After a heart attack or heart surgery, your body needs more than just time to heal-it needs a clear, safe, and supported plan to get stronger. Many people assume rest is the best medicine, but that’s not true anymore. In fact, moving too little can actually hurt your recovery. Cardiac rehabilitation is the proven, science-backed way to rebuild your heart health after a major cardiac event. It’s not just about exercise. It’s about learning how to live differently so your heart stays strong for years to come.
What Exactly Is Cardiac Rehabilitation?
Cardiac rehabilitation is a medically supervised program designed for people who’ve had a heart attack, bypass surgery, stent placement, valve replacement, or other serious heart conditions. It’s not a luxury or an optional add-on. It’s a core part of treatment, just like medication or surgery. The American Heart Association calls it one of the most effective tools in cardiovascular care-and yet, fewer than 4 in 10 eligible patients actually join one.
The program isn’t a one-size-fits-all. It’s built around your needs, your limits, and your goals. It has three clear phases, each with its own focus and timeline. And it’s not just about physical activity. It includes education, emotional support, and ongoing monitoring to make sure you’re healing safely.
Phase I: Starting Right in the Hospital
Rehab doesn’t wait until you leave the hospital. It starts within 24 to 48 hours after your heart event. This is Phase I. Your care team will get you up and moving-slowly, safely, and with constant monitoring.
Early movement might sound scary, but it’s safer than staying in bed. You’ll start with simple tasks: sitting up in bed, standing for a few minutes, walking to the bathroom. These sessions last only 3 to 5 minutes at first, with breaks in between. By the third day, you’ll likely be walking short hallways-totaling about 20 minutes of activity per day.
Your heart rate is closely watched. You shouldn’t push past 120 beats per minute, or your resting heart rate plus 20. You’ll also be asked to rate how hard you feel you’re working using the Borg scale. A score of 12 or 13 out of 20 means you’re working at just the right level-enough to help, not enough to strain.
This phase isn’t just about movement. You’ll also learn warning signs to watch for: chest pain, dizziness, extreme shortness of breath. If you feel any of these, you stop. And you tell someone immediately.
Phase II: Outpatient Recovery-The Heart of the Program
Once you’re discharged, you’ll move into Phase II. This is the most structured part of rehab. It usually starts 1 to 3 weeks after leaving the hospital and lasts about 12 weeks.
You’ll attend 36 supervised sessions, typically three to five days a week. Each session is one hour long and includes:
- Warm-up (5 minutes)
- Main aerobic exercise (30-40 minutes): walking on a treadmill, cycling on a stationary bike, or using an arm ergometer
- Strength training (10-15 minutes): light weights or resistance bands for major muscle groups
- Cool-down (5 minutes)
The goal? Build endurance without overdoing it. You’ll work at 40% to 59% of your heart rate reserve-roughly 60% to 75% of your maximum predicted heart rate. On the Borg scale, aim for 11 to 13. That’s the sweet spot: you’re breathing harder than usual, but you can still talk in short sentences.
Strength training isn’t optional. Lifting light weights (10-15 reps, 2-3 times a week) helps you do daily tasks without getting winded. Start with weights you can lift easily. Don’t hold your breath. Exhale when you lift, inhale when you lower. This prevents dangerous spikes in blood pressure.
By the end of Phase II, most people see big improvements: a 15% increase in oxygen use during exercise, a 40% boost in metabolic capacity, and a 10% longer 6-minute walk. These aren’t just numbers-they mean you can climb stairs without stopping, carry groceries, or play with your grandkids without fear.

Phase III: Lifelong Maintenance
Phase III is where you take control. There’s no more scheduled group sessions. Instead, you continue on your own, using what you’ve learned. The goal? Stay active every day.
World Health Organization guidelines recommend at least 150 minutes of moderate-intensity aerobic activity per week. That’s 30 minutes, five days a week. You can break it into 10-minute chunks if needed. Walking, swimming, cycling-anything that gets your heart pumping is fine.
Keep doing strength training twice a week. Keep checking your heart rate. Keep using the Borg scale. If you’re unsure whether you’re working too hard, ask yourself: Can I sing a song? If yes, you’re too easy. Can you barely speak? Then you’re pushing too hard. The right pace lets you talk, but not sing.
Many programs offer follow-up check-ins every few months. Some even use wearable tech to track your heart rate and activity remotely. This helps your care team spot problems early.
Who Can Benefit?
Cardiac rehab isn’t just for people who’ve had a heart attack. It’s recommended for anyone with:
- Heart attack within the last 12 months
- Coronary artery bypass surgery
- Stent placement or angioplasty
- Heart valve repair or replacement
- Heart or lung transplant
- Stable angina
- Chronic heart failure
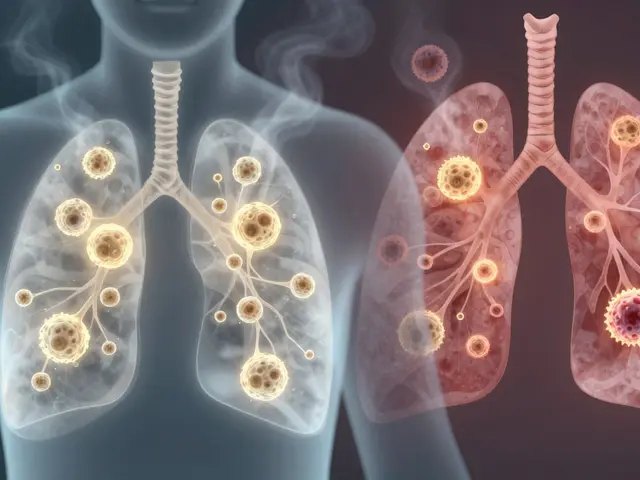
Even if you don’t have symptoms, having blocked arteries or a weakened heart muscle means you’re at risk. Rehab helps you manage that risk. It’s also helpful for people with peripheral artery disease-when arteries in the legs narrow and cause pain when walking.
But it’s not for everyone. If you have unstable angina, uncontrolled arrhythmias, severe aortic stenosis, or active heart inflammation, rehab may be delayed until your condition stabilizes. Your doctor will decide when you’re ready.
Why So Few People Join
Despite all the evidence, only about 37% of eligible Medicare patients enroll in cardiac rehab. That’s a huge gap. Why?
- Doctors don’t always refer patients-only 69% of eligible people get a referral.
- Transportation is a problem, especially in rural areas.
- People think it’s too expensive, but Medicare covers 36 sessions with just a 20% copay.
- Some believe they’re too old, too weak, or that exercise is dangerous after a heart event.
The truth? Cardiac rehab is safer than driving to the store. Studies show only 1 serious complication per 100,000 hours of exercise. That’s less risky than falling in the shower.
And the results? People who complete rehab are 26% less likely to die from heart disease and 18% less likely to be hospitalized again. That’s not just better health-it’s more time with family, more independence, and more life.

What About Mental Health?
After a heart event, it’s common to feel anxious, depressed, or overwhelmed. Up to 40% of patients experience these feelings. Rehab programs now include counseling and mental health support because emotional health is part of heart health.
Group sessions help you connect with others who understand what you’re going through. Talking about fear, guilt, or anger isn’t weakness-it’s part of healing.
If you’re feeling down, don’t wait. Tell your rehab team. There are proven therapies and medications that work. Your heart doesn’t heal in isolation.
What You Can Do Right Now
If you or a loved one had a heart attack or surgery:
- Ask your doctor for a referral to cardiac rehab. Don’t wait.
- If they say no, ask why. If it’s because of transportation, ask about telehealth options.
- Start walking today-even 5 minutes counts. Build up slowly.
- Stop smoking. If you need help, rehab programs offer support.
- Follow your diet plan. Reduce salt, sugar, and processed foods.
- Take your meds. Don’t skip them because you feel better.
Cardiac rehab isn’t a finish line. It’s the start of a new way of living. It’s not about going back to how you were before. It’s about becoming stronger, healthier, and more confident than ever.
What’s Next?
The future of cardiac rehab is personal. Wearable devices track your heart rate and activity in real time. AI helps adjust your plan based on your daily progress. Telehealth lets you join sessions from home. Mental health support is becoming standard. These changes are making rehab more accessible, more effective, and more human.
But the biggest change? You. You showing up. You taking the first step. You choosing to fight for your heart.
Is cardiac rehab safe after a heart attack?
Yes, it’s extremely safe. Studies show only 1 serious complication per 100,000 hours of supervised exercise. That’s safer than many everyday activities. Your heart rate, blood pressure, and symptoms are monitored throughout every session.
How long does cardiac rehab last?
Phase II, the core supervised program, lasts about 12 weeks with 36 sessions. Phase I starts in the hospital and lasts a few days. Phase III is lifelong-you keep exercising and managing your health after the formal program ends.
Can I do cardiac rehab at home?
Yes. Many programs now offer telehealth options with remote monitoring. You can do aerobic exercise at home, track your heart rate with a wearable, and check in with your team via video. But starting with in-person sessions is recommended for safety and guidance.
Does insurance cover cardiac rehab?
Yes. Medicare covers 36 sessions for eligible patients after a heart attack, bypass surgery, or other qualifying events. Most private insurers also cover it. You’ll pay a 20% coinsurance after meeting your deductible.
What if I’m too weak to start exercising?
You don’t have to be strong to start. Phase I begins with sitting up and standing. Even short walks in the hospital are part of rehab. Your team will tailor everything to your current ability. Progress is measured in small steps-like walking from the bed to the bathroom without stopping.
Can cardiac rehab help me live longer?
Absolutely. People who complete cardiac rehab reduce their risk of dying from heart disease by 26% and lower their chance of being hospitalized again by 18%. It’s one of the most effective ways to extend your life after a heart event.








5 Comments
After my bypass, I was scared to move. My nurse told me to sit up for 3 minutes. I thought I’d die. But I didn’t. By day 3, I walked to the bathroom without help. Cardiac rehab saved my life. It’s not magic-it’s science. And it works.
Don’t wait until you’re ‘ready.’ You’re never ready. You just start.
Phase I isn’t about fitness. It’s about proving to your brain that your heart still works.
I cried the first time I walked down the hall. Not from pain-from pride.
And yeah, the Borg scale? I still use it. 12-13 is the sweet spot. If you’re gasping, you’re going too hard. If you’re humming, you’re not going hard enough.
My doc said 36 sessions. I did 38. Worth every minute.
Oh great. Another corporate wellness cult. Next they’ll tell us to meditate with our stents and drink kale smoothies while listening to binaural beats.
Cardiac rehab? More like cardiac propaganda. You think your heart needs a schedule? It’s a muscle, not a spreadsheet.
My uncle had a heart attack in ‘87. Didn’t do rehab. Lived to 89. Played golf every Sunday. Drank whiskey with his meds.
Modern medicine is just capitalism with a stethoscope.
Also, ‘150 minutes a week’? Who made that up? Some guy in a lab who’s never held a shovel?
Let me guess-this whole rehab thing is pushed by Big Pharma and the treadmill industry.
They don’t want you to heal naturally. They want you dependent. 36 sessions? That’s 36 chances to upsell you on supplements, wearables, and ‘heart-healthy’ meal plans that cost $12 a bagel.
And who monitors you? Some guy with a clipboard who’s paid by the hospital? What if he’s asleep? What if the machine glitches?
My neighbor did rehab. Got a new pacemaker six months later. Coincidence? I think not.
Also-why is the Borg scale even a thing? Who named that? Sounds like a sci-fi villain.
My heart doesn’t need a rating system. It needs peace. And silence. And no more machines beeping at 3 a.m.
Look, I get it. You want us to ‘get moving.’ But this isn’t Europe. We don’t have time for group therapy and walking circles on treadmills.
Back in my day, you got up, you worked, you ate, you slept. No one handed you a schedule. No one told you your heart rate was ‘too high.’
Now we’re told to count steps like it’s a video game. ‘You’ve reached 7,000 steps! Good job, soldier!’
What’s next? Heart-healthy emojis?
And don’t get me started on ‘telehealth.’ You want me to do cardiac rehab from my couch while watching Netflix? That’s not rehab. That’s surrender.
We used to be tougher. Now we’re just… fragile.
Y’all need to stop overthinking this.
Start walking. Even if it’s 5 minutes. Even if you’re tired. Even if you’re scared.
I did rehab after my stent. I cried in the first session. My legs shook. My heart felt like it was gonna explode.
But I kept going.
Now I hike on weekends. I carry my grandkids. I cook for my family. I don’t think about my heart anymore-because it’s not the enemy.
You don’t need to be perfect. You just need to show up.
And if your doc didn’t refer you? Ask again. And again. And again.
You deserve this. Not because you’re ‘sick.’ But because you’re alive.
And you’re worth the effort.