages were worsened by switching between manufacturers.
On top of that, the new Medicare Drug Price Negotiation Program, starting in 2026, includes three NTI drugs among its first 10 targets. Pharmacists are worried. A 21-day reimbursement delay under this program could make it harder for community pharmacies to keep stock on hand. If a pharmacy can’t afford to buy the drug upfront, patients go without.
What Pharmacists Are Doing About It
Many hospitals and health systems are taking matters into their own hands. The ASHP recommends keeping patients on the same generic manufacturer whenever possible. Sixty-three percent of hospital systems now have policies to stick with one source for NTI drugs. That means if you start on one brand of levothyroxine, you stay on it-no switches unless absolutely necessary.
Pharmacists are also pushing for better tools. The FDA’s Therapeutic Equivalence Ratings database is updated quarterly and helps identify which generics are considered interchangeable. But many pharmacists say it’s outdated. The American Association of Colleges of Pharmacy is calling for stricter bioequivalence standards, especially for drugs with complex chemistry like chiral molecules (where mirror-image versions of the drug behave differently in the body).
Pharmacy residency programs are finally catching up. In 2024, 81% of these programs added specialized NTI drug training. Pharmacists now learn how to interpret therapeutic drug monitoring results, recognize early signs of instability, and communicate effectively with prescribers and patients.
What Patients Need to Know
If you’re on an NTI drug, here’s what you should do:
- Ask your pharmacist: “Is this the same manufacturer as last time?” If it’s changed, ask if switching is safe.
- Don’t assume a generic is interchangeable. Just because it’s cheaper doesn’t mean it’s identical.
- Keep your blood tests on schedule. If you’re on warfarin, levothyroxine, or phenytoin, regular monitoring is non-negotiable.
- If you feel different after a switch-more tired, dizzy, or anxious-tell your doctor immediately. Don’t wait.
- Ask your prescriber to write “Dispense as Written” or “Do Not Substitute” on your prescription. It’s legal, and it gives you control.
One independent pharmacy owner in Oregon told me that when generics were available, patient abandonment for NTI drugs dropped by 35%. That’s huge-many patients couldn’t afford the brand. But he also saw four cases in a year where switching generics led to hospital visits. The trade-off is real.
The Bigger Picture
NTI generics are a perfect example of how cost-saving policies can unintentionally create new risks. The system was built on the assumption that all generics are the same. But for these critical drugs, they’re not. The FDA’s 2025 announcement of a new bioequivalence framework for 12 high-priority NTI drugs is a step forward. But experts say it’s not enough. The standards still don’t account for real-world variability in manufacturing, storage, or patient metabolism.
Pharmacists aren’t against generics. They support access to affordable medicine. But they’re asking for a system that doesn’t treat all drugs the same. For NTI drugs, precision matters more than price.
By 2027, 74% of healthcare systems plan to have pharmacist-led NTI drug stewardship programs. That means pharmacists will have a formal role in deciding which generics are safe for which patients. It’s a shift from passive dispensing to active clinical involvement. And for patients on these drugs, that might be the most important change of all.
Are all generic drugs the same?
No. While most generics are bioequivalent to their brand-name versions, NTI drugs like warfarin, levothyroxine, and phenytoin are different. Even small changes in how the body absorbs these drugs can cause serious side effects or treatment failure. Two generics of the same NTI drug may not be interchangeable for every patient.
Can pharmacists switch my NTI generic without telling me?
In most states, yes. Only 28 states have laws that restrict automatic substitution for NTI drugs. In the rest, pharmacists can swap your prescription for a different generic without notifying you or your doctor. Always ask if your medication changed, and consider asking your prescriber to write “Dispense as Written” on your prescription.
Why are NTI drugs more likely to have shortages?
NTI drugs are often manufactured overseas, and their production requires stricter quality controls. When one factory has a problem-like contamination or equipment failure-it can cause a ripple effect. Because there are fewer manufacturers for these drugs, and switching suppliers can destabilize patient treatment, shortages hit harder and last longer.
What should I do if I feel different after switching to a new generic?
Don’t ignore it. If you’re on an NTI drug and notice new symptoms-like unexplained fatigue, dizziness, irregular heartbeat, or mood changes-contact your doctor right away. These could be signs your drug levels have shifted. Request a blood test if you’re on warfarin, levothyroxine, or phenytoin. Bring the new bottle to your appointment so your provider can check the manufacturer.
Is it safer to stick with the brand-name NTI drug?
For some patients, yes. Brand-name versions are more consistent because they’re made by a single manufacturer with standardized processes. But generics are often much cheaper, and many patients do well on them-especially if they stay on the same generic version. The key is consistency: once you find a generic that works, stick with it unless your doctor advises otherwise.




12 Comments
I’ve been on levothyroxine for 12 years, and I swear by staying on the same generic. One time my pharmacy switched me without telling me, and I felt like I was dragging through concrete for two weeks. My TSH went haywire. Turned out the new brand had a different filler. I now ask for the manufacturer by name every time. Don’t let them play Russian roulette with your thyroid.
Oh here we go again with the pharma fearmongering. You want precision? Pay for brand name. The FDA approves these generics. If your body can’t handle a 10% swing in absorption, maybe you’re the problem, not the system. Stop coddling patients and let the free market work. Also, 80% of generics are made overseas? So what? China makes my phone too, and it doesn’t explode.
Ryan, you’re missing the point entirely. It’s not about coddling-it’s about pharmacology. NTI drugs aren’t like ibuprofen. A 10% swing in warfarin can cause a stroke or a bleed. The FDA’s 90–111% range is a guideline, not a guarantee. Manufacturing variability? Yes. Patient metabolism? Yes. Storage conditions? Also yes. And when you’re on a tightrope, even a breeze matters. This isn’t fearmongering-it’s clinical reality. I’ve seen patients crash because a pharmacy swapped generics. No one’s asking for luxury. We’re asking for consistency.
Also, your phone doesn’t have a half-life. Your thyroid does.
HAHAHAHA. So we’re now in the era of pharmaceutical astrology? 🌌 The body is a temple, the pill is a sacred relic, and the pharmacist is the high priest of bioequivalence? How quaint. In ancient India, we used to dose with cow urine and moon phases-now we have chromatography and FDA paperwork. You want perfection? Live in a lab. Otherwise, adapt. Your body isn’t a precision watch. It’s a chaotic, beautiful mess. Embrace the variance. Or just… pay more. 💸🪷
Sam, you’re so extra 😂 But honestly? I get it. I’m on phenytoin. My neurologist won’t let me switch generics. I pay $180/month for the brand. My friend pays $12 for the generic. She had a seizure last year after a switch. So… yeah. I’m not mad. I’m just… sad that we live in a world where your life depends on which factory made your pill. 🤷♂️💊
Stephen, that hit me right in the feels. I’m a nurse, and I’ve had patients cry because they couldn’t afford the brand-and then got hospitalized after a switch. It’s not about being rich or poor. It’s about dignity. You shouldn’t have to risk your life because your insurance won’t cover the same pill you were on last month. We need better rules. Not just for NTI drugs-for all meds. People aren’t guinea pigs.
I just want to say thank you to the pharmacists who are pushing for change. I had no idea how much work goes into this. My mom’s on warfarin, and her pharmacist calls her every time there’s a switch. They even keep a log of which brand she’s on. That’s the kind of care we need more of. Not less.
My pharmacy in Vancouver switched my levothyroxine last year. I didn’t notice anything until my TSH came back weird. I asked for the old brand. They gave it to me. No hassle. No drama. Just good service. Maybe we don’t need more laws. Maybe we just need more pharmacists who care.
Don’t let anyone tell you it’s not worth fighting for. If you’re on an NTI drug, be your own advocate. Ask questions. Keep records. Know your manufacturer. Your life isn’t a cost center. You’re worth the extra step.
YESSSS this is so important!! 💪❤️ I used to think generics were all the same until my cousin had a bad reaction. Now I check every bottle like it’s a treasure map. And yes, I ask for "dispense as written"-no shame in that!! 🙌
There’s a deeper truth here: we treat medicine like a commodity, but biology is not a spreadsheet. We optimize for cost, not consequence. NTI drugs are a mirror. They show us what happens when we reduce human health to a line item. Maybe the real crisis isn’t the generics-it’s the mindset that says "good enough" is okay when someone’s life is on the line.
Anyone who still thinks generics are "just as good" hasn’t worked in a hospital. Or read a single adverse event report. This isn’t opinion. It’s data. And if you’re still defending automatic substitution for NTI drugs, you’re either dangerously naive or paid by a generic manufacturer. Pick one.