Travel Blood Clot Risk Calculator
Personalized Travel Risk Assessment
This tool estimates your risk of developing a travel-related blood clot based on your medical history and travel plans.
Traveling internationally while on blood thinners doesn’t have to be scary-but it does require smart planning. If you’re taking anticoagulants like warfarin, rivaroxaban, or apixaban, your biggest worry isn’t the flight itself. It’s the deep vein thrombosis (DVT) that can sneak up during long trips. You’re not alone: about 4 million Americans are on long-term blood thinners, and roughly 65% of them travel at least once a year. The good news? Most people who take their meds as prescribed and follow simple safety steps can fly, train, or drive across the globe without a clot forming.
Why Travel Increases Your Risk of Blood Clots
Long trips-especially those over 4 hours-raise your risk of DVT because sitting still slows blood flow in your legs. This isn’t about economy class. It’s about immobility. Back in the 1970s, people called it “economy class syndrome,” but doctors now know seat class doesn’t matter. What matters is how long you sit without moving. Your blood starts to pool. If you’re already on anticoagulants, your body is trying to balance clotting and bleeding. Skip a dose? Your blood gets stickier. Stay seated too long? That stickiness can turn into a clot. The risk isn’t the same for everyone. If you’re over 40, have a BMI over 30, recently had surgery, have cancer, or had a blood clot before, your risk jumps. The CDC says for someone with no extra risk factors, the chance of a travel-related clot is about 1 in 4,656 flights. But if you have three or more risk factors? That jumps to 1 in 1,000. That’s why knowing your personal risk level isn’t optional-it’s essential.What You Should Do Before You Leave
Start planning at least 4 to 6 weeks before your trip. First, talk to your doctor. Don’t assume your regular anticoagulant is fine for travel. If you’re on warfarin, get an INR test 1 to 2 weeks before departure. Your target range? Usually 2.0 to 3.0 if you’re on it for atrial fibrillation, or 2.5 to 3.5 if you have a mechanical heart valve. If your INR is unstable or your trip lasts more than two weeks, consider getting a portable INR monitor like the Roche CoaguChek® Mobile. It costs around $299, and test strips run about $7.50 each-but it gives you control when you’re far from a lab. If you’re on a DOAC like rivaroxaban or apixaban, you don’t need blood tests. But you need to know if it’s available where you’re going. Apixaban isn’t sold in 32% of low-income countries, according to WHO data. Pack extra. Always carry a printed list of your medications, doses, and your doctor’s contact info. Include your most recent INR result if you take warfarin. Some countries won’t recognize your prescription unless you have documentation.How to Take Your Medication While Traveling
Never skip a dose. That’s the single biggest mistake people make. Anticoagulants work best when taken consistently. If you skip even one day, your blood can become more prone to clotting than if you never took the drug at all. Time zones? Don’t change your schedule based on local time. Take your pill at the same clock time you always do. If you normally take it at 7 p.m. in New York and you land in Tokyo 16 hours later, still take it at 7 p.m. your home time-or adjust to your new time zone only if your doctor advises it. Most experts say stick to your usual schedule to avoid confusion. For those on low molecular weight heparin (LMWH) like dalteparin, you’ll need to carry needles and refrigerate them. That’s a hassle on long trips. DOACs are easier: they’re pills, no refrigeration needed. But they’re expensive. Rivaroxaban can cost $575 for 30 tablets in the U.S., while warfarin is under $5. If cost is a barrier, talk to your doctor. Sometimes switching back to warfarin for travel is safer than risking a clot.
What to Do During Your Trip
Move. Every 30 minutes, do seated calf exercises: point your toes up toward your nose, hold for 5 seconds, then point them down. Repeat 10 times. Every 2 to 3 hours, get up and walk. On a plane, walk the aisle. On a train, stretch your legs in the hallway. On a road trip, stop every few hours and walk around a gas station or rest area. Don’t just sit and scroll. Movement keeps your blood flowing. Wear compression stockings. Not the kind you buy at the drugstore. You need properly fitted below-knee graduated compression stockings that give 15-30 mmHg pressure at the ankle. These aren’t fashion accessories-they’re medical tools. The American College of Chest Physicians and CDC both recommend them for high-risk travelers. They help squeeze blood back up from your legs, reducing the chance of pooling. Drink water. Avoid alcohol and sugary drinks. They dehydrate you. Dehydration thickens your blood. That’s the opposite of what you want. Carry a refillable water bottle and sip constantly. If you’re on a flight, ask for water even if you don’t think you’re thirsty.What to Watch For-Symptoms You Can’t Ignore
Most DVTs happen in one leg. Watch for swelling, warmth, redness, or pain that feels like a cramp. It doesn’t always hurt. About 72% of people with DVT have swelling in one leg, according to the RIETE registry. Don’t wait for pain. If one calf looks bigger than the other, get checked. Pulmonary embolism (PE) is the scary cousin of DVT. That’s when a clot breaks loose and travels to your lungs. Signs: sudden shortness of breath, sharp chest pain that gets worse when you breathe in, rapid heartbeat, or coughing up blood. These aren’t “maybe it’s just a cold” symptoms. They’re emergencies. If you have any of these, get to a hospital immediately-even if you’re in a country where you don’t speak the language. Don’t forget: clots can form up to eight weeks after travel. That’s not a myth. It’s documented in medical records. If you notice leg swelling or chest pain after you get home, don’t brush it off. Call your doctor.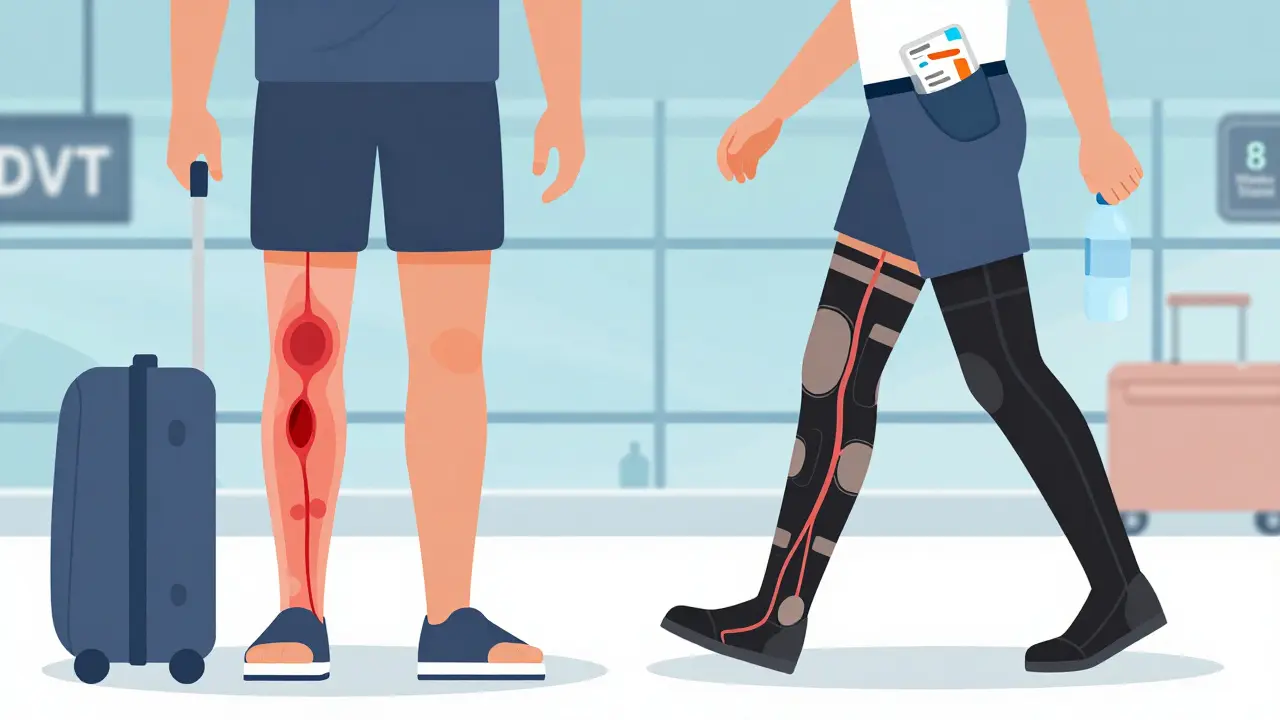
What You Shouldn’t Do
Don’t take extra blood thinners. The American College of Chest Physicians says clearly: don’t add aspirin or another anticoagulant just because you’re flying. It won’t help your risk of clots-it will raise your risk of bleeding. You’re already on a therapeutic dose. Adding more is dangerous. Don’t assume your doctor knows your travel plans. Many patients don’t tell them. That’s a mistake. Your doctor needs to know if you’re going somewhere remote, where medical care is limited, or if you’ll be out of touch for weeks. They might adjust your plan or give you a letter for border agents or airlines. Don’t forget your emergency contacts. Save local emergency numbers for your destination. Keep a card in your wallet with your medication list, doctor’s phone number, and a note saying you’re on anticoagulants. Some countries have emergency medical cards you can request in advance. Check with your embassy.When It’s Safe to Fly After a Blood Clot
If you’ve had a DVT or PE in the past, you might be worried about flying. The International Air Transport Association (IATA) says you can fly once you’re asymptomatic and stable on anticoagulants. That’s it. No specific waiting period. But most doctors recommend waiting at least 2 to 4 weeks after diagnosis. Cambridge University Hospitals advises against long-distance travel within four weeks of a clot. Why? Your body is still healing. The clot hasn’t fully stabilized. The risk of it breaking loose is higher. If you’ve had an unprovoked clot (no surgery, injury, or known trigger), your risk of another one is 30% over time if you stop your meds. That’s why doctors often recommend lifelong anticoagulation in these cases. Travel isn’t the problem. Stopping your meds is.Final Checklist for Safe Travel
- ☑ Talk to your doctor 4-6 weeks before departure
- ☑ Get INR tested if on warfarin
- ☑ Verify your medication is available at your destination
- ☑ Pack extra pills (at least 2 weeks’ supply beyond your trip)
- ☑ Carry a printed medication list and recent INR result
- ☑ Wear properly fitted compression stockings (15-30 mmHg)
- ☑ Drink water, avoid alcohol and sugary drinks
- ☑ Move every 30 minutes-calf exercises and walks every 2-3 hours
- ☑ Never skip a dose
- ☑ Know the signs of DVT and PE
- ☑ Save emergency contacts for your destination
Traveling on blood thinners isn’t about avoiding the world. It’s about moving through it safely. The science is clear: with the right prep, you can cross continents without a clot. You’ve already done the hard part-managing your condition. Now, just add a few smart habits, and your next trip can be as smooth as your medication schedule.







10 Comments
I’ve been on warfarin for six years now and have flown to Japan, Peru, and Iceland without a single clot. The key is movement and hydration - I carry a water bottle that’s bigger than my carry-on and I do those calf pumps every 30 minutes like clockwork. Even on a 14-hour flight to Bangkok, I got up and walked the aisle every time the seatbelt sign went off. People think I’m weird for doing 20 reps of toe-pointing in my seat, but I’d rather be the weirdo who’s healthy than the one in the ambulance.
Also, I got that CoaguChek monitor after my INR went haywire during a trip to Mexico. Worth every penny. I check it before I eat, before I sleep, and definitely before I board. It’s like having my doctor in my pocket.
And no, I don’t take aspirin ‘just in case.’ That’s how you end up in the ER with a bleed-out. Trust the regimen. It’s not magic, it’s math.
It is imperative that travelers on anticoagulant therapy adhere strictly to evidence-based guidelines as outlined in this comprehensive article. The American College of Chest Physicians, the CDC, and the World Health Organization all concur on the necessity of medication continuity, compression stockings, and mobility protocols. Deviations from these protocols, even minor ones such as altering dosing schedules due to time zone changes, may significantly elevate the risk of thromboembolic events.
Furthermore, it is recommended that patients obtain a formal letter from their prescribing physician, detailing medication names, dosages, and indication, particularly when traveling to jurisdictions with differing pharmaceutical regulations. Such documentation is not merely advisable - it is a critical component of medical preparedness in an international context.
This is such a helpful guide. I remember when I flew to Italy last year and didn’t realize how dehydrated I got until my legs felt like concrete. After this, I started carrying a big water bottle and doing those toe curls every hour - honestly, it made the whole trip feel way less stressful. I didn’t even think about how common this is until I read this. So many people are out there flying with blood thinners and just winging it. You’re not alone. And you’re doing great just by reading this and caring enough to plan.
Let’s be real - this whole ‘economy class syndrome’ thing is a myth pushed by airlines to sell you $120 compression socks. The real risk? Being sedentary for hours. But guess what? So is working at a desk job for 8 hours a day. Why is flying suddenly the villain?
Also, the CDC’s 1 in 4,656 stat? That’s meaningless without context. Most people who get DVTs after flying are over 65, obese, and on birth control - not because of the flight. And don’t get me started on the ‘never skip a dose’ dogma. Sometimes skipping a dose is the right call if you’re bleeding or in a country with zero medical access. This article reads like a pharmaceutical ad wrapped in a wellness blog.
There’s a metaphysical dimension to anticoagulant travel that this piece, for all its clinical precision, utterly ignores. You are not merely a biological system on a plane - you are a sentient vessel navigating the dissonance between corporeal fragility and the relentless momentum of global capitalism.
When you take rivaroxaban in the belly of a Boeing 787, you are performing a ritual of sovereignty over your own mortality. The compression stockings? They are not merely medical devices - they are the sartorial manifestation of your rebellion against gravity’s seduction. The water bottle? A chalice of consciousness, resisting the dehydrating entropy of corporate air travel.
And yet - you are still bound. Bound to schedules, to time zones, to the tyranny of the pill. The real question isn’t how to avoid clots - it’s how to remain unclotted in a world that wants you docile, compliant, and chemically tethered.
Just got back from a 3-week trip across Southeast Asia and this hit home. I was on apixaban and honestly didn’t think it’d be a big deal. Turns out I didn’t pack enough pills and had to scramble to find it in Laos. Lucky I had my doctor’s contact info saved. Also moved every 2 hours like they said - walked around every rest stop, did calf pumps on the bus. Felt way better than last time I flew and just sat there scrolling. Don’t be lazy. Your legs will thank you. And hey - if you’re reading this, you’re already doing better than half the people out there.
Also water. Drink water. It’s not that hard.
They don’t want you to know this but the real danger isn’t the clot - it’s the surveillance. Every time you use a portable INR monitor, your data is being uploaded to some corporate database. The airlines, the pharma giants, the government - they’re all tracking your blood. That’s why they push ‘compression socks’ - it’s a distraction. They want you thinking about calves while they monitor your INR trends and adjust your premiums. And don’t even get me started on how they ban LMWH on flights because it’s harder to control than pills. This isn’t safety. It’s control.
As someone from India who’s been on apixaban for 3 years, I’ve flown to Dubai, Singapore, and even remote parts of Nepal - and yes, the meds aren’t always available. I carry a printed prescription in English and Hindi, and I always ask for the generic name because brand names mean nothing here. Once in Kathmandu, I had to show the pharmacist the pill bottle from the US and he said ‘oh yes, this is Eliquis, we have it’ - but only because I knew to ask for the generic. Also, the calf exercises? I do them on the train, on the bus, even while waiting in line for chai. Movement is freedom. And don’t forget - the real enemy isn’t the flight, it’s the silence. Talk to your doctor. Tell someone your plans. Don’t suffer alone.
You’ve got this. Seriously. If you’re reading this article, you’re already ahead of 90% of people who are on blood thinners and just hoping for the best. Stop doubting yourself. Pack the extra pills. Wear the damn socks. Walk when you’re told to. It’s not complicated - it’s just inconvenient. And inconvenience is the price of freedom. You didn’t get this far by being passive. Don’t start now. Your future self is already thanking you.
Why is this article so focused on American guidelines? In the U.S., we have access to DOACs, insurance, and portable monitors. But in most of the world, people are choosing between food and warfarin. This isn’t ‘smart planning’ - it’s a luxury. The CDC’s statistics are meaningless when your country doesn’t even have a single anticoagulant clinic. The real problem isn’t DVT - it’s global healthcare inequality. And yet here we are, praising people who ‘follow the checklist’ like it’s some moral victory. Meanwhile, millions are forced to fly without meds, without stockings, without a chance. This isn’t empowerment - it’s victim-blaming dressed up as advice.