When a life-saving medication disappears from the pharmacy shelf, patients don’t just lose a pill-they lose stability, trust, and sometimes hope. Drug shortages aren’t rare glitches anymore. In 2023, nearly 300 medications were in short supply across the U.S., from heart pills to cancer drugs. And when this happens, the burden doesn’t fall on the manufacturer or the wholesaler. It falls on the provider-the doctor, nurse, or pharmacist who sits across from the patient and says, "I’m sorry, we don’t have your medication." That moment can break trust faster than any mistake in diagnosis. So what’s the right way to handle it?
Communication isn’t optional-it’s a duty
The Joint Commission now lists poor communication during drug shortages as a leading cause of sentinel events. That’s their term for serious, preventable harm. And it’s not because providers are careless. It’s because most haven’t been trained to do this well. A 15-minute visit isn’t enough to explain why your blood pressure med is gone, what the alternative does, how it might make you feel, and when the original might come back. But skipping any of that? That’s negligence.Providers have a legal and ethical responsibility to communicate clearly, early, and honestly. The FDA’s 2012 law requires manufacturers to report potential shortages six months in advance. That’s not a suggestion. It’s a trigger. If you know a drug is running low, you have a duty to prepare your patients before they show up for their refill and get turned away.
What good communication looks like
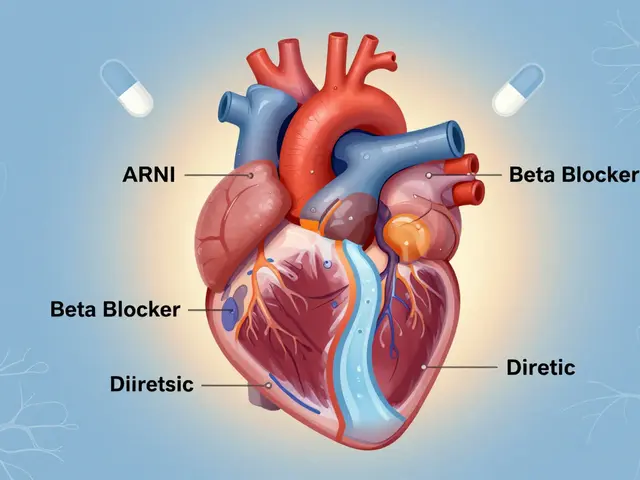
There’s a difference between telling a patient, “We don’t have your pill,” and telling them, “Your usual blood pressure medicine, lisinopril 10mg, is currently in short supply. We’ve chosen valsartan 80mg instead because studies show it works just as well for most people like you. It might cause a dry cough in about 1 in 10 people, but that usually goes away. We expect lisinopril to be back in 6-8 weeks. Here’s a printed sheet with both names, doses, and what to watch for. Call this number if you feel dizzy or your swelling gets worse.”That’s the standard. The European Medicines Agency calls it the “Five Essentials” for shortage communication:
- Identify the drug-brand name, generic name, strength, form (tablet, injection, etc.)
- Explain the shortage-how much is missing, how long it’s expected to last
- Offer alternatives-with clinical reasoning, not just a prescription swap
- Give a timeline-even an estimate helps reduce panic
- Provide contact info-so patients know who to call if things go wrong
And here’s the kicker: all of this must be written at a 6th- to 8th-grade reading level. No “therapeutic substitution,” no “pharmacokinetic profile.” Just: “This medicine helps lower your blood pressure. The new one works the same way.”
Why patients stay silent-and how to fix it
A study in JAMA Internal Medicine found that patients with limited English skills are 3.2 times more likely to misunderstand a shortage notice. But even English-fluent patients often don’t ask questions. Why? Because they’re scared. They think if they challenge their doctor, they’ll be seen as difficult. Or they assume the provider knows best-and they shouldn’t question it.That’s why “teach-back” matters. Don’t just say, “Do you understand?” Ask: “Can you tell me in your own words how you’ll take this new pill?” If they say, “I take it when my head hurts,” you know they didn’t get it. Then you fix it. Right then.
One clinic in Minnesota started using a simple script: “I know this change might feel unsettling. What worries you most about switching?” That one question opened up conversations that led to 40% fewer missed doses and 60% fewer emergency visits during shortages.

What happens when you don’t communicate
Patients aren’t just annoyed-they’re scared. On Reddit, one user wrote: “My heart medication disappeared. My doctor handed me a new pill. No explanation. I didn’t know if it was stronger, weaker, or if it would kill me. I stopped taking it for three days.” That’s not an outlier. On Healthgrades, reviews mentioning drug shortages average just 2.1 stars. The top complaints? “No warning.” “No explanation.” “I felt like a lab rat.”Meanwhile, clinics that use structured protocols-like Mayo Clinic’s SHIP system-see 87% patient satisfaction. Why? Because patients feel seen. They know what’s happening. They’re not guessing. And they trust the person who told them the truth, even if the news was bad.
Real barriers-and how to overcome them
Let’s be honest: most clinics aren’t set up for this. The average doctor visit is 15.7 minutes. EHR systems? Only 38% flag drug shortages automatically. Rural clinics? 68% don’t get real-time updates. And training? Most providers get zero formal instruction on how to talk about shortages.But solutions exist. Kaiser Permanente built shortage alerts into their routine visit workflow. Instead of adding time, they saved it-cutting extra communication time to just 2.7 minutes per patient. Intermountain Healthcare created an EHR template that auto-fills shortage details, so the provider just checks a box and it’s done. Memorial Sloan Kettering assigned trained communication specialists to handle all cancer drug shortage talks. That way, oncologists focus on treatment, and patients get the emotional support they need.
Costs? Around $12,500 per facility to set up a system. But the cost of not doing it? Higher readmissions, lawsuits, lost trust, and patients who stop taking their meds altogether. One study found that 28% fewer prescribing errors happened when providers used clear communication protocols.

The new rules are coming
Starting January 2025, the Joint Commission will require all accredited facilities to have structured, empathetic communication plans for drug shortages-or risk losing accreditation. The FDA’s new Drug Shortage Communication Collaborative now requires manufacturers to provide ready-to-use patient materials within 24 hours of a shortage declaration. And the WHO is pushing for global standards.What does this mean for you? If you’re a provider, you’re not just a prescriber anymore. You’re a communicator, a counselor, and a crisis manager. You need to know which drugs are at risk, how to explain alternatives without jargon, and how to listen when patients are scared.
And if you’re a patient? Ask. Say: “I’m worried about this switch. Can you explain why you chose this one?” If they can’t answer clearly, ask for a second opinion. Your health depends on it.
What you can do today
You don’t need a fancy system to start doing this right. Here’s a simple checklist:- Check your pharmacy’s shortage alerts weekly-sign up for FDA or ASHP updates.
- When a shortage hits, notify patients before they come in for a refill.
- Use plain language: no medical terms unless you explain them.
- Always use teach-back: “Can you tell me how you’ll take this?”
- Document what you said, how they responded, and what they understood.
- Offer a phone number or email for follow-up questions.
It’s not about being perfect. It’s about being present. When a drug vanishes, the one thing patients can still count on is you. Don’t let them down.