Generic drugs have long been the backbone of affordable healthcare. But the old model-copying a single active ingredient after patent expiry-is fading. Today, the real action is in generic combinations: smarter, more complex products that don’t just match branded drugs-they improve on them. These aren’t your grandfather’s generics. They’re fixed-dose combos, drug-device systems, extended-release pills, and even nanoparticle formulations designed to make treatment safer, simpler, or more effective. And the market is shifting fast.
What Exactly Are Generic Combinations?
Generic combinations are medicines that combine two or more active ingredients into one dosage form, or pair a drug with a device like an inhaler or auto-injector. Unlike traditional generics, which only need to prove they’re chemically identical to the brand, these products must show they offer a real therapeutic advantage. That means better absorption, fewer side effects, or improved patient adherence. Take the example of bupropion. A basic generic version sells for pennies. But Teva’s Budeprion XL, an extended-release version, commanded $187 million in annual sales before competitors entered. Why? Because it delivered steady blood levels throughout the day, reducing nausea and improving compliance. That’s the power of a well-designed combination. The FDA classifies these into three tiers by complexity:- Simple combinations: Oral tablets with two or more drugs, like blood pressure pills combining an ACE inhibitor and a diuretic. These make up 62% of today’s market.
- Complex combinations: Drug-device systems like inhalers or auto-injectors, or modified-release capsules. These are growing at nearly 10% a year.
- Super-complex combinations: Nanoparticle-based delivery, multi-layered tablets, or systems that target specific tissues. They’re only 10% of the market now-but growing over 12% annually.
Why Are They Growing So Fast?
The driver isn’t just innovation-it’s necessity. The generic drug market is drowning in price wars. Traditional generics lose 80-90% of their price within two years of launch. Margins vanish. Companies need a way out. Enter the super generic. These products keep the affordability of generics but command higher prices because they’re harder to copy. While a standard generic might sell at 5% margin, a complex combination can maintain 20-35% margins for five years or more. Add to that a massive wave of expiring patents. Between 2025 and 2030, branded drugs generating $217-236 billion in annual sales will lose exclusivity. High-value targets include:- Trelegy Ellipta (fluticasone/umeclidinium/vilanterol): $2.8 billion in U.S. sales in 2024.
- Austedo (deutetrabenazine): $1.2 billion in sales, used for movement disorders.
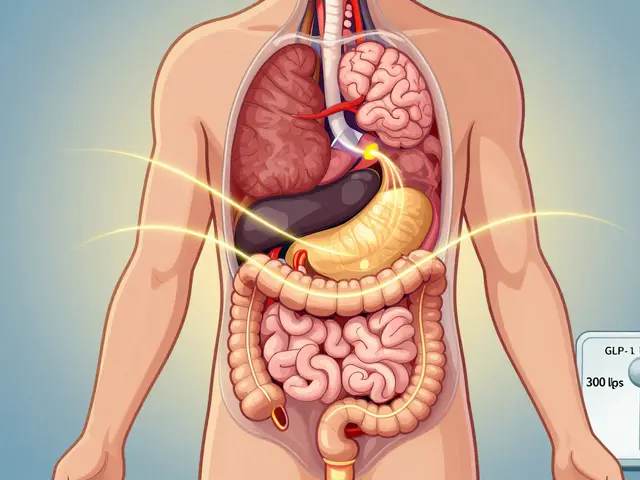
- GLP-1 agonists like semaglutide: A $100+ billion market with generic combos in development.
Regulatory Hurdles Are Real-But Changing
Getting approval for a generic combination is no walk in the park. Traditional generics require a standard ANDA (Abbreviated New Drug Application). For combos, the FDA demands more: additional clinical data, specialized bioequivalence studies, and proof that the delivery system works as intended. According to FDA internal data from 2024, approval timelines for complex combos are 18-24 months longer than for simple generics. Development costs jump from $1-5 million to $15-50 million. And 78% of rejections come not from the active ingredient, but from failure to prove equivalence in the delivery system-like an inhaler that doesn’t deliver the same particle size or an extended-release tablet that doesn’t match the original’s release profile. But regulators are adapting. In October 2025, the FDA launched a pilot program to fast-track reviews for generic combinations made entirely in the U.S. That could cut approval time by 3-6 months. The goal? Encourage domestic manufacturing and reduce reliance on overseas supply chains. Meanwhile, the European Medicines Agency (EMA) is moving slower. Through Q1 2025, the EU approved only 12 complex generic combinations. The U.S. approved 37. That gap creates a strategic problem: companies can’t just build one product and sell it everywhere. They need region-specific strategies.Who’s Winning and How?
The players aren’t just big pharma anymore. It’s the specialists-companies that understand formulation science, device integration, and regulatory strategy. Viatris and Credence merged for $2.3 billion in early 2025 to build a powerhouse in complex generics. Sandoz, now independent from Novartis, has pivoted entirely to high-value combinations. And companies like Aspen Pharmacare are developing generic versions of semaglutide combos-targeting the biggest drug market in decades. These aren’t just R&D plays. They’re manufacturing plays. Producing a stable, bioequivalent extended-release tablet requires hot-melt extrusion, lipid-based systems, and machines that control dosage ratios within ±2%. Only a handful of manufacturers globally have that capability. India leads in production volume, with 35% of global output, but U.S.-based facilities are gaining ground thanks to policy incentives. The winners will be those who partner early. Catalent is working with Hikma on auto-injectors. Other generic firms are teaming up with device makers to co-develop inhalers and patch systems. It’s no longer enough to be a drug company-you need to be a systems company.Therapeutic Areas That Are Exploding
Not all generic combos are created equal. Some markets are ripe. Others are saturated.- Oncology: Growing at 11.3% CAGR. Kinase inhibitors are being combined into single pills to simplify treatment for cancer patients.
- Respiratory: 9.89% CAGR. Inhalable combos for COPD and asthma are replacing multiple inhalers with one device.
- CNS: 8.7% CAGR. Combos for depression, Parkinson’s, and epilepsy are reducing pill burden and improving adherence.
- Cardiovascular: Still strong, but more crowded. New combos focus on fixed-dose pills with newer agents like SGLT2 inhibitors.

The Big Risks
There’s a trap here. Just because a combo is complex doesn’t mean it’s better. Some companies are pushing “me-too” versions with minor tweaks-adding a coating here, changing a release profile there-without meaningful clinical benefit. That’s dangerous. Harvard’s Dr. Aaron Kesselheim warned in NEJM 2025: “The therapeutic equivalence standard for complex generics remains inadequately defined.” In other words, if two products are labeled “bioequivalent,” but one delivers the drug unevenly, patients could be at risk. Regulatory agencies are scrambling to catch up. And then there’s pricing pressure. Even with higher margins, the overall generics market is under siege. Morningstar predicts a 30% margin erosion over the next decade unless companies can successfully transition to higher-value products. That’s why the race is on-not just to launch combos, but to launch the right ones.What’s Next?
The future of generics isn’t about being cheaper. It’s about being better. By 2030, super generics are expected to make up 35-40% of the total generics market value, up from under 20% today. Three trends will define the next decade:- Increasing complexity premium: Products with multiple innovations-drug + device + modified release-will command 2-3x the price of traditional generics.
- Regional divergence: The U.S. will keep moving fast on approvals. Europe will stay cautious. Companies must build separate pipelines.
- Manufacturing localization: U.S. and EU policies are pushing for domestic production. The days of outsourcing everything to India or China are ending.
Frequently Asked Questions
What’s the difference between a generic drug and a generic combination?
A traditional generic replicates a single active ingredient from a branded drug. A generic combination includes two or more active ingredients in one dosage form, or pairs a drug with a device like an inhaler or auto-injector. It must prove it offers a real therapeutic advantage-not just chemical similarity.
Why are generic combinations more expensive to develop?
They require more complex formulation science, specialized manufacturing equipment, and additional clinical data to prove bioequivalence and therapeutic advantage. While a simple generic costs $1-5 million and takes 2-3 years, a complex combination can cost $15-50 million and take 4-7 years.
Are generic combinations as safe as branded ones?
Yes-if they meet regulatory standards. The FDA and other agencies require the same level of safety testing as branded drugs. The challenge is ensuring equivalence in delivery systems, like inhalers or extended-release tablets, where small differences can affect how the drug is absorbed.
Which countries are leading in generic combination production?
India leads in manufacturing volume, producing about 35% of the world’s complex generics. The U.S. is catching up quickly, especially with new FDA incentives for domestic production. Europe lags in approvals but has strong research capabilities.
What’s the biggest threat to the future of generic combinations?
Pricing pressure and regulatory ambiguity. If regulators can’t clearly define what counts as a meaningful improvement, companies may flood the market with low-value “me-too” products. That could erode trust and trigger stricter rules-or price controls-that hurt innovation.










15 Comments
Wow, this is actually one of the most thoughtful pieces I've read on generics in years. 🙌 Finally someone gets that it's not about cheap pills anymore-it's about smart delivery. That Budeprion XL example? Perfect. I've seen patients switch from 3 pills to 1 and actually start taking them. Game changer.
Let’s be real-this is just pharma’s latest scam to keep prices high under the guise of ‘innovation.’ You call it ‘super generics,’ I call it ‘patent evergreening with extra steps.’ The FDA’s ‘pilot program’? A PR stunt to make Americans feel safe while they still import 90% of the API from China and India. 🤡
Interesting read. I work in supply chain for a mid-sized pharma co in the UK. The shift to complex combos is real-our lab just upgraded to hot-melt extruders last year. Cost? A fortune. But the margins? Worth it. Still, the regulatory mess between US and EU is insane. We had to build two separate lines for the same combo. 😩
So you’re saying if I can’t copy a pill exactly, it’s now ‘innovation’? That’s not innovation-that’s legal loophole exploitation. The whole point of generics is to be identical. Now we’re pretending that a slightly slower-releasing tablet is somehow ‘better’? Please. Patients don’t care about your particle size. They care about price.
Can we just take a moment to appreciate how incredible it is that we’re moving toward fewer pills, fewer injections, and better adherence? I’ve worked with elderly patients who forget to take 4 meds a day. One combo pill? Life-changing. This isn’t corporate greed-it’s human-centered design. 💙
Biggest red flag? The FDA’s approval lag for complex combos. 18-24 months longer? That’s a death sentence for startups. I’ve seen 3 small biotechs burn through $20M and still get rejected because their inhaler’s aerosol cloud didn’t match the brand’s ‘exact’ dispersion pattern. But the brand’s data was from 2012. The tech’s evolved. The regs haven’t. This isn’t science-it’s bureaucracy with a lab coat.
Man, I just read this on my lunch break and had to pause. I used to work in a pharmacy in Ohio. Patients would come in with 8 different bottles. One combo for BP, one for diabetes, one for cholesterol… then add the new one for depression. It was chaos. Now I see them with one pill and a smile. It’s not magic-it’s just smart. Keep pushing this.
Typical American overhype. ‘Super generics’? More like ‘overpriced generics with fancy packaging.’ India produces 35% of the world’s supply, and suddenly the U.S. wants to ‘localize’? Good luck competing with 10-cent pills made in Hyderabad. This isn’t innovation-it’s nationalism dressed up as policy. 🇺🇸💸
It’s funny how we treat drugs like they’re just chemistry. But they’re not. They’re behavior. A pill that’s easier to take isn’t just more convenient-it’s more humane. We’ve spent decades treating patients like data points. Now, for the first time, the system is being designed around the person who has to swallow it. That’s not just science. That’s ethics.
From a formulation standpoint, the real bottleneck isn’t the API-it’s the excipient compatibility matrix in multi-layered tablets. You need to balance hygroscopicity, crystallinity, and interfacial tension across 3+ layers while maintaining dissolution profiles within ±2%. Most CMOs don’t even have the HPLC-MS/MS to validate that. That’s why only 12 global players can do this at scale. The rest are just playing with LEGO.
As someone who works in Canadian regulatory affairs, I can confirm: EMA is moving at glacial speed. We approved 3 complex combos last year. The U.S. did 37. We’re not lagging because we’re cautious-we’re lagging because we’re underfunded. Our agency has 1/5 the staff of the FDA. And yes, we still use fax machines for some submissions. 😅
USA better not think they can out-produce India. We’ve been making generics since the 70s. You think your ‘pilot program’ will save you? HA. Your ‘domestic manufacturing’ is just a tax write-off for Big Pharma. India makes it cheaper, faster, and better. Don’t pretend otherwise.
Ok but who’s gonna pay for these ‘super generics’? Medicare won’t cover them. Medicaid won’t touch them. Private insurers will nickel-and-dime patients with $100 copays. So what? We just made a $20 pill into a $120 pill and called it ‘innovation’? This isn’t progress-it’s a con. 😭
As someone from India who’s seen the supply chain from both sides-yes, we make 35% of the volume, but the real innovation is happening in the U.S. and EU labs. The tech-nanoparticles, lipid systems, co-crystals-it’s not something you can replicate with a standard tablet press. It’s not about where it’s made. It’s about who understands the science. We’re catching up, but we’re not leading yet.
Just wanted to say thank you for writing this. My mom takes 7 pills a day. Last month, her doctor switched her to one combo. She cried. Not because it was expensive-because she finally felt like she could keep up. That’s the real win.