When you see bright red blood in your stool, it’s scary. You might think it’s just hemorrhoids. But if you’re over 60, it could be something more serious - like diverticula bleeding or angiodysplasia. These are two of the most common causes of lower GI bleeding, and knowing the difference can save your life.
What Exactly Is Lower GI Bleeding?
Lower gastrointestinal bleeding means blood is coming from somewhere in your colon, rectum, or anus - anywhere past the ligament of Treitz, which is deep inside your abdomen. The most obvious sign? Hematochezia: bright red or maroon blood in your stool. Sometimes it’s just a streak. Other times, it’s a full stream, like a faucet turned on. You might even pass clots. This isn’t the same as melena - that’s black, tarry stool from upper GI bleeding. If you’re seeing red, it’s almost always lower. About 1 in 5 people with GI bleeding have it in the lower tract. And it’s not rare: 20 to 27 people out of every 100,000 get it each year, mostly over age 60.Diverticula: The Silent Bleeder
Diverticula are tiny pouches that stick out from your colon wall. They’re common - nearly half of people over 60 have them. Most never cause problems. But sometimes, a blood vessel running near the base of one of these pouches gets torn. That’s diverticular bleeding. Here’s what makes it dangerous: it’s often painless. You don’t feel cramps or fever. One minute you’re fine. The next, you’re losing a lot of blood - sometimes enough to make you dizzy or pass out. It can look like you’ve been stabbed in the gut. About 30% to 50% of all hospitalizations for lower GI bleeding are from diverticula. And here’s the twist: the bleeding usually stops on its own. In 8 out of 10 cases, it just… stops. But that doesn’t mean you can ignore it. You still need to get checked. Why? Because it can come back. And if you’re on blood thinners or have heart disease, the risk of complications goes up.Angiodysplasia: The Slow Leak
Now, think of angiodysplasia as the opposite of diverticula. Instead of a sudden gush, it’s a slow drip. These are abnormal, fragile blood vessels in the colon wall - usually in the right side, near the cecum. They form because as you age, your blood vessels stretch and weaken. Think of them like old, frayed garden hoses. Unlike diverticula, angiodysplasia rarely causes a big, scary bleed. Instead, it leaks slowly over weeks or months. That’s why most people don’t even notice the blood. They just feel tired. Weak. Out of breath climbing stairs. Their doctor finds they’re anemic - hemoglobin below 10 g/dL - and wonders why. It’s the second most common cause of major lower GI bleeding after diverticula. About 3% to 6% of cases, but up to 40% in older adults with chronic anemia. It’s especially common in people with aortic stenosis - a narrowed heart valve. The turbulent blood flow there damages clotting proteins, making bleeding more likely.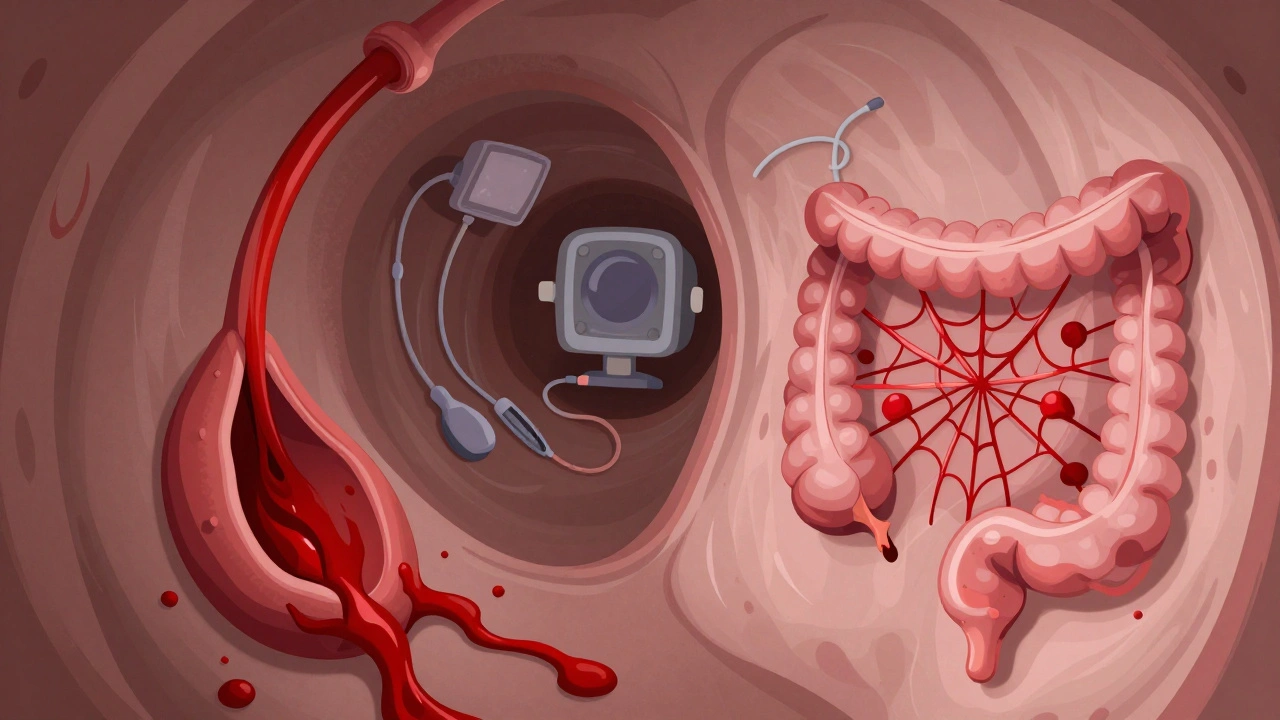
How Do Doctors Know What’s Causing It?
The first thing any doctor does when you show up with bleeding? Stabilize you. Check your blood pressure. Heart rate. Hemoglobin level. If you’re pale, sweaty, and your systolic pressure is below 100, you’re high risk. That means you need fast action. Then comes the workup - a step-by-step plan to find the source.- Blood tests: CBC (to check hemoglobin), coagulation panel (to see if you clot normally), and type and crossmatch (in case you need a transfusion).
- Colonoscopy: This is the gold standard. Done within 24 hours if possible. Studies show it cuts death risk by 26% compared to waiting 48 hours. Doctors use a scope to look inside your colon. They’re looking for red, oozing spots (diverticula) or flat, spiderweb-like red patches (angiodysplasia).
- CT angiography: If the colonoscopy doesn’t show anything, but you’re still bleeding, they’ll do a CT scan with contrast. It’s great at spotting active bleeding - 85% accurate if blood is flowing faster than half a milliliter per minute.
- Capsule endoscopy: You swallow a tiny camera. It takes pictures as it moves through your small intestine. It finds the cause in 62% of cases where colonoscopy was normal. But it’s not perfect - 15% of people have a capsule stuck if they have unseen strictures.
- Device-assisted enteroscopy: A longer scope that reaches deeper into the small bowel. More invasive, but it finds bleeding in 71% of tough cases. Used when capsule endoscopy shows something but you need to treat it right away.
What Happens After They Find the Source?
Treatment depends on what’s bleeding.For diverticula: Most stop bleeding on their own. You get IV fluids. Maybe a blood transfusion. If it keeps bleeding, they go back in with a colonoscope. They inject epinephrine to shrink the blood vessel, then use heat or clips to seal it. Success rate? 85% to 90%. But it can come back - 20% to 30% of people bleed again within a year. If it keeps happening in the same spot, they might remove that part of the colon.
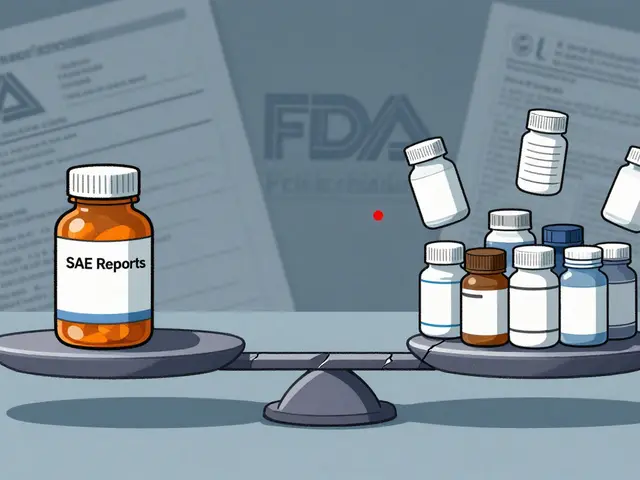
For angiodysplasia: The go-to treatment is argon plasma coagulation (APC). It’s like a laser that zaps the abnormal vessels. It stops the bleeding right away in 80% to 90% of cases. But here’s the catch: 20% to 40% of people bleed again within two years. That’s why some patients end up with multiple procedures.
For those with recurring angiodysplasia, doctors now use drugs like thalidomide (100 mg daily). A 2019 study in Gut showed it cuts transfusion needs by 70%. Octreotide, a hormone-like drug, helps too - given as shots three times a day. It’s not a cure, but it reduces bleeding episodes.
If everything else fails, surgery is an option. For angiodysplasia in the right colon, a right hemicolectomy (removing the right side of the colon) is common. For diverticula that keep bleeding in one segment, they remove just that piece.
What You Need to Know
- Diverticula = sudden, heavy, painless bleeding. Often stops on its own. High risk of recurrence if you’re older or on blood thinners. - Angiodysplasia = slow, chronic bleeding. Leads to anemia, fatigue, weakness. Often missed because it’s not dramatic. - Colonoscopy within 24 hours is critical. Delaying it increases your risk of death. - Don’t assume it’s hemorrhoids. Especially if you’re over 60, or have heart disease, or are on anticoagulants. - AI-assisted colonoscopy is now being used in some hospitals. It boosts detection of angiodysplasia by 35% - meaning fewer missed diagnoses.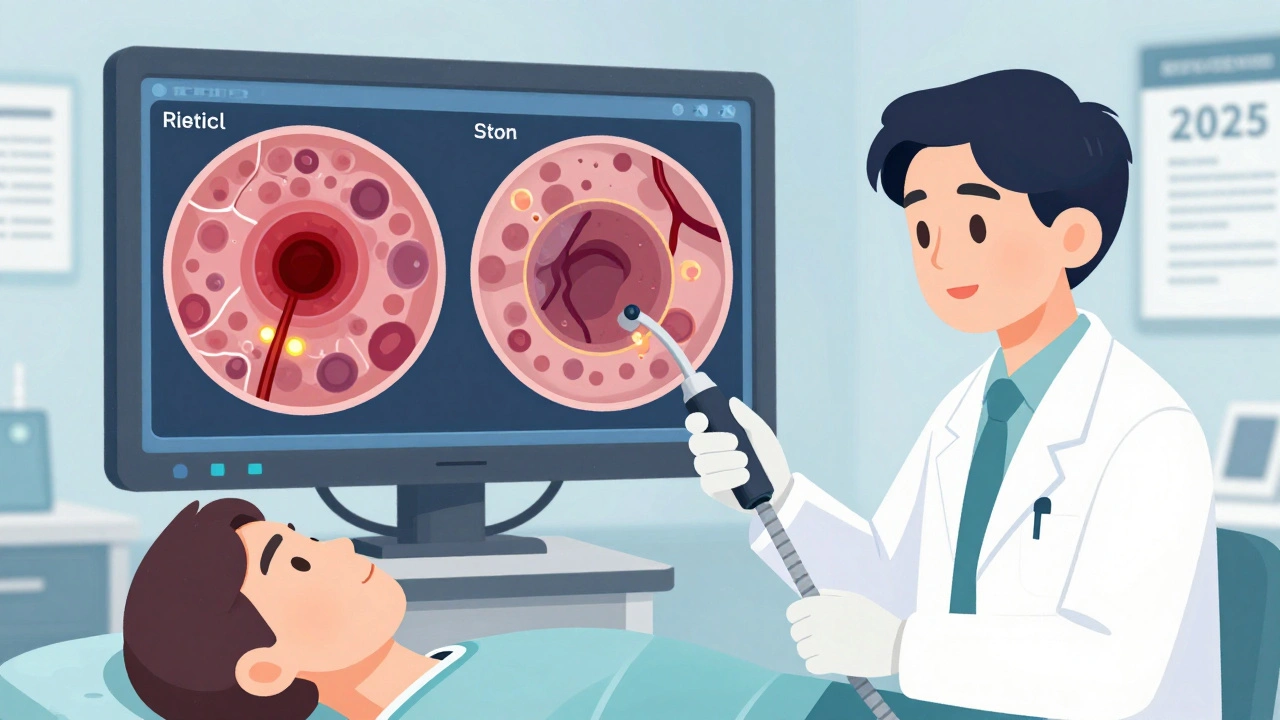
What’s New in 2025?
A big clinical trial funded by the NIH (NCT04567891) is wrapping up. It’s testing thalidomide vs. placebo for recurrent angiodysplasia. Early results suggest it’s one of the best medical options we have. Also, new endoscopic clips are showing 92% success in stopping diverticular bleeding - better than older methods.Long-Term Outlook
The good news? Most people survive. Five-year survival rates are 78% for diverticula and 82% for angiodysplasia. But survival isn’t about the bleed - it’s about your other health problems. Heart disease. Diabetes. Kidney issues. Those are what really affect your outcome. The real challenge? Repeated bleeding. Patients with angiodysplasia often go through a diagnostic odyssey - 18 months on average. Many have three or more negative colonoscopies before the real cause is found. That’s why if you’re anemic and no one can find the source, keep pushing. Ask about capsule endoscopy. Ask about CT angiography. Don’t give up.Frequently Asked Questions
Is lower GI bleeding always serious?
Not always, but it should always be taken seriously. About 80% of diverticular bleeds stop on their own, but the risk of rebleeding is high. Angiodysplasia bleeds are slower but can lead to chronic anemia, which strains your heart and reduces your quality of life. Any unexplained rectal bleeding in someone over 50 needs medical evaluation.
Can diverticula bleed without being inflamed?
Yes. Diverticular bleeding is different from diverticulitis. Bleeding happens when a blood vessel near the diverticulum ruptures - no infection or inflammation needed. You won’t have fever, cramps, or bloating. Just sudden, painless blood in your stool.
Why is angiodysplasia linked to aortic stenosis?
Aortic stenosis causes turbulent blood flow through the narrowed heart valve. This damages a clotting protein called von Willebrand factor. Without enough of it, your blood doesn’t clot properly - even in small vessels like those in the colon. That’s why doctors check for heart valve problems in older patients with unexplained GI bleeding.
Can I prevent diverticula from bleeding?
You can’t prevent diverticula from forming - they’re part of aging. But you can reduce your risk of bleeding by avoiding NSAIDs like ibuprofen and naproxen, which can irritate the colon. Eating a high-fiber diet helps prevent constipation and straining, which lowers pressure in the colon. Staying hydrated and exercising regularly also help.
If I had one episode of bleeding, will it happen again?
Yes, especially with angiodysplasia. Up to 40% of patients bleed again within two years. With diverticula, rebleeding happens in 20% to 30% of cases. That’s why follow-up is key. Your doctor may recommend repeat colonoscopy in 6 to 12 months, especially if you’re still on blood thinners or have other risk factors.
Are there any new treatments on the horizon?
Yes. A new type of endoscopic clip is showing 92% success in stopping diverticular bleeding. AI tools are now helping colonoscopists spot tiny angiodysplasia lesions they used to miss. And a phase III trial for thalidomide in recurrent angiodysplasia is expected to report results in late 2024 - it could become a standard treatment soon.








9 Comments
man i just saw red in my stool last week and thought it was hemorrhoids... turned out to be a diverticulum bleeding. i was lucky it stopped on its own but wow. never ignoring that again. thanks for the post, learned more in 10 mins than my last 3 doctor visits.
angiodysplasia is silent killer no one talks about it my aunt bled for 8 months no one knew why she was just tired then one day passed out in kitchen colonoscopy found it but by then hemoglobin was 6.5. doctors need to test for this sooner especially in elderly with heart issues. stop assuming its iron deficiency. its not. its vascular.
I’ve had two colonoscopies in the last five years... both 'normal.' I’m still anemic. I keep asking for capsule endoscopy. No one listens. I’m not just tired-I’m fading. If you’re over 65 and your doctor shrugs at low hemoglobin, find someone who won’t. This isn’t normal aging. It’s a clue.
so your body just gets old. blood vessels get weak. pouches form. you bleed. sometimes it stops. sometimes it doesn’t. you get a scope. you get a clip. you get a shot. you get told to eat fiber. that’s it. no magic. just time and medicine. we’re all one bleed away from a hospital.
colonoscopy within 24 hours. non-negotiable. delay = higher death risk. period.
my uncle had diverticula bleeding and kept getting better then worse again. they finally did a right hemicolectomy and he’s been fine for 3 years. if you keep bleeding, don’t wait. surgery is scary but so is losing blood every month. sometimes the fix is cutting out the problem, not just patching it.
It is profoundly concerning that the medical establishment continues to treat this as a purely mechanical, anatomical phenomenon-ignoring the ontological disintegration of the aging body as a systemic failure of vital integrity. One cannot simply 'clip' the collapse of biologic order.
It is unconscionable that patients are still being told to 'eat more fiber' as if this were a lifestyle choice rather than a physiological inevitability of aging. The normalization of gastrointestinal decay in the elderly is a moral failure of modern medicine.
I’ve watched three elderly relatives die from this. One bled out in the ER. Another got a transfusion, then went home-and bled again three days later. The third? They found the angiodysplasia after six months of misdiagnosis. They were 78. They didn’t deserve to suffer like that. This isn’t just medical-it’s a human rights issue. If you’re over 60 and you see red, you don’t wait. You don’t hope. You demand the scope. Now.