For over 25 years, metformin has been the go-to drug for managing type 2 diabetes. It’s cheap, effective, and generally safe. But behind its widespread use is a quiet, often overlooked risk: vitamin B12 deficiency. And it’s not rare. It’s common. And if left unchecked, it can lead to nerve damage, fatigue, and even irreversible neurological problems - all masked as worsening diabetes symptoms.
How Metformin Drains Your B12
Metformin doesn’t just lower blood sugar. It also interferes with how your body absorbs vitamin B12 in the small intestine. The drug blocks calcium-dependent receptors in the ileum - the final part of your small intestine - where B12 normally binds to a protein called intrinsic factor and gets pulled into your bloodstream. Without enough calcium to help this process, up to 30% less B12 gets absorbed. It’s not a mystery; it’s a known mechanism backed by multiple studies.
And it gets worse with time. The longer you take metformin, the more your body’s B12 stores drop. You start with about 2,500 micrograms stored in your liver. You only need 2.4 micrograms a day. So it takes years for symptoms to show up. That’s why most people don’t realize they’re deficient until they’ve been on metformin for five, eight, or even ten years.
It’s not just the dose - though higher doses (2,000 mg/day or more) raise the risk - but the duration. A landmark 13-year study from the Diabetes Prevention Program found that each year of metformin use increased the chance of B12 deficiency by 13%. By year 10, nearly half of long-term users had levels low enough to cause problems.
Who’s Most at Risk?
Not everyone on metformin will develop B12 deficiency - but some groups are far more vulnerable.
- People taking 2,000 mg or more daily - Risk jumps significantly above this threshold.
- Those on metformin for 4+ years - Deficiency rarely shows up before this point.
- Vegetarians and vegans - If you don’t eat meat, eggs, or dairy, you’re already getting less B12 from food. Metformin makes it worse.
- People on proton-pump inhibitors (PPIs) - Drugs like omeprazole (Prilosec) reduce stomach acid, which is needed to free B12 from food. Add metformin, and absorption drops even further. Studies show up to 40% of diabetics on PPIs also develop B12 deficiency.
- Older adults - Natural B12 absorption declines with age. Metformin accelerates it.
One study found that patients with all four risk factors - high-dose metformin, PPI use, vegetarian diet, and age over 65 - had a 52% chance of being deficient after 12 years.
Symptoms That Get Mistaken for Diabetes
This is the dangerous part. B12 deficiency doesn’t always cause anemia. In fact, in over a third of cases, neurological symptoms appear first - and they look exactly like diabetic nerve damage.
Common signs include:
- Constant fatigue - reported by 72% of deficient patients in long-term studies
- Tingling or numbness in hands and feet - often blamed on diabetic neuropathy
- Muscle weakness - especially in legs, making walking harder
- Sore, red tongue or mouth ulcers
- Blurred or double vision
- Pale or yellowish skin
- Memory problems or brain fog
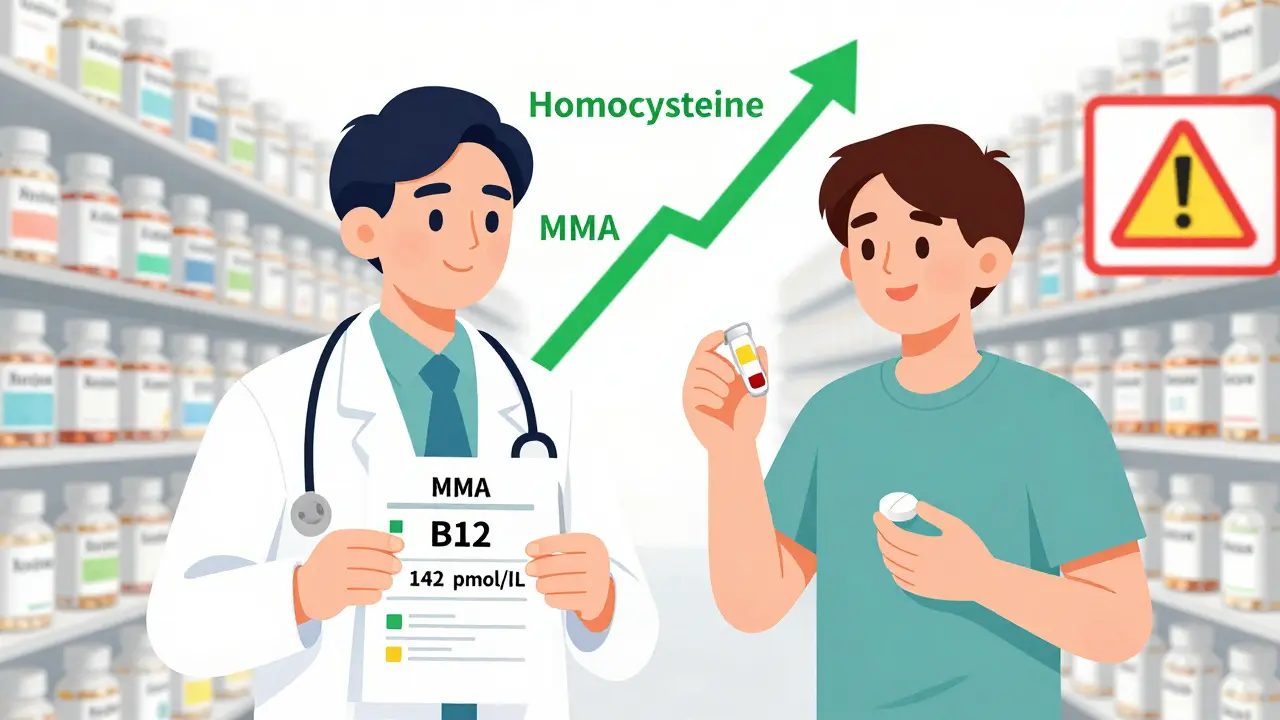
One patient on Reddit, u/MetforminSurvivor, spent five years being told his numb feet were just "worsening diabetes." Only after his B12 level hit 142 pmol/L (normal is above 221) did he get diagnosed with subacute combined degeneration - a serious spinal cord injury caused by long-term B12 lack. Some damage was permanent.
Another patient, "DiabeticSince2008," shared on NHS forums that after eight years on metformin, he was so weak he could barely climb stairs. His doctor finally tested his B12 - it was 128 pmol/L. After six months of injections, his energy returned. His nerve pain improved. He wasn’t getting worse from diabetes. He was just deficient.

Why Doctors Miss It
Many doctors still think B12 deficiency only shows up with anemia - pale skin, fatigue, fast heartbeat. But in metformin users, neurological damage often comes before any blood changes. A 2023 review found that 38% of patients had nerve symptoms before their blood tests showed low B12.
Also, standard B12 blood tests aren’t perfect. A level between 200 and 300 pmol/L might be "normal" on paper, but still too low for your nerves. That’s why experts now recommend checking methylmalonic acid (MMA) and homocysteine levels too. When B12 is low, MMA rises - even if your B12 number looks okay. It’s a more accurate signal of what’s happening in your tissues.
What You Should Do
If you’ve been on metformin for four or more years, here’s what you need to do:
- Ask your doctor for a B12 blood test - don’t wait for symptoms.
- Request MMA and homocysteine tests if your B12 is borderline (between 200-350 pmol/L).
- Get tested every 2-3 years - or annually if you’re vegetarian, on PPIs, or over 65.
- Consider calcium supplements - taking 1,200 mg of calcium carbonate daily has been shown to reduce B12 deficiency risk by 47% in metformin users.
- Don’t stop metformin - it’s still the best drug for most people with type 2 diabetes. Fix the deficiency, not the medication.
Treatment: Simple, Fast, Effective
Once you’re diagnosed, fixing it is straightforward.
For mild to moderate deficiency (B12 150-300 pmol/L):
- Take 1,000-2,000 mcg of oral B12 daily
- Results usually show in 4-8 weeks: energy improves, tingling fades
For severe deficiency (below 150 pmol/L) or neurological symptoms:
- 1,000 mcg injections once a week for 4 weeks
- Then monthly for life, or switch to high-dose oral if absorption improves
Studies show 89% of patients recover fully with treatment - but only if caught early. Delayed treatment can lead to permanent nerve damage.
The Bigger Picture
With over 150 million people worldwide taking metformin, even a 10-20% deficiency rate means millions are at risk. The UK’s NHS spends £47 million a year treating complications from undiagnosed B12 deficiency in metformin users. That’s preventable money - and preventable suffering.
Regulators are catching on. The FDA updated metformin’s label in 2022. The European Medicines Agency added B12 deficiency as a known side effect in 2021. NICE (UK) and the European Association for the Study of Diabetes now recommend routine testing. The American Diabetes Association says testing should be "considered" - but many experts argue that’s not enough.
Future solutions are coming. Researchers are testing enteric-coated metformin - a version that releases the drug lower in the gut, where it doesn’t interfere with B12 absorption. Early trials show 32% less B12 loss. Genetic testing may soon identify people with mutations in the cubilin gene - making them extra sensitive to metformin’s effect on B12.
For now, though, the solution is simple: test, treat, and monitor. You don’t need to stop metformin. You just need to know your B12 level.
What to Ask Your Doctor
Don’t wait for symptoms. If you’ve been on metformin for four or more years, ask these questions:
- "Have you checked my vitamin B12 level?"
- "Can we also test my methylmalonic acid (MMA) and homocysteine?"
- "Should I take calcium supplements with my metformin?"
- "How often should I get tested?"
- "If my B12 is low, what’s the best treatment for me - pills or shots?"
These aren’t niche questions. They’re essential. Your doctor should know the answer.











10 Comments
Been on metformin since 2017 and never thought about B12 until now. My legs have been tingling for years and my doc just said it's neuropathy. Guess I'm getting tested next week. Thanks for the clarity
Let me tell you something they don't want you to know. Big Pharma doesn't care if you lose your nerves or your memory because they make more money off the injections and the supplements than they do on metformin itself. They've known about this since the 90s. The FDA update? A PR stunt. The real reason they're not warning everyone is because if they did, millions would stop taking it and then where would the insulin sales be? And don't even get me started on the calcium myth - calcium doesn't fix absorption, it just masks the problem while they quietly push you toward their patented B12 patches that cost $89 a month. The truth is, your gut isn't broken - your system is being manipulated. You think you're managing diabetes? You're being managed. Wake up.
They told us metformin was the miracle drug. But what if the miracle was just a slow poison wrapped in a prescription? 🤔 We’ve been conditioned to trust doctors, trust labels, trust science - but science is just the language of power dressed in a lab coat. B12 deficiency isn't a side effect - it’s a signature. The body screaming, "I’m not broken, you’re poisoning me." And now they want us to take calcium? Like that’s a bandaid on a bullet wound. What about the real question: why are we even relying on a drug that steals what keeps us alive? Maybe the real treatment isn’t more supplements - it’s rethinking the entire framework of how we treat diabetes. We’re treating symptoms, not systems. And systems are broken.
OMG I’M SO GLAD I READ THIS!!! I’ve been on metformin for 7 years and my B12 was 180 last year!!! I was told "it’s fine" until I demanded MMA testing - it was through the roof!!! Now I’m on daily 2000mcg B12 and I swear I’ve gotten 10 years of my life back!!! My brain fog is GONE!!! I can climb stairs again!!! My doctor was like "huh, interesting" and now he’s asking me to lecture his residents!!! YOU’RE A LIFESAVER!!!
As someone who's worked in global health for over 15 years, I’ve seen this play out in rural clinics and urban hospitals alike. In places where blood testing is scarce, B12 deficiency gets mislabeled as malnutrition or aging - and metformin users in low-resource settings often go undiagnosed for decades. The irony? The drug is hailed as a cost-effective solution, but the long-term neurological damage creates far greater economic burdens. The real innovation isn't in new formulations - it's in integrating B12 screening into standard diabetes protocols everywhere, not just in the U.S. or Europe. This isn’t niche. It’s universal.
Oh sweet celestial irony - the diabetic population, the very group that prides itself on "discipline" and "control," is being slowly dismantled by a drug they worship like a god. And now they’re being told to swallow calcium pills like obedient sheep? Pathetic. I’ve seen patients on metformin for 12 years with B12 levels lower than my cat’s. And yes, I know cats need B12 too - they’re more aware of their bodies than most humans on Big Pharma’s payroll. If you’re still taking metformin without testing, you’re not managing diabetes - you’re performing a slow suicide with a prescription.
It is with profound concern and deep conviction that I address this critical issue. The systemic failure to routinely screen for vitamin B12 deficiency among long-term metformin users constitutes not merely an oversight - it is, in fact, a breach of the ethical imperative to do no harm. The data are unequivocal. The mechanisms are well-documented. The consequences are irreversible. To delay testing is to gamble with neurological integrity. I implore every healthcare provider, every patient, every advocate: act now. Request the tests. Demand the protocols. The time for passive acceptance has expired. Vigilance is not optional - it is the very foundation of compassionate care.
Let me be perfectly clear - if you are on metformin for more than four years and have not had your B12, MMA, and homocysteine levels checked, you are not being responsible. You are being negligent. And if your doctor hasn’t brought this up, they are either uninformed or indifferent. Neither is acceptable. This isn't about fear-mongering - it's about basic science. You wouldn't drive a car without checking the oil. Why are you driving your body without checking your B12? This isn't a suggestion. It's a medical obligation. Stop making excuses.
In my village in Nigeria, we say: "The medicine that cures the body may starve the soul." Metformin saves lives, yes - but at what cost? I have seen elders with trembling hands, walking like ghosts, told their diabetes is worsening - when in truth, their cells are whispering for B12. We do not have labs everywhere, but we have community health workers. We have elders who remember when food was real - fish, yams, palm oil. Perhaps the answer is not just pills, but returning to food as medicine. And yes - calcium from crushed eggshells, boiled in water, has been used for generations. Science is rediscovering what tradition never forgot.
While the clinical evidence supporting routine B12 screening in metformin users is compelling, it remains insufficiently codified in national guidelines. The absence of a mandatory testing protocol constitutes a gap in standard of care. Until such time as the ADA formally recommends annual screening for all long-term users, the burden of initiating testing remains disproportionately on the patient - an inequity that perpetuates disparities in outcomes. This is not a matter of opinion. It is a matter of clinical governance.