Every day, pharmacy technicians handle thousands of prescriptions. Most of them-over 90%-are for generic drugs. But knowing the difference between metoprolol and Toprol-XL, or spotting a mix-up between glipizide and glyburide, isn’t just helpful. It’s life-or-death. Generic drug competency isn’t a nice-to-have skill. It’s the foundation of safe pharmacy practice.
Why Generic Drug Knowledge Is Non-Negotiable
Generic medications save the U.S. healthcare system over $300 billion a year. But they also create a hidden risk: confusion. A 2021 study by the Institute for Safe Medication Practices found that 10-15% of medication errors linked to death involved brand-name and generic drug mix-ups. That’s not rare. That’s routine.
Technicians who can’t quickly identify that atorvastatin is the generic for Lipitor, or that hydrochlorothiazide is a diuretic, can accidentally dispense the wrong dose, the wrong form, or the wrong drug entirely. In one case, a technician confused hydroxyzine (an antihistamine) with hydralazine (a blood pressure drug). The patient suffered a stroke. The error was caught-barely-because the pharmacist noticed the wrong color tablet.
The stakes are high. The FDA reports that over 127 serious adverse events in 2023 were tied directly to generic drug misidentification. And it’s not just hospitals. Community pharmacies, where most prescriptions are filled, see the highest volume of generic drugs-and the highest risk of human error.
What the Standards Actually Require
There’s no single national rule, but most certification bodies agree on the basics. The Pharmacy Technician Certification Board (PTCB) requires technicians to know at least 200 of the most commonly prescribed drugs by both generic and brand name. That’s not a suggestion. It’s part of the Certified Pharmacy Technician (CPhT) exam, which now dedicates 18% of its content to this area as of 2026.
The VA’s standards are even stricter. Pharmacy technicians working in Veterans Affairs facilities must identify 100% of Schedule II-V controlled substances by name-no exceptions. They also need to understand therapeutic equivalence, dosage forms, and how generics are substituted under state law.
Here’s what you’re expected to know:
- Generic and brand names of the top 200 drugs
- Drug classifications (e.g., beta-blockers, SSRIs, statins)
- Common strengths and dosage forms (tablet, capsule, liquid)
- Therapeutic duplication risks (e.g., taking two drugs with the same active ingredient)
- High-alert medications (insulin, anticoagulants, opioids)
It’s not enough to memorize a list. You need to understand why a drug belongs to a class. Why is lisinopril an ACE inhibitor? Why does metformin carry a black box warning? That context helps you catch mistakes before they happen.
How Training Programs Are Adapting
Most pharmacy technician programs now include 40-60 hours of dedicated drug identification training. But not all methods work. Rote memorization fails. Flashcards alone won’t cut it when you’re dealing with 15-20 new generic drugs entering the market every month.
Top programs use three proven strategies:
- Group by therapeutic class-Learn all beta-blockers together: metoprolol, atenolol, propranolol. Understand their shared purpose and side effects.
- Use visual cues-Many technicians swear by imprint, color, and shape. A white, round tablet with “50” on one side? That’s likely 50 mg metoprolol. A blue, oval pill with “20” and “E” on it? That’s esomeprazole.
- Practice with real prescriptions-Simulated pharmacy workflows where technicians match generics to brand names in a live dispensing environment boost retention by 60%.
Walmart and CVS have started using AI-powered training tools that adapt to each technician’s weak spots. One system noticed a trainee kept confusing glimepiride with glipizide. It flagged that pair, ran a quiz, and showed side-by-side images of the pills. Within two weeks, the error rate dropped by 80%.

Where the System Still Falls Short
Not all states require the same knowledge. California asks technicians to know 180 drugs. Texas only requires 120. That creates a mess for technicians who move across state lines. One technician in Florida passed her exam with 120 drugs. Three months later, she got hired in New York-and failed her first competency check because she didn’t know ranitidine (Zantac) was discontinued and replaced with famotidine.
Even worse, drug names change. A generic made by Teva might become a generic made by Mylan, and the pill’s imprint changes. A technician trained on last year’s version can be caught off guard.
And while hospitals have quarterly competency checks, 43% of independent pharmacies still use outdated pocket guides updated only once a year. That’s like driving with a 2018 map in a city that rebuilt half its roads.
What Success Looks Like
Pharmacy teams that prioritize generic drug competency see real results. A 2023 National Community Pharmacists Association study found that technicians scoring 90% or higher on generic drug tests reduced dispensing errors by 22%. In one Oregon clinic, after implementing weekly 15-minute drug quizzes, error rates dropped from 1 in 150 prescriptions to 1 in 800.
One technician, who’d failed the PTCB exam twice, turned things around by using the RxTechExam “Top 100 Drugs” guide. She grouped drugs by condition: diabetes, hypertension, depression. She made flashcards with pill images. She practiced with her pharmacist every morning before shift. She passed on her third try with a 94% score on the generic drug section.
Her secret? “I stopped trying to memorize. I started trying to understand.”

The Future: Beyond Memorization
The next wave of competency standards won’t just ask, “What’s the generic for X?” They’ll ask, “Why does this patient need this generic instead of that one?”
Starting in 2025, the VA and ASHP began including biosimilars in training. These are complex, biologic drugs-like adalimumab and its biosimilars-that look nothing like traditional generics. They require deeper understanding of manufacturing, immunogenicity, and substitution rules.
By 2030, experts predict pharmacy technicians will need to understand pharmacogenomics-how a patient’s genes affect how they respond to a generic drug. A generic statin might work perfectly for one person but cause muscle pain in another due to a genetic variant. Technicians won’t just be dispensers. They’ll be frontline safety monitors.
For now, the focus is on building a solid base. If you’re training to be a pharmacy technician, don’t treat generic drug knowledge as a test topic. Treat it like your first aid kit. You hope you never need it. But if you do, you better know exactly where everything is.
How to Build Your Own Generic Drug Mastery Plan
Start small. Pick one drug class. Learn five drugs in that class. Know their brand names, uses, and common side effects. Then move to the next. Use free tools like the PTCB’s official study guide or the FDA’s Orange Book to check for updates.
Set a weekly goal: “This week, I’ll master all beta-blockers.” Test yourself every Friday. Quiz a coworker. Use an app that shows pill images. Don’t just read-engage.
And remember: the goal isn’t to know every drug. It’s to know enough to stop a mistake before it happens.
What percentage of prescriptions in the U.S. are generic drugs?
Over 90% of prescriptions dispensed in the United States are for generic drugs, according to FDA data from 2022. This number has remained steady for the past five years, with generics saving the healthcare system over $300 billion annually.
How many drugs must a pharmacy technician know for certification?
The PTCB certification exam requires mastery of at least 200 commonly prescribed medications, including both generic and brand names. Some state boards and employers may require knowledge of fewer drugs, but 200 is the industry standard for safe practice.
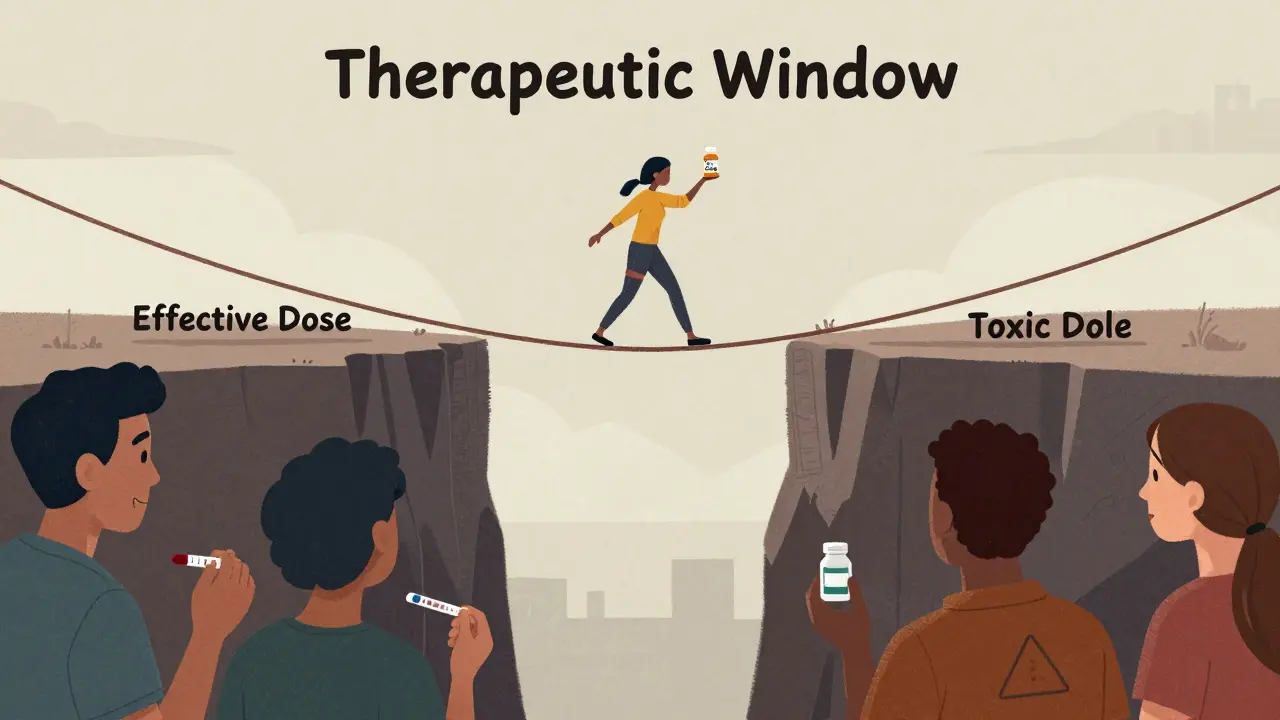
Are generic drugs always interchangeable with brand names?
Most generics are therapeutically equivalent to brand-name drugs and can be substituted unless the prescriber writes “Dispense as Written” or “Do Not Substitute.” However, some drugs-like anticonvulsants or thyroid medications-have narrow therapeutic windows, meaning even small differences in formulation can affect patient outcomes. Technicians must know when substitution is safe and when it’s not.
What are high-alert medications, and why do they matter?
High-alert medications-such as insulin, heparin, opioids, and anticoagulants-carry a higher risk of serious harm if misused. Even small errors with these drugs can be fatal. Pharmacy technicians must know the generic and brand names of these drugs with 100% accuracy and understand their unique dosing, administration, and monitoring requirements.
How often do generic drug names change?
New generic drugs enter the market at a rate of 15-20 per month, according to the FDA Orange Book (March 2025). Additionally, manufacturers may change pill imprints, colors, or packaging, making previously familiar drugs look different. Technicians must regularly check updated references and stay alert to these changes.
Can technology replace the need for generic drug knowledge?
No. Barcode scanning and automated systems help reduce errors, but they can fail-due to damaged labels, mis-scans, or system outages. Technicians must still recognize drugs visually and by name to catch these errors. Technology supports, but doesn’t replace, human knowledge.
What to Do Next
If you’re a pharmacy technician, start today. Pick five drugs you’re unsure about. Look them up. Write down their brand names, uses, and appearances. Test yourself tomorrow. Repeat.
If you’re training others, don’t just hand out lists. Use real pills. Show the differences. Let them handle the packaging. Make them explain why a substitution is safe-or why it’s not.
Generic drug competency isn’t about passing a test. It’s about protecting someone’s life. And that’s worth every hour you spend learning it.









10 Comments
Okay but let’s be real-how many techs actually *know* that hydralazine is a vasodilator and not an antihistamine until someone’s already in the ER? I’ve seen techs stare at a bottle like it’s hieroglyphics. And don’t get me started on the pill color chaos-last week I caught a 50mg metoprolol that looked like a damn M&M because the manufacturer switched imprints. FDA doesn’t even regulate pill aesthetics. We’re literally gambling with lives based on what shade of blue a tablet is.
My cousin was a tech in Texas. She passed with 120 drugs. Moved to New York. Got fired in 3 weeks because she didn’t know ranitidine was gone. No one told her. No one trained her. This isn’t about memorizing lists. It’s about systems failing people. We need mandatory cross-state competency checks. Not optional. Not ‘recommended.’ Mandatory. Lives are on the line.
bro why do we even care about generics anymore? like… isnt AI gonna do all this for us? i mean my phone can recognize a pill by taking a pic. why should i waste my brain on metoprolol vs toprol-xl? its 2025. let the robots do the boring stuff. also i think the FDA is just trying to make us memorize more so they can sell more textbooks lol
Hey, I’ve been training new techs for 8 years. The ones who crush it? They don’t memorize. They connect. They ask: ‘Why is this drug in this class?’ ‘What happens if we mix it with that?’ I had one girl who made a Spotify playlist with drug names as beats-‘Statins on the Low,’ ‘SSRIs in the Rain’-and she aced her exam with 97%. It’s not about rote. It’s about making it stick. You got this.
Let me guess-this whole ‘generic drug competency’ push is just Big Pharma’s way of keeping the generic manufacturers from undercutting them further. The FDA’s ‘127 adverse events’? Probably cherry-picked. And don’t even get me started on the ‘therapeutic equivalence’ myth. Ever heard of bioequivalence gaps? No? That’s because they don’t want you to know. The real danger isn’t misidentification-it’s the fact that generics aren’t *actually* identical. They’re just cheaper.
lol why are we even doing this? in india we just give the pill and say ‘take it’ no one cares about brand or generic. also i think all this ‘pill color’ stuff is fake. my uncle works in a pharmacy and he says 90% of the time the patient doesn’t even know what they’re taking. why are we overcomplicating? also i saw a video on tiktok that said all these drug names are just made up by pharma to confuse us. 🤡
Just got my CPhT last month. Used the RxTechExam guide. Grouped by condition: hypertension = ACEi, ARBs, beta-blockers. Made flashcards with pill pics from the FDA database. Practiced with my pharmacist every morning before shift. Passed with 94% on generics. It’s not magic. It’s method. You don’t need to know all 200 at once. Just 5 a week. One day, you’ll catch a mistake before it happens. And that? That’s why we do this. 💪💊
Okay, so we’re telling techs to memorize 200 drugs… but in 2025, we’re letting unlicensed foreign workers-some who can barely speak English-fill scripts in 17 states? And we’re not even requiring English proficiency tests? This isn’t about competency. It’s about cheap labor. And now we’re gonna blame the tech when someone dies because they confused glipizide with glimepiride? Yeah, right. Fix the system. Not the people.
You guys are missing the point. The real issue isn’t the 200 drugs. It’s that 70% of pharmacy techs are paid $15/hour and have zero continuing education. No one cares if they know metoprolol from atenolol when their manager just wants them to fill 60 scripts an hour. You can’t train competence into a system designed to burn people out. Fix the pay. Fix the hours. Then worry about pill colors.
As an Aussie who’s trained techs in both Sydney and Phoenix-I can tell you this: the U.S. is miles ahead in structured competency. Down here, we still use paper drug lists from 2010. No visual aids. No AI. No quizzes. You learn by osmosis… or you get fired. Your system’s flawed, sure-but at least you’re trying. Keep pushing. The future’s not just knowing the drug. It’s knowing the patient behind it. And that’s where real safety begins.