Rifampin Birth Control Risk Calculator
Calculate Your Risk Window
High-Risk Period
Your total high-risk period is 0 days.
Recommended Backup Methods
- Copper IUD: Gold standard - 99% effective, no liver interaction
- Condoms + spermicide: Best option if IUD not available
- Progestin implant (Nexplanon): May work but not fully proven
Critical Warning
DO NOT RELY ON:
- Hormonal birth control (pills, patch, ring)
- Withdrawal method
- Emergency contraception (Plan B)
These methods are ineffective during and after rifampin treatment.
When you're prescribed rifampin for tuberculosis or a stubborn staph infection, the last thing you might think about is your birth control. But here’s the hard truth: rifampin can make your oral contraceptive useless. Not less effective. Not slightly less. Rifampin can drop hormone levels so low that ovulation happens - and pregnancy becomes a real possibility.
How Rifampin Breaks Birth Control
Rifampin doesn’t just kill bacteria. It also tricks your liver into working overtime. It turns on enzymes - specifically CYP3A4 - that break down hormones faster than normal. That includes estrogen and progestin, the two key ingredients in most birth control pills. Studies show rifampin can slash ethinyl estradiol levels by up to 67% and progestin by over 50%. That’s not a minor drop. That’s enough to wipe out the hormonal barrier keeping you from ovulating. This isn’t theory. It’s been seen in real people. Women on rifampin have had breakthrough bleeding, spotting, and even full periods while still taking their pills. Some got pregnant. The first reports came in the 1970s, and since then, dozens of confirmed cases have been documented. No other antibiotic has this level of proof.Why Other Antibiotics Don’t Do This
You’ve probably heard warnings about antibiotics and birth control. Penicillin, amoxicillin, tetracycline, azithromycin - you name it. But here’s the catch: none of them have been shown to reduce hormone levels in controlled studies. There were 117 reports in the UK between 1970 and 1999 linking those antibiotics to birth control failure. But when researchers looked closer, they found no actual pharmacokinetic changes. No drop in hormone levels. No increase in ovulation. Just coincidence, misremembered periods, or missed pills. Rifampin is the exception. It’s the only antibiotic with clear, repeatable, and measurable evidence that it interferes with hormonal contraception. Even rifabutin - a similar drug used for MAC infections - has a weaker effect. It lowers hormone levels by about 20-30%, not 50-60%. So if you’re on rifabutin, you still need to be careful, but the risk isn’t nearly as high.How Long the Risk Lasts - Even After You Stop
Rifampin’s half-life is only 3 to 4 hours. But its effect on your liver enzymes? That lasts weeks. Enzyme induction peaks around day 7 of treatment. And once it’s turned on, it doesn’t flip off right away. Your liver keeps producing those extra enzymes for 2 to 4 weeks after your last pill. That means if you stop rifampin on Day 30, you’re still at risk for contraceptive failure until Day 58. The CDC and other major health bodies say you need backup contraception - not just for the time you’re on rifampin, but for a full 28 days after you finish. Skipping this window is one of the most common mistakes doctors and patients make.What Backup Contraception Actually Works
Not all backup methods are created equal. Condoms help, but they’re not foolproof. The best options are non-hormonal and don’t rely on your liver’s metabolism.- Copper IUD: This is the gold standard. It works locally in the uterus. No hormones. No liver interaction. It’s over 99% effective and lasts up to 10 years.
- Progestin implant (Nexplanon): Early data suggests it may hold up during rifampin use. A 2023 study of 47 women showed zero pregnancies while on rifampin and Nexplanon. The dose is higher than pills, and the hormone is released slowly - which might help it resist enzyme breakdown. But the sample size is small, so it’s not yet officially recommended as a standalone solution.
- Condoms + spermicide: If you can’t or won’t use an IUD, this is the next best option. Double protection is better than one.
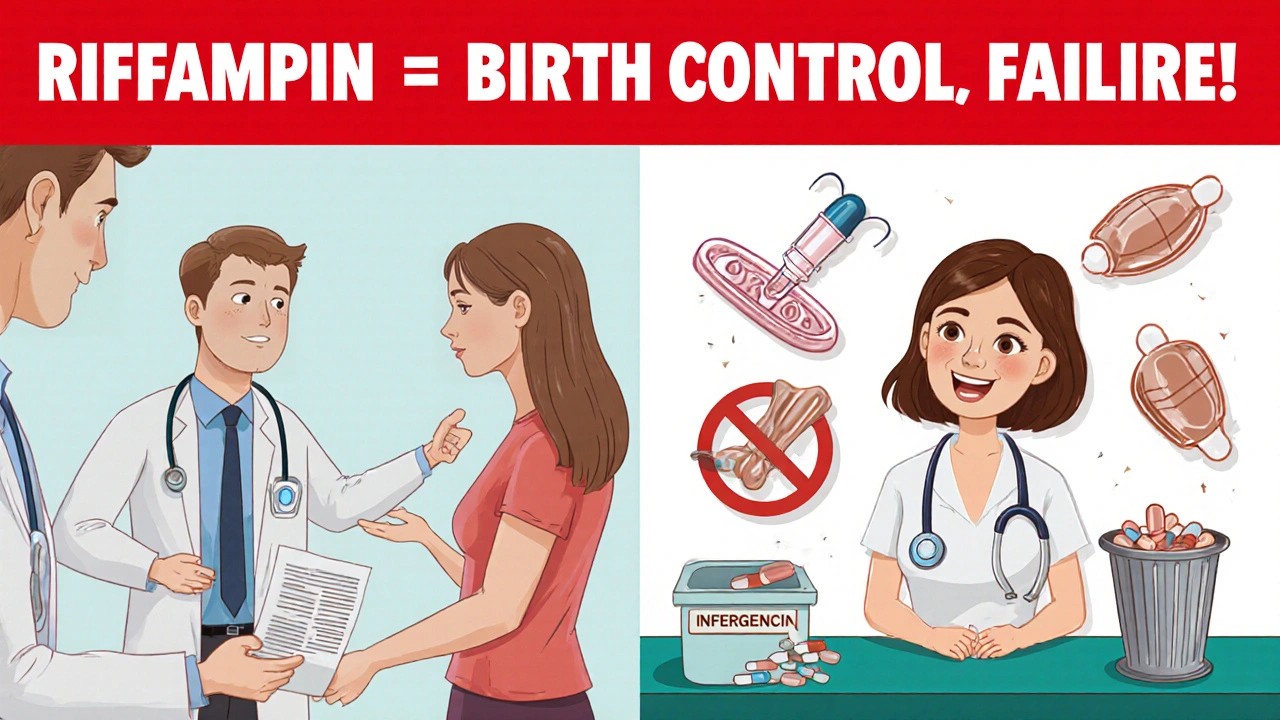
What Doesn’t Work
Don’t rely on these:- Other birth control pills: Switching brands or doses won’t help. All hormonal pills use the same estrogen and progestin compounds that rifampin breaks down.
- Withdrawal method: It’s unreliable even without drugs. Add rifampin? The risk skyrockets.
- Emergency contraception: Plan B and similar pills are metabolized by the same liver enzymes. Rifampin can make them less effective too. Don’t count on it as a safety net.
What Doctors Get Wrong
A 2017 survey found that only 42% of primary care doctors consistently warn patients about rifampin’s interaction with birth control. A shocking 28% told patients to use backup contraception for *all* antibiotics - which is unnecessary and causes confusion. Worse, many women aren’t told anything at all. A 2022 study in the Journal of Women’s Health found that 63% of women prescribed rifampin received no proper counseling on contraception. That’s not just a gap in care - it’s a public health risk. Doctors sometimes assume patients will read the pamphlet. Or they think the risk is too small to worry about. But when you’re talking about unintended pregnancy - especially in women with TB, who may already face high health risks - there’s no room for assumptions.What’s Changing in Treatment
The TB world is slowly moving away from rifampin. New regimens, like the 4-month high-dose rifapentine/moxifloxacin combo, are being tested as alternatives. If approved, they could reduce the number of women forced to choose between curing TB and preventing pregnancy. Meanwhile, manufacturers are now required to test every new hormonal contraceptive against rifampin before approval. The FDA and EMA demand it. That’s why newer pills, patches, and rings often have stronger warnings - but they’re still vulnerable. No hormonal method is safe with rifampin unless proven otherwise.
What You Should Do Right Now
If you’re prescribed rifampin:- Stop assuming your birth control is working.
- Ask your doctor: “Is this going to interfere with my birth control?” If they say no, push back. Cite the CDC guidelines.
- Get a copper IUD inserted before starting rifampin - or use condoms every time, every day, for the entire course plus 28 days after.
- Don’t wait for symptoms like spotting to realize something’s wrong. By then, it might be too late.
- If you’re on a progestin-only pill or implant, don’t assume you’re safe. The same rules apply.








12 Comments
I had no idea rifampin did this. I was on it for TB last year and just kept taking my pill. Thank god I didn’t get pregnant, but I’m so mad no one told me. My doctor just handed me a pamphlet and said 'read this.' Like, wow, thanks.
Oh here we go. Another fearmongering post about antibiotics. Next you’ll tell me coffee ruins birth control because it 'stresses the liver.' Wake up. The only thing that’s broken here is your ability to read a study. Rifampin? Fine. Everything else? No. Stop scaring people into IUDs like they’re some kind of holy grail.
I must emphasize, with the utmost seriousness, that this is not a trivial matter. The pharmacokinetic interference between rifampin and hormonal contraceptives is not speculative-it is empirically documented, peer-reviewed, and endorsed by the CDC. To ignore this is to endanger lives. Period.
I mean, I get that this is important, but like... why does everyone act like this is some new revelation? I’ve been on birth control since I was 17 and I’ve had like five different antibiotics over the years. I’ve never gotten pregnant. Ever. And now you’re telling me I need to go get a copper IUD because I took one pill for a sinus infection? I’m just saying... maybe some people are just fine? Maybe not everyone’s body is a lab experiment?
This is exactly why we need better public health education. I work in a clinic in rural Ohio, and half the women I see have never heard of enzyme induction. They think 'antibiotic' means 'birth control stops working'-and they’re terrified of every pill they take. Meanwhile, the ones who actually need the info? The ones on rifampin? They’re being handed a 2-page flyer in a 7-minute visit. We need systems, not just warnings. We need pharmacists to flag it. We need EHR alerts. We need to stop treating reproductive health like an afterthought.
So... you're saying my 2018 pregnancy wasn't because I missed a pill... but because I took amoxicillin for a toothache? Cool. I'll just add that to my 'Things I Regret' list next to 'trusting my ex' and 'eating that burrito'.
The data is unequivocal: rifampin induces CYP3A4, accelerating the hepatic metabolism of ethinyl estradiol and progestins, thereby reducing serum concentrations below the threshold required for ovulation suppression. This is not anecdotal; it is pharmacologically demonstrable. The 67% reduction in ethinyl estradiol levels, as cited in the 2005 study by the British Journal of Clinical Pharmacology, is corroborated by multiple independent cohorts. No other antibiotic exhibits this effect with such consistency.
Funny how we treat medical advice like a magic spell. Take this pill, and your body becomes a perfect machine. But then you take rifampin, and suddenly your hormones are like a toddler with a remote control-flipping channels at random. Maybe the real issue isn’t the drug. Maybe it’s that we’ve outsourced our bodies to chemistry and forgotten that biology doesn’t care about your schedule.
I’ve seen this so many times. Women come in after a surprise pregnancy, crying, saying ‘I didn’t know!’ And then we find out they were on rifampin for 6 weeks and never mentioned it. Why? Because they were too embarrassed. Because they thought their doctor ‘knew’ they were on birth control. Because they assumed the pill was ‘always’ working. This isn’t about science. It’s about communication failure. And it’s on the system. Not the patient.
I can’t believe this is even a debate. America is falling apart because we treat women’s health like a side note. You have women in rural India choosing between TB meds and their future. And here we are arguing about whether condoms are ‘enough.’ This isn’t about birth control. It’s about dignity. And if you don’t see that, you’re part of the problem.
Important note: While the copper IUD is the gold standard, it is not the only viable option. For patients who cannot or will not undergo insertion, barrier methods with spermicide (specifically nonoxynol-9) have demonstrated, in clinical trials, a failure rate of approximately 3-5% when used consistently and correctly. This is significantly lower than the 9% failure rate of oral contraceptives under typical use. Therefore, while IUDs are ideal, they are not the sole solution.
I’m glad this got posted. I’ve been telling my friends for years that rifampin is the one antibiotic you actually need to worry about. Everyone panics about amoxicillin, but if you’re on rifampin? You’re not just being careful-you’re being smart. And if your doctor doesn’t know this? Find a new one. Your body isn’t a guessing game.