IBD Treatment Comparison Tool
Enter Your Patient Details
Recommended Treatment
Quick Take
- Entocort delivers high‑dose budesonide directly to the ileum and colon while sparing the rest of the body.
- It boasts a lower systemic steroid burden than prednisone but isn’t a cure‑all for ulcerative colitis.
- Alternatives such as mesalamine, Budesonide MMX, and biologics each target different disease mechanisms.
- Choosing the right therapy hinges on disease location, severity, and individual tolerance.
- Monitoring for adrenal suppression and bone loss remains essential, even with locally acting steroids.
Entocort is a capsule formulation of budesonide designed for targeted release in the distal ileum and proximal colon. It belongs to the class of glucocorticoid receptor agonists and is approved primarily for induction of remission in mild‑to‑moderate Crohn's disease. The drug exploits high first‑pass hepatic metabolism (≈90% pre‑systemic clearance), which sharply reduces systemic exposure compared with conventional oral steroids such as prednisone.
Why Entocort Exists: The Pharmacology in Plain Terms
When you swallow a regular steroid pill, it rides through the gut, gets absorbed, and then circulates throughout your body. That widespread distribution is what gives steroids their power-and their side‑effects. Budesonide, the active ingredient in Entocort, is engineered to stick around in the gut long enough to calm inflammation locally before the liver deactivates it.
Key pharmacokinetic attributes:
- Targeted release: Enteric coating dissolves at pH>6, releasing the drug in the terminal ileum.
- First‑pass metabolism: Approximately 90% of absorbed budesonide is converted to inactive metabolites during its first pass through the liver.
- Systemic cortisol suppression: Typically <10% of the effect seen with an equivalent dose of prednisone.
This profile makes Entocort a favorite for patients who need steroid potency without the classic “weight‑gain, mood‑swing” fallout.
Major Players in the IBD Landscape
Inflammatory bowel disease (IBD) is a broad umbrella covering several distinct conditions. The two biggest are Crohn's disease and ulcerative colitis. While both involve gut inflammation, their patterns differ: Crohn's can affect any gastrointestinal segment and often penetrates deep layers, whereas ulcerative colitis locks onto the colon's surface.
Therapeutic strategies therefore split into three broad categories:
- Locally acting agents (e.g., budesonide, mesalamine).
- Systemic steroids (e.g., prednisone).
- Advanced therapies - immunomodulators and biologics (e.g., Vedolizumab, Adalimumab).
Side‑Effect Profiles: What to Watch For
Every medication carries trade‑offs. Below are the most clinically relevant risks for the four drugs we’ll compare.
- Entocort (budesonide): Mild adrenal suppression, rare candidiasis, possible headaches.
- Prednisone: Weight gain, hypertension, glucose intolerance, osteoporosis, mood changes.
- Mesalamine (5‑ASA): Kidney dysfunction, pancreatitis, mild nausea.
- Budesonide MMX: Similar to Entocort but slightly higher systemic exposure; occasional nausea.
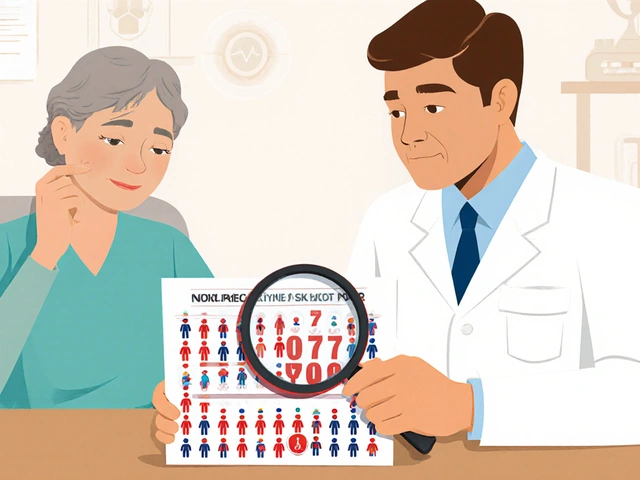
Because budesonide’s liver‑first‑pass action limits systemic cortisol, long‑term bone loss is less common, yet clinicians still recommend baseline DEXA scanning for patients on therapy longer than three months.

Head‑to‑Head: Entocort vs Alternatives
| Attribute | Entocort (Budesonide) | Prednisone | Mesalamine | Budesonide MMX |
|---|---|---|---|---|
| Primary indication | Induction in mild‑to‑moderate Crohn’s (ileum/ascending colon) | Broad‑spectrum steroid for acute flares (any IBD) | Maintenance in ulcerative colitis, mild Crohn’s | Induction in both Crohn’s and ulcerative colitis (colon‑wide) |
| Mechanism | Glucocorticoid receptor agonist with high first‑pass metabolism | Systemic glucocorticoid, full cortisol effect | 5‑ASA anti‑inflammatory, topical | Same as Entocort, but MMX matrix releases throughout colon |
| Typical dose | 9mg once daily | 40‑60mg daily taper | 2‑4g daily split | 9mg once daily |
| Systemic exposure | Low (≈10% of prednisone) | High | Negligible | Moderate (≈20% of prednisone) |
| Common side‑effects | Headache, mild adrenal suppression | Weight gain, hyperglycemia, hypertension | Kidney injury, nausea | Nausea, rare adrenal suppression |
When you read the table, the pattern is clear: Entocort nails the sweet spot for patients with localized ileal Crohn’s who can’t tolerate a full‑blown steroid course. Mesalamine shines in ulcerative colitis maintenance, while prednisone remains the rescue gun for severe flares across the board. Budesonide MMX offers a middle ground for broader colon involvement but brings a modest increase in systemic exposure.
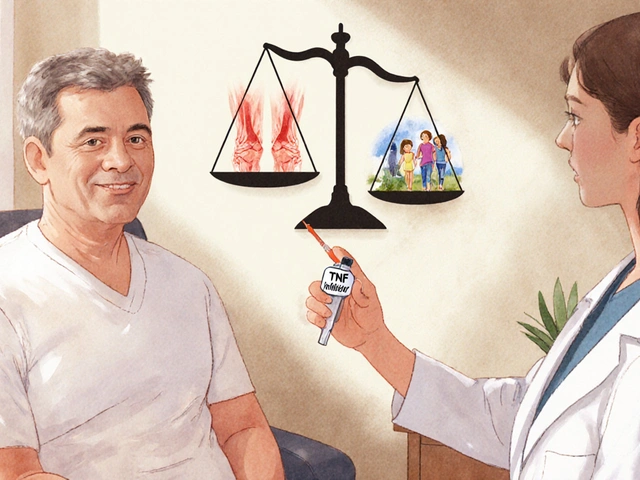
How to Pick the Right Option for You
Think of IBD treatment as a decision tree. Start with three questions:
- Where is the inflammation? If it’s confined to the terminal ileum, Entocort is a top candidate. If it’s pan‑colonic, consider Budesonide MMX or a 5‑ASA.
- How severe is the flare? Mild‑to‑moderate episodes often respond to locally acting steroids. Severe disease usually needs systemic steroids or biologics.
- What’s the patient’s risk profile? History of osteoporosis, diabetes, or mood disorders tips the scale toward low‑systemic options.
Practitioners also weigh costs and availability. In NewZealand, Entocort is subsidised for many patients under the PHARMAC schedule, while biologics may require special approval.
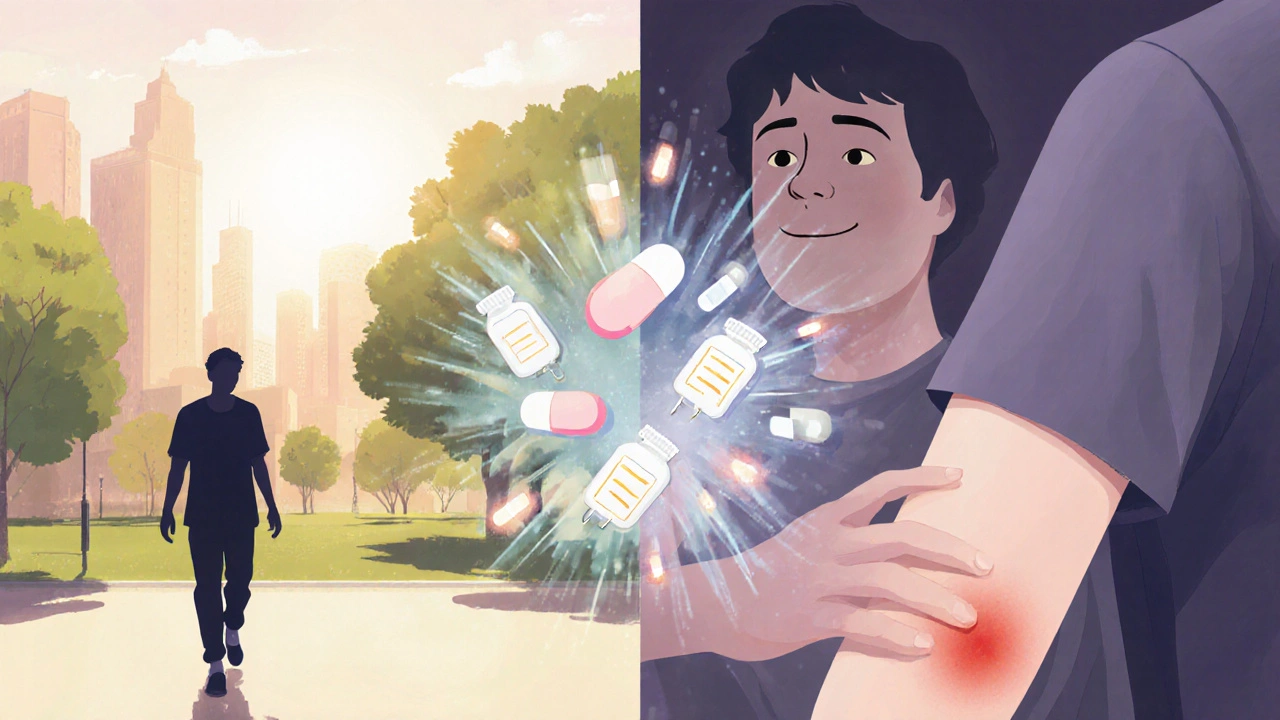
Real‑World Scenario: Meet Sam
Sam, a 29‑year‑old teacher from Dunedin, was diagnosed with Crohn’s disease affecting the terminal ileum. His gastroenterologist started him on 5‑ASA, but after six months Sam still had frequent abdominal pain and mild weight loss. A colonoscopy confirmed persistent inflammation. The doctor switched Sam to Entocort 9mg daily. Within eight weeks Sam reported a 70% reduction in pain, and a follow‑up scan showed mucosal healing.
Why didn’t Sam go straight to prednisone? He had a family history of osteoporosis, and the doctor wanted to avoid the systemic bone‑loss risk. Sam’s case illustrates how a targeted steroid can bridge the gap between mild therapy and heavy‑handed systemic steroids.
Managing Budesonide‑Related Risks
Even though Entocort’s systemic load is low, you still need a safety net.
- Baseline labs: Check fasting glucose, electrolytes, and a morning cortisol level.
- Bone health: DEXA scan before starting if you’re over 40 or have risk factors.
- Infection vigilance: Budesonide can still dampen local immunity; watch for oral thrush.
- Taper schedule: Unlike prednisone, Entocort often doesn’t require a complex taper, but abrupt cessation after >3months may cause rebound inflammation.
Patients on long‑term budesonide should also maintain adequate calcium and vitaminD intake.
Related Concepts Worth Exploring
Understanding Entocort fits into a bigger picture of IBD pharmacology. Here are a few adjacent topics you might want to dig into next:
- First‑pass metabolism: How the liver deactivates certain drugs, influencing systemic side‑effects.
- Glucocorticoid receptor polymorphisms: Genetic factors that affect individual response to steroids.
- Biologic therapy sequencing: When to move from steroids to agents like Vedolizumab.
- Therapeutic drug monitoring: Using blood levels to optimise biologic dosing.
Frequently Asked Questions
Can Entocort replace prednisone for all Crohn’s flares?
Entocort works best for mild‑to‑moderate disease limited to the ileum or right colon. Severe, extensive flares often need the broader anti‑inflammatory power of systemic steroids like prednisone, at least initially.
How long is it safe to stay on Entocort?
Most guidelines suggest a 12‑week induction course, followed by reassessment. If remission is achieved, patients usually transition to a maintenance agent such as mesalamine or a biologic.
What are the main differences between Entocort and Budesonide MMX?
Entocort releases budesonide early in the distal ileum, while the MMX matrix spreads release throughout the entire colon. Consequently, MMX has slightly higher systemic exposure and is chosen when inflammation is more diffuse.
Do I need to taper off Entocort?
Because systemic absorption is low, a formal taper is often unnecessary. However, stopping abruptly after several months can trigger a rebound flare, so a brief step‑down (e.g., 6mg for two weeks) is sometimes recommended.
Is Entocort safe for pregnant women?
Budesonide is categorized as FDA pregnancy category B, meaning animal studies show no risk, but human data are limited. Physicians usually weigh the benefits of disease control against potential fetal exposure; in many cases, controlling inflammation outweighs the modest risk.
How does mesalamine compare in effectiveness for Crohn’s disease?
Mesalamine is most effective for ulcerative colitis. In Crohn’s, especially ileal disease, its benefit is modest, and many clinicians reserve it for mild cases or as a maintenance adjunct.
What monitoring is required while on Entocort?
Baseline labs (CBC, electrolytes, fasting glucose, morning cortisol) and a DEXA scan if risk factors exist. Follow‑up labs every 3‑4months help catch adrenal suppression early.








13 Comments
Entocort saved my life when prednisone turned me into a puffy, anxious mess.
Let me tell you something nobody wants to admit-budesonide isn’t magic, it’s just a slower-acting steroid with a fancy coating. The pharmaceutical industry loves selling you ‘targeted’ solutions because they know you’ll pay double for the illusion of safety. Meanwhile, your adrenals are still gasping for air, your bones are thinning, and your doctor’s still getting paid every refill. They call it ‘lower systemic burden’-I call it ‘marketing spin with a side of osteoporosis.’ And don’t even get me started on the cost. $1,200 a month for a drug that’s basically prednisone in a tuxedo.
I’ve been on Entocort for 18 months now. It’s not perfect-yes, I still get the occasional flare-but compared to prednisone, it’s like switching from a sledgehammer to a scalpel. I used to sleep 14 hours a day and cry for no reason. Now I can go for walks, cook dinner, even babysit my niece without feeling like I’m about to explode. The bone density scan wasn’t great, but my endo put me on calcium and vitamin D and we’re monitoring it. Worth it. Also, the enteric coating? Total game-changer. I used to gag on pills, but these are small and swallow like butter.
so does it work for uc too or just crohns
Entocort’s pharmacokinetic profile demonstrates a favorable therapeutic index for ileal-predominant Crohn’s disease, particularly in treatment-naive patients. However, its efficacy diminishes significantly in pancolitis or left-sided UC due to suboptimal colonic release kinetics. The MMX formulation, by contrast, achieves more uniform distribution across the colon via pH-dependent and time-dependent release mechanisms, thereby offering superior mucosal healing rates in UC cohorts. Biologics remain first-line for moderate-to-severe disease, but for mild-to-moderate CD, Entocort remains a viable steroid-sparing agent with a 60% remission rate at 8 weeks in RCTs.
Entocort? More like Entocost. I paid $900 out of pocket last month. My insurance says it’s ‘not medically necessary’ unless I’ve tried five other things first. Meanwhile, my cousin in Canada gets it for $20. Someone’s making bank while we’re broke and bloated.
There’s something deeply human about how we chase these tiny pills hoping they’ll fix what’s broken inside us. We don’t just want the inflammation gone-we want to feel like ourselves again. The quiet mornings. The unweighted breaths. The ability to sit through a movie without thinking about the bathroom. Entocort doesn’t cure, but it gives space. Space to heal. Space to breathe. Space to hope. And sometimes, that’s more than enough.
Why are we even talking about this? Just take prednisone, deal with the side effects, and get on with your life. This country’s gone soft.
did u know the gov is hiding the truth about budesonide? they dont want you to know its made in china and the capsules are laced with microchips to track your bowel movements. my cousin works at the fda and she says its all part of the big pharma surveillance network. also the color of the pill is a code for your blood type. i swear its true. check the patent filings.
I get why people hate the cost and the side effects but honestly I think we’re all just trying to find something that lets us live without being a prisoner to our guts. I’ve tried everything. Mesalamine did nothing. Biologics made me sick. Entocort? It’s not perfect but it lets me go to work without planning my day around a toilet. I’m not gonna say it’s perfect but I’m not gonna throw it away either.
Let me be clear: if you’re taking Entocort because you’re too lazy to fix your diet, heal your gut microbiome, or stop eating gluten, you’re not treating the disease-you’re treating your denial. The pharmaceutical industry has convinced you that a pill can replace truth, discipline, and responsibility. You think budesonide is the answer? It’s a bandage on a bullet wound. Real healing comes from fasting, fermented foods, stress reduction, and stopping the cycle of self-sabotage. You want to be well? Stop looking for a magic bullet and start looking in the mirror.
Entocort gave me back my life but I still cry sometimes when I think about all the years I wasted on prednisone. I’m not mad at the drug-I’m mad at the system that made me wait 7 years to find it. Also 🤍
Wait-so if Entocort is metabolized 90% by the liver, does that mean it’s being used to test liver toxicity in people with IBD? Because I read somewhere that the FDA is quietly monitoring liver enzymes in IBD patients on budesonide as part of a larger surveillance program for organ manipulation. My neighbor’s cousin’s dentist’s assistant heard it on a podcast. It’s not in the pamphlet, but the small print says ‘may interact with undisclosed substances.’ I’m not saying it’s a conspiracy… but why is the warning so vague?