TNF Inhibitor Cancer Risk Calculator
How Your Treatment Affects Cancer Risk
This tool helps you understand your personal cancer risk based on your TNF inhibitor type, steroid use, and medical history. Remember: TNF inhibitors have an excellent safety record when properly managed.
Skin Cancer Risk
Lymphoma Risk
Personalized Risk Summary
- Get skin exams every 6-12 months
- Keep steroid use as low as possible
- Monitor closely if you've had cancer before
- Check for tuberculosis before starting treatment
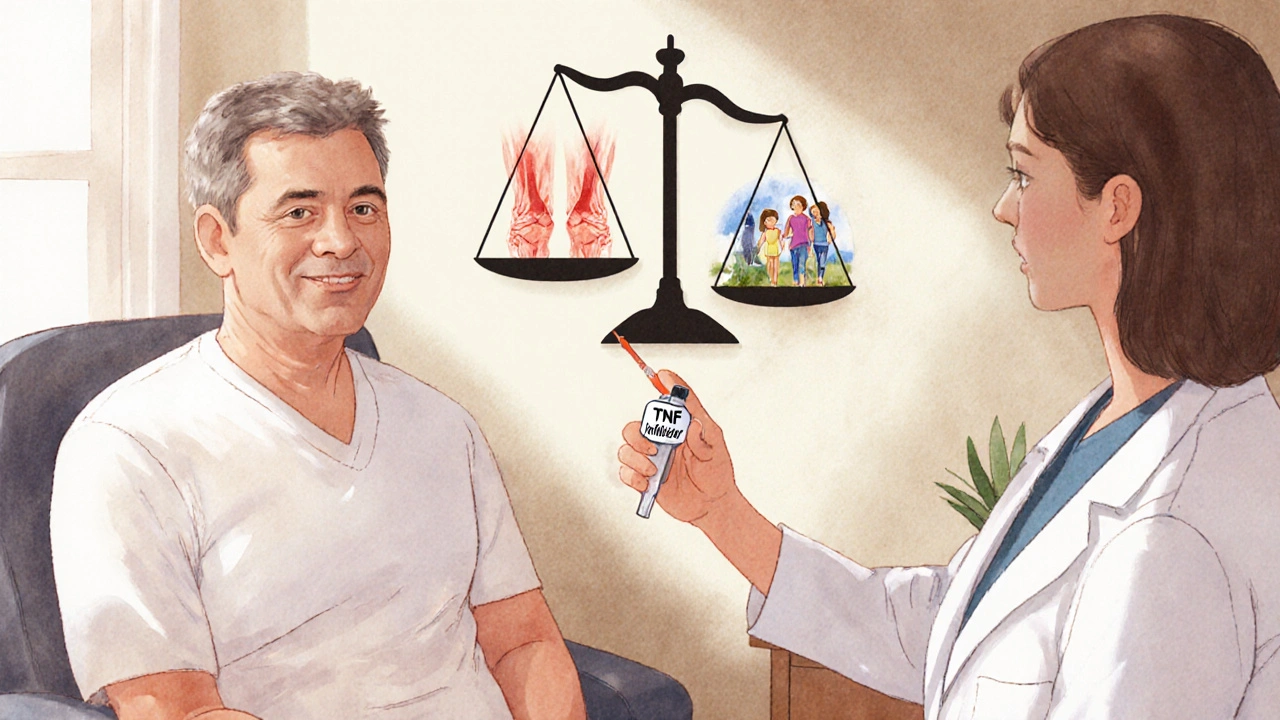
When you’re living with rheumatoid arthritis, psoriatic arthritis, or Crohn’s disease, the daily pain and fatigue can feel unbearable. For many, TNF inhibitors are the turning point - the treatment that finally brings relief. But with that relief comes a question that keeps people up at night: Does this drug increase my risk of cancer? It’s not a fear you should ignore. It’s a risk you need to understand - clearly, honestly, and without hype.
What Are TNF Inhibitors, and How Do They Work?
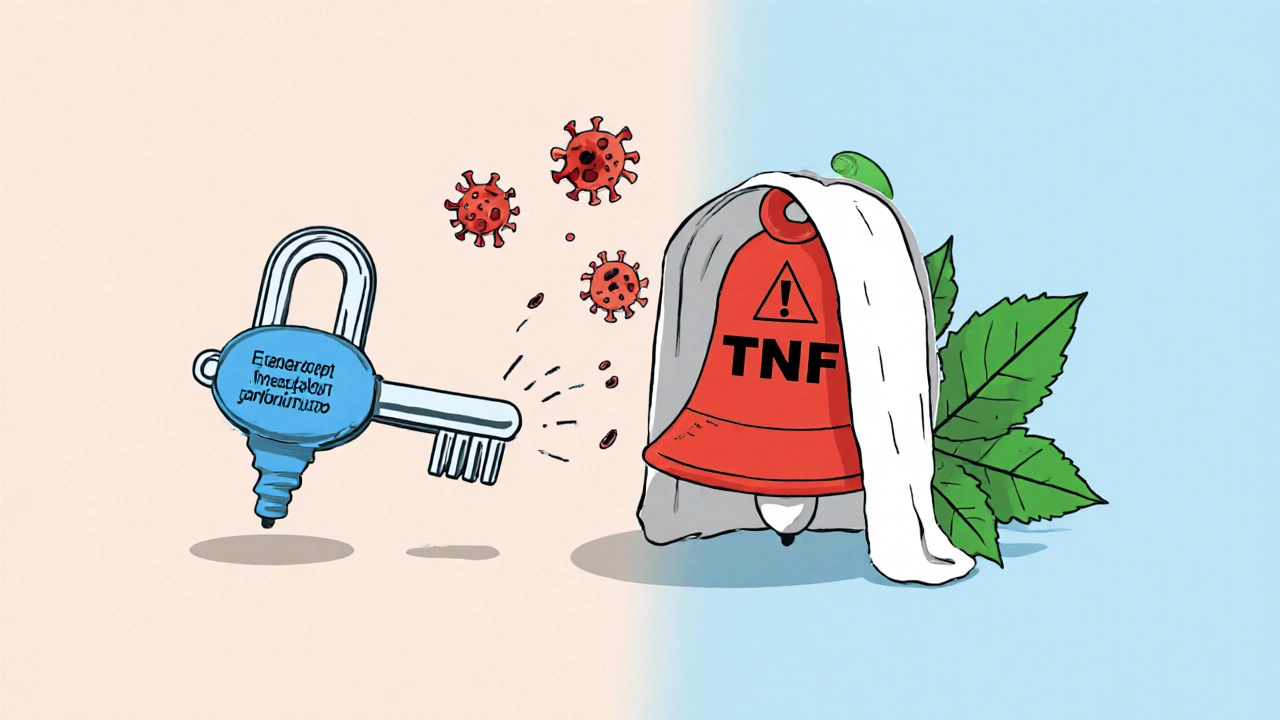
TNF inhibitors are a type of biologic drug designed to block tumor necrosis factor-alpha (TNF-α), a protein that drives inflammation in autoimmune diseases. Think of TNF-α like a faulty alarm system in your body - it’s screaming "attack!" even when there’s no real threat. These drugs quiet that alarm. They don’t cure the disease, but they stop it from tearing through your joints, skin, or gut.
Five TNF inhibitors are approved in the U.S.: infliximab, etanercept, adalimumab, certolizumab pegol, and golimumab. They’re given by injection or IV, and most are taken weekly or every few weeks. They’ve been around since the late 1990s, and over 1.5 million Americans are on them right now. For many, they mean the difference between being housebound and playing with their grandkids.
The Cancer Risk Debate: What the Data Actually Shows
The scary headlines say biologics cause cancer. The science says something more complicated.
A 2022 study tracking over 15,000 rheumatoid arthritis patients in Sweden found no overall increase in cancer risk from TNF inhibitors compared to older, non-biologic drugs. That’s huge. But it didn’t tell the whole story. When researchers looked closer, they found something odd: adalimumab showed a slight spike in cancer diagnoses during the first year of treatment. Not because it caused cancer - but because people who already had undiagnosed cancer were more likely to start the drug. That’s called "protopathic bias." It’s not the drug causing cancer; it’s cancer causing the need for the drug.
Meanwhile, etanercept consistently showed no increased risk - and in some studies, even a slightly lower risk than patients on older medications. Why? It’s not fully clear, but its different molecular structure may play a role. Etanercept binds TNF differently than monoclonal antibodies like adalimumab or infliximab. That small difference might matter more than we thought.
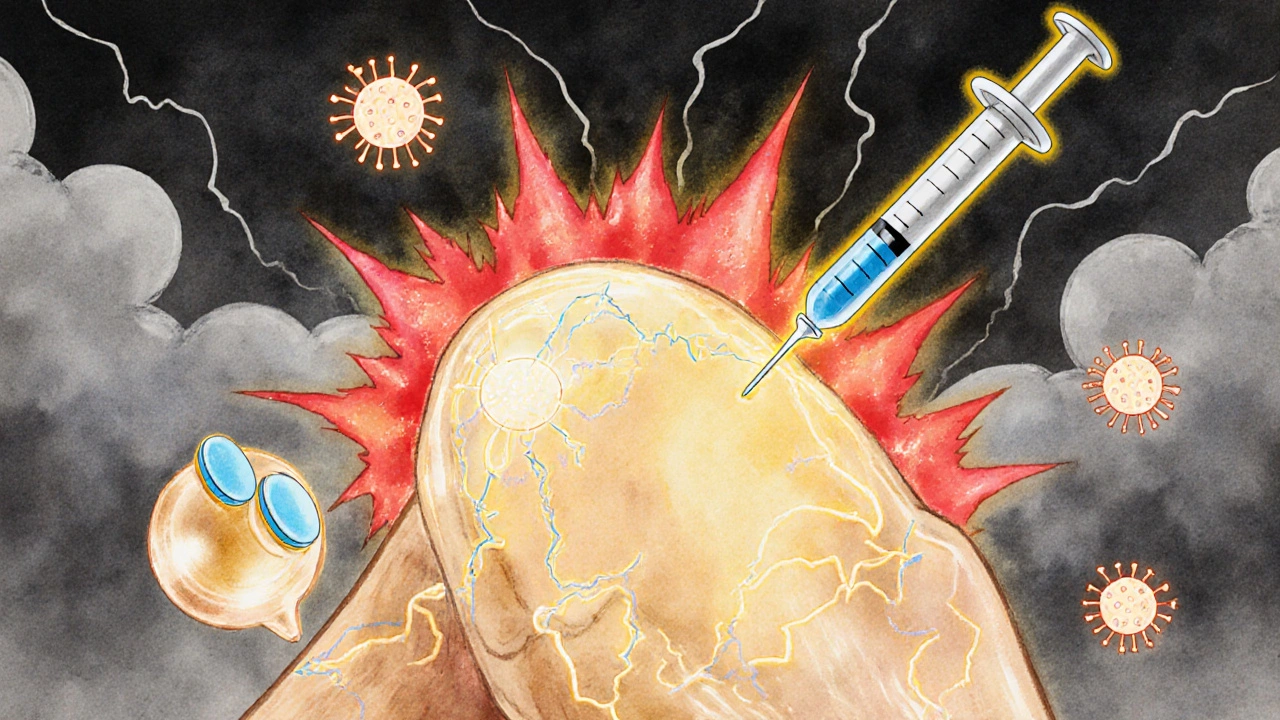
One area where risk is real: non-melanoma skin cancer. Multiple studies show a 30% higher chance of basal cell or squamous cell carcinoma in patients on TNF inhibitors, especially adalimumab. That’s not a huge jump - but it’s enough to matter. If you’re on one of these drugs, you need to see a dermatologist every 6 to 12 months. A simple skin check can catch these cancers early, when they’re almost always curable.
What About Other Cancers?
For lymphoma, the FDA added a black box warning in 2008. That warning was based on early case reports and small studies. But bigger, longer-term data - like the 20-year follow-up from the Annals of the Rheumatic Diseases - shows no rising trend in lymphoma risk over time. The absolute risk remains very low: less than 1 in 1,000 patients per year.
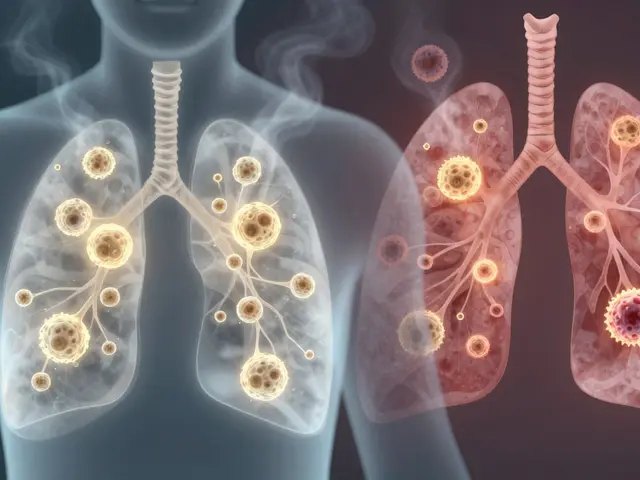
What about lung, breast, or colon cancer? The data here is surprisingly reassuring. A 2023 study of 1,872 cancer patients with rheumatoid arthritis found those on TNF inhibitors had better survival rates after lung cancer diagnosis than those on older drugs. That doesn’t mean TNF inhibitors prevent cancer. It means they don’t make it worse - and might even help the body respond better to treatment.
Here’s the kicker: patients on high-dose steroids (7.5 mg or more of prednisone daily) had much worse cancer outcomes than those on TNF inhibitors alone. That’s important. Sometimes, it’s not the biologic causing the problem - it’s the steroid you’re taking alongside it.
Real People, Real Choices
On Reddit, a woman named Lisa wrote: "I was terrified to start Humira. My cousin died of lymphoma. But my joints were breaking. I couldn’t hold my baby. I started it anyway. Two years later - no cancer. Just less pain."
Another patient, Mark, had a basal cell carcinoma removed while on adalimumab. His dermatologist told him to keep going. "It was caught early," he said. "They didn’t even need chemo. Just a cut and stitch."
But not everyone feels safe. One survey found 63% of psoriasis patients on TNF inhibitors worry about skin cancer. That’s understandable. The fear is real. But the data shows: if you get screened, you’re not gambling. You’re managing risk.
What Should You Do Before Starting?
Before you take your first dose, your rheumatologist should do a few things:
- Check your skin for suspicious moles or lesions - and refer you to a dermatologist if needed.
- Ask about your personal and family cancer history.
- Review any past cancer treatments. If you had melanoma or lymphoma, most doctors will wait at least 5 years before starting a TNF inhibitor. For breast or prostate cancer, 2 years is often enough.
- Run a TB test. These drugs can wake up dormant tuberculosis.
- Discuss alternatives. If you’re young and have mild disease, maybe a JAK inhibitor or IL-17 blocker is a better fit.
And here’s something most patients don’t know: your doctor should spend at least 12 minutes talking to you about cancer risk. That’s not just paperwork. That’s informed consent.
What Happens If You Already Had Cancer?
This is where things get personal. If you’ve had cancer, you’re not automatically off the table.
A 2023 registry study found that 87% of rheumatologists continue TNF inhibitors in patients with early-stage, low-risk cancers - like Stage I breast cancer or localized prostate cancer - after getting clearance from an oncologist. And 92% of those patients had no cancer recurrence linked to the drug.
But timing matters. You need to be cancer-free for a while. For aggressive cancers like melanoma or lymphoma, wait 5 years. For slower ones, 2 years is often enough. And you need to be monitored closely - every 3 to 6 months - for the first few years after restarting.
One patient, Diane, had Stage I breast cancer. She stopped her TNF inhibitor during treatment. After surgery and radiation, she waited 2 years. Then, with her oncologist’s approval, she restarted. "I thought I’d be in pain forever," she said. "But I got my life back."

The Bigger Picture: Biologics Are Not All the Same
Not all biologics are created equal. TNF inhibitors are just one class. Newer drugs - like JAK inhibitors (tofacitinib, baricitinib) and IL-17 blockers (secukinumab, ixekizumab) - are gaining ground. Some of these may have different risk profiles.
But here’s what the data says: TNF inhibitors have the longest safety track record. Over 25 years of real-world use. More than 10 million patient-years of data. That’s more than any other biologic class.
And while newer drugs might be more convenient or cheaper, they don’t yet have the same depth of evidence when it comes to long-term cancer risk. If you’re choosing between a TNF inhibitor and a newer drug, the decision isn’t just about cost or dosing. It’s about how much we know - and how long we’ve been watching.
Bottom Line: Risk Is Real - But Manageable
Yes, TNF inhibitors carry a small increased risk of skin cancer. Yes, there’s a theoretical risk of lymphoma. But the evidence doesn’t support the fear that these drugs cause cancer in healthy people.
The real danger isn’t the drug. It’s not getting treated. Untreated rheumatoid arthritis increases your risk of heart disease, lung problems, and yes - even cancer. Chronic inflammation is a cancer promoter. Suppressing it might actually protect you.
What you need is a plan:
- Get screened for skin cancer before you start.
- Stick to your dermatology appointments.
- Don’t skip your TB test.
- Talk to your oncologist if you’ve had cancer.
- Keep your steroid dose as low as possible.
- Know that etanercept may be safer than adalimumab for skin cancer.
These drugs aren’t magic. But for millions, they’re the only thing that lets them live normally. The key isn’t avoiding risk - it’s managing it. With the right checks, the right monitoring, and the right doctor, you can take control - not just of your disease, but of your future.
Do TNF inhibitors cause cancer?
No, TNF inhibitors don’t directly cause cancer in most people. Large, long-term studies show no overall increase in cancer risk compared to older arthritis drugs. However, there is a small increased risk of non-melanoma skin cancer - especially with adalimumab - and a very low risk of lymphoma. Most of the early cancer cases seen in patients were likely undiagnosed before treatment started, not caused by the drug.
Is adalimumab riskier than etanercept for cancer?
Yes, for non-melanoma skin cancer, adalimumab carries about a 30% higher risk than etanercept. Studies also show a slight spike in early cancer diagnoses with adalimumab, likely because patients with hidden cancers are more likely to be prescribed it. Etanercept has consistently shown lower or neutral cancer risk in large studies. If skin cancer is a concern, etanercept may be the safer choice.
Can I take TNF inhibitors if I’ve had cancer before?
Yes, in many cases. If you had a low-risk cancer like breast or prostate cancer and have been cancer-free for at least 2 years, most rheumatologists will restart a TNF inhibitor after consulting your oncologist. For high-risk cancers like melanoma or lymphoma, the waiting period is usually 5 years. The key is coordination between your rheumatologist and oncologist - and close monitoring after restarting.
Do I need skin checks while on TNF inhibitors?
Absolutely. All patients on TNF inhibitors should have a full-body skin exam by a dermatologist before starting treatment and then every 6 to 12 months. Non-melanoma skin cancers are common in this group - but they’re highly curable if caught early. Don’t skip these appointments. They’re simple, quick, and potentially life-saving.
Are biologics safer than steroids for cancer risk?
Yes, generally. High-dose steroids (7.5 mg or more of prednisone daily) are linked to worse outcomes in cancer patients - including higher death rates. TNF inhibitors don’t carry that same risk. In fact, some studies show better cancer survival in patients on TNF inhibitors compared to those on high-dose steroids. Reducing steroid use is often a key goal when starting biologics.
What’s Next?
The future of TNF inhibitors isn’t about stopping them - it’s about personalizing them. By 2027, doctors may use genetic tests to identify patients who are at higher risk for lymphoma before even starting treatment. That’s not science fiction. It’s already being tested in research labs.
For now, the message is clear: if you need a TNF inhibitor, don’t let fear stop you. But don’t ignore the risks either. Get screened. Stay on top of your skin checks. Talk to your doctors. And remember - the biggest threat isn’t the drug. It’s letting inflammation go unchecked.









11 Comments
I started Humira last year after years of joint pain that made holding my cat feel like torture. I was terrified, too-my aunt had lymphoma, and I swore I’d never touch biologics. But after six months? I’m hiking again. No cancer. Just less pain. I get skin checks every 6 months. It’s not perfect, but it’s better than crying in the shower every morning.
Let’s be real-this whole article reads like a pharma-funded pamphlet. TNF inhibitors don’t cause cancer? Sure, buddy. And cigarettes don’t cause lung cancer. The data is skewed because they only track people who survive long enough to be counted. Meanwhile, my cousin got squamous cell carcinoma on his nose at 38 after two years on adalimumab. He’s fine now, but that doesn’t mean the drug didn’t help push it over the edge. Wake up.
It is imperative that we recognize the profound implications of immunosuppressive therapy in the context of oncological risk. While the data presented may appear reassuring, the underlying biological mechanisms remain incompletely understood. The notion that etanercept is inherently safer than adalimumab is not empirically validated across all populations. One must consider genetic polymorphisms, metabolic clearance rates, and concomitant medication use. This is not a decision to be made lightly.
I read this whole thing and I’m still not sure if I should take it or not. Like, I get that the stats say it’s low risk, but what if I’m the one in a thousand? And why do they keep saying "it’s not the drug, it’s the inflammation" like that’s supposed to make me feel better? I’ve got a 10-year-old daughter. What if I get cancer and she has to watch me fade away? That’s not a risk I can just "manage." Also, why does everyone keep saying "skin checks" like it’s a spa day? I hate doctors. I hate needles. I hate being told what to do. I just want to feel normal.
Listen. I’ve been on etanercept for 11 years. I’ve had two basal cell carcinomas removed-both caught early. My dermatologist says I’m lucky. I’m not lucky. I’m careful. I wear sunscreen every damn day, even in winter. I don’t skip appointments. I don’t ignore weird moles. And I didn’t let fear silence me. If you’re scared, that’s okay. But don’t let it make you passive. Get checked. Stay informed. Fight for your life-not against the drug, but for your health. You’ve got this.
So let me get this straight. The drug might cause cancer, but not really. It’s probably just the cancer that was already there. But also, it definitely causes skin cancer. But it’s fine because we can just cut it off. And we’re supposed to be grateful? Cool. I’ll just keep taking prednisone and pretending I’m not turning into a pufferfish.
According to the 2022 Swedish cohort study, the hazard ratio for overall malignancy was 0.98 (95% CI: 0.89–1.08), indicating no statistically significant increase. However, for non-melanoma skin cancer, the adjusted HR was 1.31 (95% CI: 1.12–1.53), with a dose-dependent trend observed for adalimumab. The protopathic bias hypothesis is supported by temporal clustering of cancer diagnoses within the first 12 months, particularly in patients with elevated CRP and ESR prior to initiation. The differential safety profile between etanercept and monoclonal antibody TNF inhibitors may relate to Fc-mediated effector functions.
Here’s the thing no one says out loud: we’re all just guessing. We’re taking drugs that shut down part of our immune system, and we’re told to trust the numbers. But numbers don’t live with the fear. Numbers don’t stare at their skin in the mirror and wonder if that spot is the one. Maybe the real question isn’t whether TNF inhibitors cause cancer-it’s whether we’ve built a medical system that makes people feel like they have to gamble their future just to walk without pain. And if that’s the case… who’s really responsible?
Oh wow, so adalimumab is the villain now? Let me guess-next they’ll say it’s because of the preservatives, or the manufacturing plant in Ireland, or the fact that it’s made by AbbVie. This isn’t science, it’s fearmongering with footnotes. Etanercept is safer? Maybe. Or maybe it’s just less popular, so fewer people notice the side effects. And what about the 10% of patients who don’t respond to etanercept? Do they just die of inflammation? Stop cherry-picking data and start treating patients.
I’m from Texas. We don’t cower from cancer. We stare it down. I’ve been on Humira for 7 years. I’ve had two skin cancers removed. I’ve got a scar on my neck and a doctor who knows my name. I’m not a statistic. I’m a survivor. And if you’re scared? Good. That means you’re alive. Now go get checked. Don’t let fear write your story. You’re stronger than this drug.
Before initiating any biologic therapy, it is essential to conduct a comprehensive risk-benefit analysis, incorporating patient-specific variables such as age, comorbidities, prior malignancy history, and genetic predisposition (e.g., BRCA, Lynch syndrome). Furthermore, longitudinal monitoring protocols-including dermatologic surveillance, CBC with differential, and inflammatory marker trends-must be standardized across clinical practices. The differential pharmacokinetics of etanercept versus monoclonal antibodies necessitate individualized treatment algorithms, not population-based generalizations. Patient autonomy must be preserved through transparent, time-intensive counseling.