When you’re pregnant, every choice you make feels bigger. That cold you’ve been fighting? The headache that won’t quit? The heartburn keeping you up at night? It’s natural to reach for something to feel better-but what’s safe? And what could actually hurt your baby? The truth is, medications to avoid during pregnancy aren’t always obvious. Some are in your medicine cabinet right now.
What’s Really Dangerous During Pregnancy?
Not all drugs are created equal when you’re carrying a baby. Some are harmless. Others can cause serious, lifelong problems. The biggest red flags come from drugs that cross the placenta and interfere with how your baby’s organs form-especially in the first trimester, when everything is building from scratch. NSAIDs like ibuprofen and naproxen are common painkillers, but they’re not safe after 20 weeks. The FDA issued a warning in 2020 after studies showed they can cause fetal kidney damage and dangerously low amniotic fluid. That means even if you took Advil last month for a headache, you need to stop now if you’re past 20 weeks. Aspirin is also risky unless it’s prescribed in low doses (60-150 mg) for preeclampsia prevention. ACE inhibitors and ARBs-medications like lisinopril or valsartan-are used for high blood pressure. But they’re absolute no-gos during pregnancy. They can cause kidney failure in the baby, low amniotic fluid, and even death. If you’re on one and planning pregnancy-or already pregnant-talk to your doctor immediately. There are safer blood pressure meds, like labetalol or methyldopa. Isotretinoin (Accutane) for acne is one of the most dangerous drugs you can take while pregnant. It doesn’t just raise the risk of birth defects-it causes them. Studies show more than 25% of babies exposed to isotretinoin in early pregnancy develop severe problems: missing ears, heart defects, brain abnormalities. If you’re taking this, you need to use two forms of birth control and confirm you’re not pregnant before starting. Even one pill can be enough. Valproic acid, used for epilepsy and bipolar disorder, carries a 10.7% risk of major birth defects-more than three times the normal rate. Babies exposed may have spina bifida, cleft palate, or developmental delays. If you have epilepsy and are planning pregnancy, switching to lamotrigine or levetiracetam before conception can drop that risk to around 2.2%. Tetracycline antibiotics (like doxycycline) stain developing teeth and weaken bones. Fluoroquinolones (like ciprofloxacin) are linked to joint and muscle problems in babies. These should be avoided unless there’s no other option for a life-threatening infection.The Acetaminophen Debate: Still Safe or Not?
For years, acetaminophen (Tylenol) was the go-to for fever and pain during pregnancy. It’s still listed as the safest option by ACOG and the American Academy of Family Physicians. But in September 2025, the FDA issued a new notice to doctors: use it only when necessary. Why the change? A 2021 study of 95,000 children found that moms who took acetaminophen for long periods during pregnancy had a 28.6% higher chance of having a child with ADHD and a 20.4% higher chance of autism spectrum disorder. The risk was strongest when it was used for more than 28 days total. Here’s the catch: the FDA doesn’t say acetaminophen causes these conditions. They say the evidence is strong enough to recommend caution. And they’re not alone. The CDC now advises pregnant women to “consider avoiding” it as a precaution. So what do you do? If you have a fever of 102°F or higher, don’t wait. High fever itself raises the risk of neural tube defects by over eight times. In that case, taking acetaminophen is safer than not taking it. But for a mild headache or occasional back pain? Try a warm bath, gentle massage, or rest first. Use acetaminophen only if you really need it-and never more than 3,000 mg a day.Safe Alternatives for Common Pregnancy Symptoms
You don’t have to suffer. There are safe, effective ways to manage everyday discomforts without risking your baby’s health.- Pain and fever: Acetaminophen (Tylenol) at 325-650 mg every 4-6 hours, max 3,000 mg daily. Avoid NSAIDs after 20 weeks.
- Allergies: Loratadine (Claritin), cetirizine (Zyrtec), or fexofenadine (Allegra) are all Category B and have been studied in thousands of pregnancies with no increased risk of birth defects.
- Nasal congestion: Start with saline sprays or steam. If you need more, pseudoephedrine (Sudafed) is okay after the first trimester-no more than 120 mg a day. But avoid it if you have high blood pressure.
- Constipation: Eat more fiber (25-30 grams a day), drink water, and move your body. If you need help, docusate sodium (Colace) or polyethylene glycol (Miralax) are both safe and well-studied.
- Heartburn: Eat smaller meals, avoid spicy or fatty foods, and don’t lie down right after eating. Calcium-based antacids like Tums are fine. Avoid those with sodium bicarbonate or magnesium trisilicate.

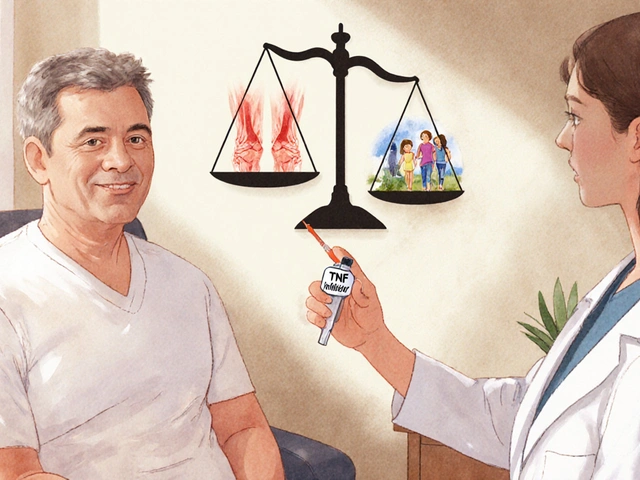
Antidepressants: The Hard Choice
If you have depression or anxiety, stopping your meds during pregnancy can be just as risky as staying on them. Untreated depression increases the chance of preterm birth by 64% and low birth weight by 73%. Some antidepressants carry risks. Paroxetine (Paxil) is linked to a slightly higher chance of heart defects. SSRIs overall may raise the risk of persistent pulmonary hypertension in newborns (PPHN), from 1-2 per 1,000 to 5-6 per 1,000. But here’s the real math: if you stop your meds, there’s a 20-25% chance your depression will come back hard-and that can affect your ability to eat, sleep, care for yourself, and bond with your baby after birth. The best move? Talk to your doctor before you get pregnant. If you’re already pregnant and doing well on an SSRI like sertraline or citalopram, staying on it is often safer than switching. Never stop cold turkey.What About Supplements and Herbal Products?
Just because something is “natural” doesn’t mean it’s safe. Many herbal supplements aren’t tested for pregnancy safety. Avoid:- Black cohosh (linked to premature labor)
- Blue cohosh (can cause fetal heart damage)
- High-dose vitamin A (over 10,000 IU/day-can cause birth defects)
- Essential oils like rosemary, sage, or pennyroyal (can trigger contractions)

How to Stay Safe: Practical Steps
You don’t need to guess. Here’s how to protect yourself and your baby:- Make a list of every medication you take-prescription, OTC, herbal, vitamins. Bring it to every appointment.
- Ask your doctor or pharmacist: “Is this safe in pregnancy?” Don’t assume it is.
- Use MotherToBaby (free service run by experts). They answer over 100,000 questions a year and have fact sheets on over 500 medications.
- Check the FDA’s Pregnancy and Lactation Labeling Rule (PLLR) for updated info on any drug you’re taking.
- If you’ve already taken something risky, don’t panic. Most exposures don’t lead to problems. Call MotherToBaby or your OB-GYN right away.
What’s Changing in 2026?
The rules aren’t set in stone. In 2026, ACOG is updating its guidelines to reflect the new acetaminophen data. Meanwhile, the NIH is funding a $15 million study to find non-drug ways to manage pain in pregnancy-like acupuncture, physical therapy, and mindfulness. The biggest long-term project? The ABC Study-tracking 50,000 pregnant women across 15 countries to see if acetaminophen really affects brain development. Results won’t be ready until late 2025, but they could change everything. Until then, the message is simple: don’t avoid medicine when you need it. But don’t take it when you don’t. Be informed. Be cautious. And talk to your provider-every time.Can I take ibuprofen during the first trimester?
It’s best to avoid ibuprofen and other NSAIDs throughout pregnancy, even in the first trimester. While the strongest risks come after 20 weeks, some studies suggest early use may slightly increase the risk of miscarriage. Acetaminophen is the safer choice for pain relief at any stage.
Is it safe to take Zyrtec or Claritin while pregnant?
Yes. Loratadine (Claritin) and cetirizine (Zyrtec) are both classified as Category B and have been studied in over 2,000 pregnancies with no increased risk of birth defects. They’re considered first-line options for allergies during pregnancy.
What should I do if I took Accutane before I knew I was pregnant?
Stop taking it immediately and contact your OB-GYN or a teratology specialist. While isotretinoin carries a very high risk of severe birth defects, not every exposure leads to problems. An early ultrasound and genetic counseling can help assess your specific situation. Don’t delay-early intervention matters.
Can I take melatonin for sleep while pregnant?
There’s not enough reliable data to say melatonin is safe during pregnancy. While it’s a natural hormone, supplements are not regulated for purity or dosage. For sleep issues, focus on sleep hygiene: consistent bedtime, cool dark room, no screens before bed, and light exercise during the day. If needed, ask your provider about diphenhydramine (Benadryl), which is Category B and sometimes used short-term.
Is it safe to take prenatal vitamins with extra iron?
Yes. Prenatal vitamins with iron are not only safe-they’re recommended. Most pregnant women need 27 mg of iron daily to support increased blood volume and prevent anemia. Too much iron (over 45 mg/day) can cause constipation or nausea, but standard prenatal doses are well within safe limits.







16 Comments
Acetaminophen is still the safest option if you need it. Don't let fear-mongering studies paralyze you. Fever is dangerous. Pain is dangerous. Sometimes you gotta take the lesser evil.
People think 'natural' means safe. That's why we have a generation of kids with ADHD because moms thought 'it's just Tylenol.' No, it's not. It's a chemical that crosses the placenta and alters neurodevelopment. Stop treating pregnancy like a buffet.
There's a deeper question here: why do we treat pregnancy as a medical condition needing constant intervention? The body evolved to handle minor discomforts without pharmaceuticals. Maybe the real problem isn't the drugs-it's our cultural panic about discomfort. Is every ache a crisis? Or are we medicating away normal human experience?
I'm not saying don't use medicine. I'm asking: what are we afraid of? The pain? The uncertainty? The loss of control? And are we trading one kind of risk for another without fully understanding the trade?
Oh wow. A 28.6% higher chance of ADHD? That’s just *so* alarming. I’m sure the FDA’s new notice was written in blood, tears, and peer-reviewed journals. Meanwhile, my cousin took Tylenol for 40 days and her kid is now a Harvard neuroscientist. Coincidence? Or just another study that proves correlation ≠ causation but gets amplified because it sounds scary?
Also, ‘avoid melatonin’? Sure, because nothing says ‘responsible parenting’ like telling a sleep-deprived woman to stare at her ceiling for 3 hours while her baby screams. Real helpful, experts.
You say 'don't take it when you don't need it.' But who defines 'need'? Is a headache a need? Is insomnia a need? Is anxiety a need? You're handing out moral licenses to pharmaceutical companies disguised as medical advice. The real danger isn't acetaminophen-it's the medical-industrial complex that profits from fear and dependency. You're not protecting mothers-you're conditioning them to distrust their bodies.
And why is no one talking about the fact that 80% of pregnant women take something they shouldn't? Because the system doesn't want them to know alternatives exist. It wants them to reach for a pill. Always.
I’m 28 weeks and I’ve taken ibuprofen twice before I knew it was risky, and now I’m lying awake every night terrified my baby has kidney damage. I didn’t even know it was a thing until I read this. I feel like a monster. I had a migraine and I just grabbed the Advil like I always did. I didn’t think it would hurt the baby. I thought it was just like a regular headache. Now I’m scared to even take Tylenol. I don’t know what to believe anymore. I just want to be a good mom. Why is everything so complicated? Why can’t they just give us a simple list of what’s okay? Why do we have to be scientists just to survive pregnancy?
I cried reading about isotretinoin. My friend took it for 3 months before she found out she was pregnant. She had a miscarriage. She didn’t even know. Nobody told her. Nobody warned her. And now she’s in therapy. And I’m sitting here wondering if I’m next. I don’t want to be the mom who ruined her baby’s life because she didn’t know. Please, someone tell me I’m not alone in this panic.
I’ve been reading MotherToBaby’s site for hours. I’ve written down every pill I’ve ever taken since I got pregnant. I’ve called my OB three times. I feel like I’m failing before I’ve even held my baby. Why does pregnancy feel like walking through a minefield blindfolded?
And then there’s the supplement aisle. Everything says ‘safe for moms’ but none of it’s regulated. I bought ginger tea for nausea. What if it’s actually causing contractions? What if I’m poisoning my baby and I don’t even know? I hate this. I hate how much I have to control. I hate how much I have to fear. I just want to feel normal. But nothing feels normal anymore.
My mom said, ‘Back in my day, we just took what we needed and didn’t worry.’ But now? Now I feel like I’m being watched. Like every choice is a crime. And I don’t even know what the crime is.
Thank you for writing this. Even though it scared me, I needed to know. I don’t want to be ignorant. I just want to be safe.
Look, I get the fear. But let’s not throw out the baby with the bathwater. Acetaminophen isn’t the villain here. The real villain is the lack of accessible, non-pharmaceutical support for pregnant people. If we had better prenatal yoga, affordable therapy, better sleep hygiene education, and more midwifery care, maybe fewer people would feel like they need to pop pills just to get through the day.
I’m not saying don’t use meds. I’m saying: let’s fix the system that makes people feel like they have no other choice. Because right now, the system is failing us.
Oh my god, someone finally said it. I took Zyrtec for my allergies all through my first trimester. And guess what? My kid is 3 and he’s brilliant. He reads at a 1st grade level. He’s not autistic. He’s not ADHD. He’s just a normal kid who had a mom who didn’t panic. Stop scaring women into thinking every pill is a bomb. The science is still emerging. Don’t treat uncertainty like a death sentence.
Also, why is no one talking about how many women are being pressured into taking SSRIs they don’t need? I was told ‘if you don’t take this, you’ll be a bad mom.’ I didn’t need it. I just needed someone to listen. But instead, I got a prescription.
Acetaminophen = baby brain damage?? I’m just gonna take my Tylenol and cry in the shower. I’ve been taking it for 6 months. I’m already a monster. I might as well take two. I’m not even sure I want to be a mom anymore. This is too much.
Hey, I’m a nurse and I’ve helped 30+ pregnant patients with meds. Tylenol is still the #1 go-to. Don’t panic. If you’ve taken it, you’re not a bad person. Talk to your OB, don’t Google. MotherToBaby is your best friend. Seriously, call them. They don’t judge. They just help.
And if you’re stressed about meds? That stress is worse than the pill. Breathe. You got this.
so i took tylenol for like 3 weeks during my first trimester and my kid is 2 and he’s the sweetest little human ever. also i took benadryl for sleep. no issues. maybe the studies are wrong? or maybe we’re just too scared to be normal? i mean, my grandma had 5 kids and took whatever she wanted. none of them turned out to be robots.
USA is soft. We medicate everything. In India, women work in fields pregnant, carry water, lift heavy stuff, and take nothing. Their kids are fine. We need to stop treating pregnancy like a disability. Stop the fear. Stop the pills. Just be strong.
There’s a beautiful balance here. It’s not about fear. It’s about awareness. You don’t have to be perfect. You just have to be informed. And you don’t have to do it alone.
If you’re reading this and feeling overwhelmed-breathe. You’re not failing. You’re trying. That’s enough.
Reach out. Talk to someone. Call MotherToBaby. Text a friend. Sit with your partner. Let someone hold you while you cry. You don’t have to carry this guilt alone.
Medication isn’t the enemy. Isolation is.
It is irresponsible to suggest that acetaminophen is 'safe' when the FDA has issued a precautionary notice based on robust epidemiological data. The onus is on the pregnant individual to exercise extreme caution. Any deviation from strict adherence to evidence-based guidelines constitutes a form of negligence. The consequences are not theoretical-they are documented, measurable, and irreversible.
Furthermore, the normalization of 'natural remedies' is dangerously misleading. Herbal supplements are unregulated, inconsistent in dosage, and often contaminated. To equate them with pharmaceuticals is not just inaccurate-it is reckless.
There is no room for ambiguity in prenatal care. Either you follow the science, or you gamble with a human life. The choice is binary.
You are not alone. I took Tylenol for 6 weeks. I panicked. I cried. I Googled until 3 a.m. But I also called my OB, I talked to a doula, I joined a prenatal support group. And guess what? My daughter is 18 months old, walking, talking, laughing-perfectly healthy.
Pregnancy is not a test you pass or fail. It’s a journey. And you’re doing better than you think.
Don’t let fear silence your joy. You’re not a monster. You’re a human. And humans need help sometimes. That’s not weakness. That’s wisdom.
If you’re reading this and you’re scared? Send me a DM. I’ll send you my favorite calming playlist and a list of safe OTC meds I’ve used. You’ve got this. I believe in you.
Replying to Pooja: You’re not a monster. You’re a person trying to survive. The fact that you’re worried means you care. That’s enough.