Getting a good night’s sleep shouldn’t feel like a battle. But if you have sleep apnea, every night can feel like a war against your own breathing. That’s where CPAP machines come in. They’re not glamorous, but they’re the most effective non-surgical treatment for obstructive sleep apnea - and they work. The problem? Most people quit using them. Not because they don’t help, but because they’re uncomfortable, confusing, or poorly fitted. If you’ve been told you need a CPAP, or you’re struggling to stick with it, this isn’t about willpower. It’s about finding the right machine, the right mask, and the right strategy to make it stick.
What Kind of CPAP Machine Do You Really Need?
Not all CPAP machines are the same. There are four main types, and picking the wrong one can make your nights miserable. The most common is the standard CPAP - it delivers one fixed pressure all night. If your breathing stays steady, this works fine. But if you toss and turn, wake up often, or your pressure needs change, you’ll fight the machine. Most people start here, but many end up switching. Then there’s APAP - the auto-adjusting version. Instead of one pressure, it scans your breathing and changes on the fly. If you snore harder in your back, it pushes more air. If you’re sleeping peacefully on your side, it backs off. This isn’t luxury - it’s smarter therapy. Studies show APAP users stick with it 15% more often than those on fixed-pressure CPAP. Models like the ResMed AirSense 11 AutoSet adjust pressure between 4 and 20 cm H2O, and most doctors now recommend it as a first choice, especially if you’re new to therapy. If you’re on high pressure - say, over 15 cm H2O - or you have another lung condition like COPD, you might need a BiPAP. This machine gives you two pressures: one for inhaling, a lower one for exhaling. It feels more natural. Patients who struggled with CPAP often say BiPAP was the first time they actually slept. The catch? It costs more - up to 30% higher - and needs a separate titration study to set the right pressures. But if you’re gasping for air every night, the extra cost is worth it. Then there are the oddballs: EPAP devices. These are tiny, nasal valves that cost under $150. They don’t pump air - they just create resistance when you breathe out. They’re only for mild sleep apnea (AHI under 15). If you’re in the moderate to severe range, they won’t cut it. A 2020 study found they worked for only 45% of users with worse apnea - compared to 85% for CPAP. Skip these unless your doctor says you’re a perfect candidate. And if you travel a lot, there’s the travel CPAP. The ResMed AirMini is the most popular. It’s smaller than a coffee mug, weighs less than a pound, and fits in your coat pocket. But it doesn’t have a built-in humidifier. You need to buy one separately. It’s also louder - around 52 dBA - compared to 30 dBA on standard machines. It’s not ideal for every night, but if you’re on the road, it’s better than skipping therapy.Mask Fit: The #1 Reason People Quit
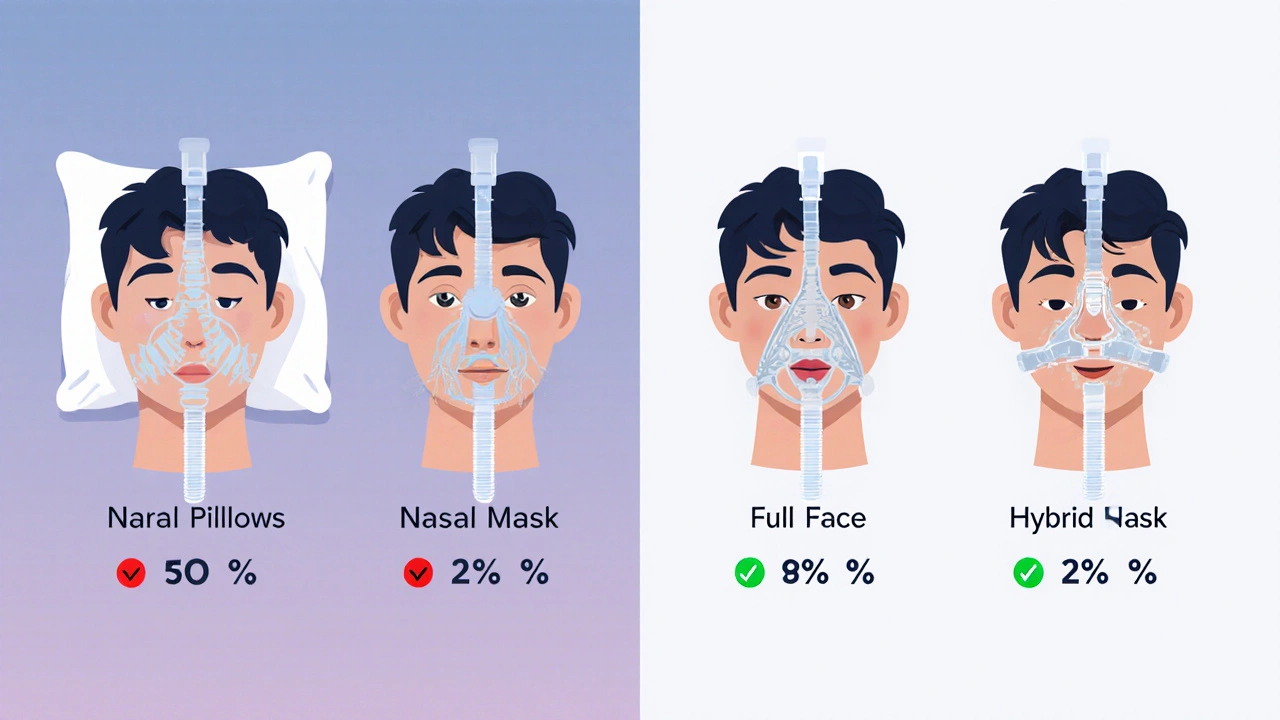
You can have the fanciest machine on the planet, but if your mask leaks like a sieve, you’re wasting your time. The American Academy of Sleep Medicine says 20-30% of people stop CPAP therapy because of mask discomfort - not because the machine doesn’t work. It’s not about being picky. It’s about anatomy. There are four main mask types:- Nasal pillows: Tiny silicone tips that sit at the edge of your nostrils. Best for side sleepers. Minimal face contact. Only 32% of users pick these, but they’re the most popular among long-term users. If you hate feeling claustrophobic, this is your best shot. User u/NasalPillowFan on Reddit cut their leak rate from 15 to 3 L/min after switching.
- Nasal masks: Cover your nose only. The most common type - used by 45% of people. Good balance of comfort and seal. Ideal if you breathe through your nose and don’t mind a bit of coverage.
- Full-face masks: Cover both nose and mouth. Used by 18% of users - usually mouth breathers or people with nasal congestion. But they cause 35% more skin irritation than nasal pillows. If you’re using one and getting red marks, you likely need a better fit, not a different mask.
- Hybrid/oral masks: Designed for severe nasal blockage. Only 5% of users. Rare, but life-changing for those who need them.
How to Actually Stick With It
Let’s be honest: CPAP therapy is hard. Only 46% of users meet the minimum standard of 4+ hours per night, 70% of nights. That’s not failure. That’s the system failing you. But you can beat the odds. Start slow. Don’t try to wear it all night on day one. Do this: spend 10 minutes a day, three times a day, wearing the mask while you watch TV or read. Get used to the feel. Then, turn on the machine at low pressure. Use the ramp feature - it slowly increases pressure over 5 to 45 minutes. Most users turn this on. It’s not optional - it’s essential. Humidification is non-negotiable. Dry nose, sore throat, congestion - those are the top complaints. Heated humidifiers (set between 86°F and 95°F) cut those complaints by 50%. If your machine doesn’t have one, get one. And use heated tubing. Users with heated tubes have 78% adherence. Those without? Just 52%. Track your data. Modern machines log your usage, leak rates, and AHI scores. Don’t ignore this. ResMed’s myAir app gives personalized coaching - users who use it see 27% higher adherence. If your AHI stays above 5, your pressure might be wrong. If leaks are high, your mask doesn’t fit. Use the numbers. Talk to your sleep specialist every two weeks. Don’t wait until you’re ready to quit. Sleep position matters. If you’re a side sleeper, get a CPAP pillow with cutouts for your mask. It reduces leaks by 40%, according to Reddit users. If you’re a stomach sleeper, nasal pillows are your friend. If you’re a back sleeper, you might need a full-face mask - but only if you’re mouth breathing.What’s New in 2025?
The tech has gotten quieter, smarter, and more personal. ResMed’s AirSense 11, launched in 2023, uses AI to predict breathing events before they happen - reducing AHI by 22% compared to older models. Philips’ DreamStation 3 dropped in late 2023 with whisper-quiet operation at 25 dBA - that’s quieter than a library. Regulations changed too. Starting in 2024, all CPAP machines sold in the U.S. must include usage tracking. Medicare and Medicaid now require you to use your machine at least 4 hours a night, 70% of nights - or they stop paying. Insurance companies are watching. So are employers. Trucking companies like Schneider Logistics now require drivers with AHI over 20 to use CPAP - and they’ve seen 32% fewer accidents. The market is shifting. ResMed holds 45% of the U.S. market. Philips has 30%. But after the 2021 foam recall that pulled 3.5 million Philips devices off shelves, ResMed’s stock jumped 35%. You’re not just buying a machine - you’re choosing a brand with reliability.
When CPAP Isn’t Enough
Some people try CPAP for months and still wake up exhausted. That doesn’t mean it’s broken. It might mean you have something else. About 5-15% of CPAP users develop treatment-emergent central sleep apnea - where the brain stops telling the body to breathe. That’s not obstructive - it’s neurological. For those cases, a machine like the ResMed AirCurve 10 ASV (adaptive servo-ventilation) is needed. It’s pricier - around $2,800 - but it’s the only thing that works. New tech is emerging too. Transcend’s Micro 3 uses transnasal pressure - it delivers air through tiny tubes inside the nose, not a mask. Fisher & Paykel’s SleepStyle has an algorithm that cuts exhalation pressure by up to 50%. It’s not mainstream yet, but it’s the future.What to Do Next
If you’ve been prescribed a CPAP and you’re scared: start with a mask trial. Don’t buy anything yet. Ask your sleep clinic for samples. Try nasal pillows first. If they don’t work, move to nasal masks. Use the ramp. Turn on the humidifier. Wear it for 10 minutes a day. Track your data. Talk to your provider every two weeks. If you’ve quit before: you’re not alone. But you’re not broken. You just didn’t get the right setup. Go back. Ask for an APAP. Ask for a different mask. Ask for a heated humidifier. Ask for a sleep coach. The machine isn’t the problem - the fit and the support are. Sleep apnea isn’t just about snoring. It’s about your heart, your brain, your energy, your life. CPAP works - if you can stick with it. And you can. You just need the right tools.Can I use a CPAP machine without a prescription?
In the United States, all CPAP machines require a prescription. Insurance won’t cover them without one, and most retailers won’t sell them without proof of diagnosis. Even if you find a machine online without a prescription, it’s risky - you might get the wrong pressure setting, which can be ineffective or even harmful. Always get a sleep study first.
How do I know if my CPAP mask fits properly?
A properly fitted mask shouldn’t leak, pinch, or cause red marks after removal. You should be able to breathe easily without feeling like your face is being squeezed. Check your machine’s leak rate - it should stay under 24 L/min. If it’s higher, your mask is too loose or the wrong size. Try adjusting the headgear straps evenly. If you still leak, try a different mask type. Nasal pillows often seal better than full-face masks for side sleepers.
Why does my CPAP machine make me feel bloated?
Bloating happens when you swallow air - a common side effect called aerophagia. It’s often caused by pressure that’s too high, or breathing too fast. Lower your pressure slightly, use the ramp feature to ease into it, and try sleeping with your head slightly elevated. If it continues, talk to your doctor. You might need a BiPAP machine, which reduces exhalation pressure and makes swallowing air less likely.
Is APAP better than CPAP for beginners?
Yes, for most beginners. APAP adjusts pressure automatically, so it handles changes in sleep position, alcohol intake, or congestion without you needing to call your doctor. A 2021 study in Sleep Medicine Reviews found APAP users had a 15% higher adherence rate than CPAP users. It’s more expensive, but the comfort and convenience often make it worth it - especially if your breathing varies at night.
How long does it take to get used to a CPAP machine?
Most people need 2 to 4 weeks to adjust. Some take longer - up to 3 months. The key is consistency. Don’t wait until you’re sleeping well to use it. Use it every night, even if it’s just for an hour. Build up slowly. Use the ramp feature. Try daytime practice sessions. Don’t give up after a week. The first few nights are the hardest - but the payoff - better sleep, more energy, clearer thinking - is real.
Can I travel with my CPAP machine?
Yes, and you should. Travel CPAPs like the ResMed AirMini are designed for this. They’re lightweight, fit in a backpack, and work on 110V and 220V power. You don’t need to skip therapy just because you’re away from home. Some airlines allow them as carry-ons. Bring extra batteries if you’re going somewhere with unreliable power. And if your machine doesn’t have a humidifier, consider a portable one - dry air can ruin your sleep even on vacation.










10 Comments
Just started my APAP last week and honestly? It’s been a game-changer. Used to hate the CPAP, but the auto-pressure thing? Feels like the machine is reading my mind. No more waking up gasping. Humidifier on 90°F and heated tube = life.
Ugh, I tried nasal pillows for 3 days and felt like a robot with nostril straws. Full-face all the way. If you’re mouth breathing, stop pretending it’s ‘just a phase.’ Your face isn’t the problem - your denial is.
you guys are overthinking this. just wear it. even for 10 min. every night. i started with 5 min. and now i sleep 8 hrs. no joke. the ramp and humidifier saved me. dont quit before you give it a real shot!!
Let’s be clear: CPAP is the pharmaceutical-industrial complex’s answer to a lifestyle problem. We’ve been conditioned to believe that breathing is a mechanical failure, when in reality, sleep apnea is often a symptom of chronic poor posture, obesity, and societal disconnection from natural circadian rhythms. The machine is a band-aid on a bullet wound.
Still… I use mine. Because I’m not a Luddite. Just a disillusioned realist with a ResMed AirSense 11 on my nightstand. And yes, I do use emojis: 🤖💤
As someone who’s been on APAP for 3 years and works in sleep tech, let me clarify a myth: APAP isn’t just ‘smarter’ - it’s statistically superior in titration accuracy. The algorithm doesn’t just react; it predicts micro-arousals based on flow patterns, not just snore amplitude. Most clinicians still default to CPAP out of habit, not evidence. A 2023 meta-analysis in JAMA Sleep showed APAP reduced AHI variability by 41% in patients with fluctuating obstruction patterns - think alcohol nights, allergies, or REM-predominant apnea. Also - humidification isn’t optional. It’s biomechanical. Dry mucosa = increased resistance = higher pressure needed = more aerophagia. Heated tubing? Non-negotiable. 78% adherence is real. Skip it, and you’re sabotaging your own data.
And yes, travel CPAPs are noisy. The AirMini hits 52 dBA because it’s compressing air in a 20cc chamber. That’s physics, not design flaw. But if you’re flying, it’s better than zero therapy. Bring a USB battery. And never trust a third-party mask without a 60-night trial. Your nasal bridge isn’t a one-size-fits-all mold.
Oh please. CPAP is for people who can’t just lose weight. I’ve had apnea since college. I stopped using mine after 2 months. Guess what? I lost 40 pounds. My AHI dropped to 2. No machine. No drama. Just food and sleep hygiene. Stop selling fear. This isn’t medicine - it’s a lifestyle audit.
I cried the first night I used my mask. Not because it hurt. Because I realized I hadn’t slept without gasping in 12 years.
Hey, if you're new to this - you're not alone. I'm a nurse in rural Ohio and I've helped over 50 patients get started. First thing I tell everyone: don't buy a mask online. Go to a sleep clinic. They have demo masks. Try them while you watch TV. Nasal pillows? They feel weird at first, but if you're a side sleeper? They're magic. And if your nose gets dry? Humidifier on. Heat the tube. It's not extra - it's essential. Also - track your data. Don't ignore the myAir app. It tells you when you're slipping. And if you feel bloated? Lower the pressure. Use ramp. You got this. One night at a time.
Just wanted to say - I quit CPAP twice. Failed. Felt like a failure. Then I switched to APAP, got nasal pillows, turned on the humidifier, and used the ramp. Now I sleep 7+ hours. My wife says I don’t snore anymore. My boss says I’m more focused. It’s not easy. But it’s worth it. You’re not broken. You just need the right fit. Don’t give up. 💪🌙
Why are we letting big pharma and ResMed control our breathing? In America, we don’t need machines to breathe. We need to fix the food, the stress, the laziness. CPAP is a crutch for weak people who won’t get off the couch. If you’re obese and sleep apneic - lose weight. That’s the real solution. Not some $3,000 plastic mask. This country is falling apart because we medicate instead of motivating.