When someone has struggled with obesity and type 2 diabetes for years, medication alone often feels like fighting a losing battle. Insulin shots, pills, strict diets, and endless monitoring don’t always bring relief. That’s where metabolic surgery comes in-not as a quick fix, but as a powerful tool that changes how the body handles food, hormones, and blood sugar. The results? Many patients lose a huge amount of weight and, surprisingly, their diabetes disappears-sometimes within days.
What Metabolic Surgery Actually Does
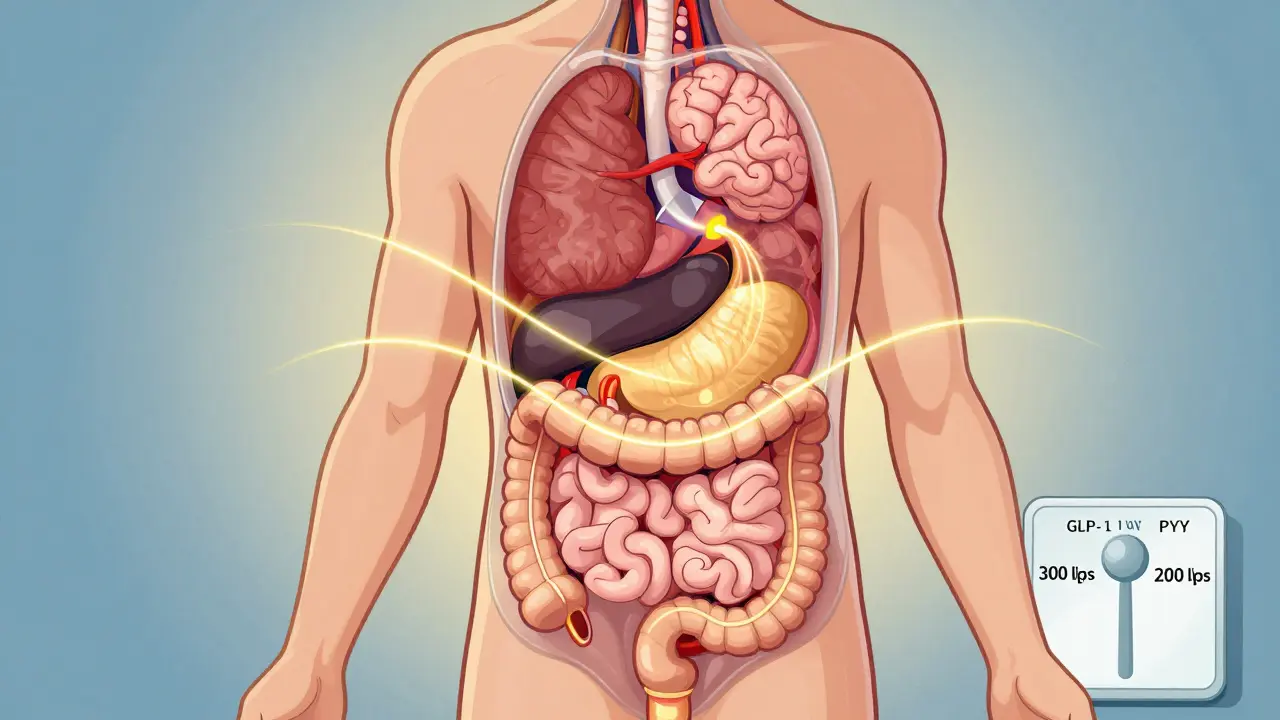
Metabolic surgery isn’t just about shrinking your stomach. It’s about rewiring your body’s metabolism. Procedures like gastric bypass, sleeve gastrectomy, and duodenal switch don’t just limit how much you can eat-they change the signals between your gut and your pancreas. This triggers a cascade of hormonal changes that improve insulin sensitivity almost immediately, often before you’ve lost much weight at all.
For example, after a Roux-en-Y gastric bypass, levels of GLP-1 and PYY-hormones that help control blood sugar and appetite-spike within hours. That’s why many patients stop needing insulin within days. It’s not magic. It’s biology. The gut starts communicating differently with the rest of the body, and that changes everything.
How Much Weight Do People Actually Lose?
Numbers matter here. Studies show patients who undergo metabolic surgery lose an average of 27.7% of their total body weight. Compare that to medical treatment alone, where patients typically lose less than 0.2%. That’s not a small difference-it’s life-changing.
Take gastric bypass patients with a starting BMI of 45.9. Six years later, they’d lost nearly 20% of their body weight. Sleeve gastrectomy patients lost about the same over five years. Even more impressive: those who had biliopancreatic diversion with duodenal switch lost over 60% of their excess weight on average. These aren’t outliers. These are consistent results across thousands of patients tracked for over a decade.
Diabetes Remission: The Real Win
The biggest surprise? Many people with type 2 diabetes go into remission. Not just better control-complete remission. No pills. No insulin. Normal blood sugar levels.
One of the most trusted studies, the Swedish Obese Subjects trial, followed patients for 15 years. Of those who had surgery, 30.4% still had their diabetes in remission. Only 6.5% of those who didn’t have surgery did. That’s nearly five times higher.
Breakdown by procedure:
- Gastric bypass: 42% remission at one year, 29% at five years
- Sleeve gastrectomy: 37% at one year, 23% at five years
- Duodenal switch: up to 95% remission at one year
Even more telling: patients with a BMI under 35-who are often told they’re not “severe enough” for surgery-still saw 36% complete remission after five years. In contrast, those treated only with medication had just 1.2% remission.

Who Benefits the Most?
Not everyone responds the same way. The best candidates share a few key traits:
- Not yet on insulin
- Diagnosed with diabetes within the last 10 years
- BMI over 30, but especially over 35
- Still producing some of their own insulin
Patients who haven’t started insulin have a 53.8% chance of remission 14 months after surgery. Those already on insulin? Much lower. Why? Because insulin use often means the pancreas has already lost a lot of its ability to make insulin. Surgery can’t bring back dead cells.
Age matters too. Younger patients tend to have better outcomes, but even those in their 60s and 70s see major improvements in blood sugar control and reduced medication use.
It’s Not a Cure-It’s a Lifelong Commitment
Some people think surgery fixes diabetes forever. It doesn’t. Remission rates drop over time. The Swedish study showed 72% remission at two years, but only 36% at ten years. Why? Weight regain, slowing metabolism, and the natural progression of the disease.
But here’s the key point: even when diabetes comes back, it’s usually much milder. Patients who relapse still use fewer medications, have lower HbA1c levels, and face less risk of nerve damage, kidney disease, and vision loss. Dr. Philip Schauer found that for every year you stay in remission, your risk of microvascular complications drops by 19%.
That’s not nothing. That’s years of avoiding dialysis, amputations, and blindness.
What You Lose Along the Way
Metabolic surgery isn’t risk-free. Long-term studies show higher rates of nutritional deficiencies-especially iron, vitamin B12, calcium, and vitamin D. That’s why lifelong monitoring is non-negotiable. Blood tests every 6 to 12 months. Supplements daily. Skipping them can lead to anemia, bone fractures, or neurological damage.
Gastrointestinal side effects like dumping syndrome (rapid emptying of the stomach), nausea, and diarrhea are common early on. Most improve over time, but they’re real. And yes, there’s a small risk of complications during surgery: leaks, infections, blood clots. But for most patients, the risk of dying from obesity-related complications is far higher than the risk from surgery.
One study found that surgical patients had a 40% lower risk of death over 10 years compared to those who didn’t have surgery. That’s not a small win.

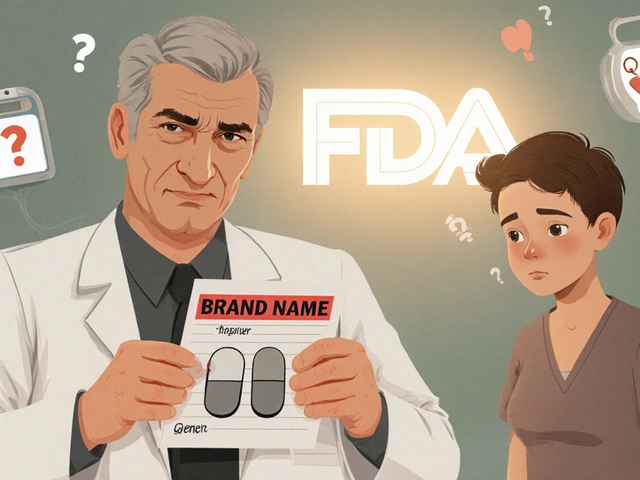
Why Isn’t Everyone Having It?
Despite the data, less than 2% of eligible patients in the U.S. get metabolic surgery each year. Why?
- Insurance won’t cover it if your BMI is under 35-even though studies prove it works for people with BMIs as low as 27.
- Doctors don’t always know the latest guidelines. Many still think surgery is only for “morbidly obese” patients.
- Patients fear surgery. They think it’s dangerous or that they’ll gain the weight back.
- There’s a lack of access. Not every hospital has experienced teams. The American Society for Metabolic and Bariatric Surgery says surgeons need to do at least 100 procedures to be truly skilled.
And yet, the global market for these procedures is growing fast-projected to hit $39 billion by 2030. Demand is rising. Awareness just hasn’t caught up.
What Comes Next?
Research is expanding. New trials are testing surgery on people with BMIs as low as 27. Endoscopic procedures-like gastric balloons and aspiration systems-are offering less invasive options for those who aren’t ready for full surgery. But none of them match the long-term results of gastric bypass or duodenal switch.
The most promising development? Recognizing that metabolic surgery isn’t just for weight loss. It’s for metabolic repair. The American Diabetes Association has included it in their official guidelines since 2016. The International Diabetes Federation endorsed it in 2011. The science is settled. The question now is: who gets access?
Final Thoughts
If you’ve been told your diabetes is “not bad enough” for surgery-or that you’re “too young” or “too old”-you deserve better. The data doesn’t lie. Metabolic surgery offers the best chance at lasting diabetes remission and major, sustainable weight loss. It’s not easy. It requires lifelong care. But for many, it’s the only path back to health.
It’s not about being perfect. It’s about giving your body a real shot at healing.
Can metabolic surgery cure type 2 diabetes?
Metabolic surgery doesn’t guarantee a permanent cure, but it can lead to long-term remission. About 30% of patients remain in remission 15 years after surgery. For many, blood sugar levels return to normal without medication. However, remission can fade over time due to weight regain or declining pancreatic function. Even when diabetes returns, it’s usually much milder and easier to manage.
Which metabolic surgery has the highest diabetes remission rate?
Biliopancreatic diversion with duodenal switch has the highest remission rate-up to 95% at one year. Gastric bypass follows closely at around 80%, while sleeve gastrectomy is around 37% at one year. The trade-off is that duodenal switch has a higher risk of nutritional deficiencies and requires stricter lifelong monitoring.
Do I need to be severely obese to qualify for metabolic surgery?
No. While guidelines traditionally required a BMI of 35 or higher, newer studies show strong results in patients with BMIs as low as 27-30. The American Diabetes Association now supports surgery for type 2 diabetes patients with BMI 30-34.9 if blood sugar remains uncontrolled despite medication and lifestyle changes. Insurance coverage still lags behind the science, but eligibility is expanding.
What are the biggest risks after metabolic surgery?
The most common long-term risks are nutritional deficiencies-especially iron, vitamin B12, calcium, and vitamin D-which can lead to anemia, bone loss, and nerve damage. Other risks include dumping syndrome, gallstones, and gastrointestinal issues like nausea or diarrhea. Lifelong blood tests and supplements are required. Surgical risks like leaks or infections are rare but serious, occurring in less than 5% of cases when performed by experienced teams.
How soon after surgery does diabetes improve?
Many patients see blood sugar improvements within days-sometimes even before significant weight loss occurs. This is because surgery changes gut hormone levels (like GLP-1 and PYY), which directly improve insulin sensitivity. Insulin requirements often drop dramatically in the first week. Complete remission can happen within weeks for some patients, especially those not yet on insulin.
Is metabolic surgery worth it if I’m not losing weight fast enough?
Yes. Weight loss is important, but it’s not the only benefit. Even patients who lose less than expected still see major improvements in blood sugar control, cholesterol, blood pressure, and medication use. The hormonal changes from surgery help the body use insulin better, regardless of how much weight is lost. Many patients reduce or eliminate diabetes medications even with modest weight loss.
What happens if my diabetes comes back after surgery?
If diabetes returns, it’s usually less severe than before surgery. Most patients still need fewer medications and have better overall control. The risk of complications like kidney disease, nerve damage, and vision loss remains lower than if they’d never had surgery. Ongoing monitoring, diet, and activity are still essential, but the baseline health is significantly better.
Can I have metabolic surgery if I’ve had diabetes for over 10 years?
Yes, but the chances of full remission are lower. The longer you’ve had diabetes, especially if you’ve been on insulin, the more your pancreas may have lost its ability to produce insulin. Still, many patients benefit from improved blood sugar control, reduced medication needs, and lower complication risks-even without full remission. Surgery is still valuable as part of long-term diabetes management.








10 Comments
This gave me hope. I’ve been on insulin for 8 years and thought I’d never get off it. After reading this, I’m scheduling a consultation. Not because I want to lose weight-but because I want to breathe again.
Thank you for sharing the truth.
Let’s be real-this whole ‘metabolic surgery is a cure’ narrative is dangerously oversimplified. Yes, some people lose weight and reverse diabetes-great! But what about the ones who develop severe malnutrition, chronic diarrhea, and lifelong vitamin dependency? What about the people who gain back 50% of the weight in five years and are left with a scar, a compromised digestive system, and zero support? The data cherry-picks the winners and ignores the silent majority who suffer quietly. And don’t get me started on the insurance gatekeeping-this isn’t medicine, it’s a luxury for the privileged who can afford the follow-up care. The ‘science is settled’ line? That’s what Big Pharma wants you to believe. The real science? It’s messy, it’s long-term, and it’s not as clean as this post makes it sound.
Also-why is no one talking about the psychological toll? You don’t just wake up ‘fixed.’ You wake up with a new body, a new identity, and a society that still judges you for being ‘fat’ even when you’re not.
And yes-I’m still mad about the dumping syndrome. It’s not just ‘common.’ It’s humiliating. You eat a banana and your insides revolt. That’s not biology. That’s trauma with a surgical stamp.
I appreciate how thorough this is. The numbers are staggering, but what sticks with me is the part about remission even in people with BMI under 35. That’s huge. So many doctors still dismiss patients who don’t fit the ‘morbidly obese’ mold. This should change the conversation. Not just for weight loss-but for metabolic health as a whole.
Also, the point about insulin use reducing remission chances? That’s critical. It means early intervention matters. We need to stop waiting until people are drowning before we offer them a lifeboat.
Oh please. You’re selling snake oil with a scalpel. You think people are going to believe this ‘hormonal magic’ nonsense? The body doesn’t just ‘rewire’ itself because you cut a piece out. This is just gastric bypass repackaged as a ‘cure’ to sell more surgeries. And the 95% remission stat? That’s from a tiny cohort of young, healthy patients with no comorbidities. Most people who get this surgery are diabetic, hypertensive, sleep apnea, fatty liver-half of them can’t even follow a post-op diet. And you think they’re gonna take their B12 supplements for life? Please. 80% of them are back on insulin in 3 years. The ‘40% lower death risk’? That’s because they’re not dying from obesity-they’re dying from complications from malnutrition, anemia, and osteoporosis. This isn’t a win. It’s a trade-off you don’t know you’re making until it’s too late.
And don’t even get me started on the surgeons making bank off this. $25k per procedure? That’s not medicine. That’s a gold rush.
I’ve sat across from too many patients who’ve been told, ‘You’re not sick enough.’ This post feels like a love letter to the forgotten. The way you describe the gut-hormone shift-it’s like the body finally gets to whisper its truth after years of screaming into a void. I’ve seen patients cry when their HbA1c drops to normal for the first time in a decade. Not because they lost weight. Because they felt human again.
The risks? Real. The side effects? Brutal. But the alternative-watching someone you love slowly lose their kidneys, their sight, their mobility-is worse. This isn’t a quick fix. It’s a second chance with heavy baggage. And if we’re honest? Most of us would carry that baggage in a heartbeat.
OMG I CRIED reading this 💔😭 I’m 32, diagnosed at 28, on insulin since 29, and my mom said ‘you’re too young for surgery’-but what if I’m too young to lose my legs?! 🙏🏽 I’m getting the duodenal switch in 3 months. This isn’t about being thin-it’s about being alive. I’m not a statistic. I’m a person who just wants to play with my niece without passing out from low blood sugar. 🌟✨ #MetabolicRevolution #DiabetesIsNotAFailure
From a clinical endocrinology perspective, the metabolic effects are well-documented, but the long-term efficacy is confounded by adherence to nutritional protocols and baseline beta-cell function. The GLP-1 axis modulation is indeed a pivotal mechanism, yet the heterogeneity in patient response underscores the need for stratified biomarkers-particularly fasting C-peptide levels and HOMA-B indices-to predict remission potential. Without proper patient selection, surgical intervention becomes a high-risk, low-yield proposition in the context of progressive beta-cell exhaustion. The data you cite, while compelling, lacks multivariate adjustment for duration of diabetes, insulin resistance burden, and hepatic fat content. In my practice, only 22% of patients with >10-year duration achieve durable remission, even with duodenal switch. The 95% figure is misleading without context.
So… I’m 34, BMI 31, on metformin, and my doctor said I don’t qualify because I’m ‘not obese enough.’ But I’ve been reading this and I’m like… wait, what? I’ve been trying for 5 years to lose 20 lbs. I’m tired of feeling like I’m failing. Is this actually for people like me? I’ve got prediabetes now too. I’m scared to ask my doctor because I think they’ll just say ‘try harder.’ But this says… maybe I don’t need to try harder. Maybe I need a different path. I just need someone to tell me it’s okay to want this.
Also… is ‘dumping syndrome’ as bad as people say? I’ve seen videos. It looks terrifying.
Let’s clarify terminology here-this isn’t ‘metabolic surgery’-it’s bariatric surgery with metabolic side effects. The term ‘metabolic surgery’ was coined by a group of surgeons in 2007 to rebrand bariatric procedures for insurance billing purposes. The physiological mechanisms are identical to what we’ve known since the 1950s. The ‘hormonal cascade’ is real, but it’s not new. The novelty is the marketing. And the ‘95% remission’? That’s from a 2012 study with n=38. Peer-reviewed? Yes. Generalizable? No. The American Diabetes Association’s endorsement? Based on meta-analyses that exclude patients with BMI <30. The data isn’t lying-it’s being selectively curated. You want truth? Read the 2023 Cochrane review. It’s sobering.
i just wanted to say thank you for writing this. i’ve been scared to even look into surgery because i thought i wasn’t ‘bad enough.’ but reading this made me feel seen. i’m 42, have had type 2 for 11 years, and i’m on 3 meds. i don’t want to be on meds forever. i don’t want my kids to watch me get sicker. i’m going to ask my doctor about this. not because i’m lazy or giving up-but because i’m done giving up on myself.
ps: sorry for the typos. i’m crying while typing this.